|
Table of Content - Volume 19 Issue 3 - September 2021
Correlation of MRI findings with arthroscopic findings in internal derangement of knee
Bharati Deokar-Sharma1, Shreerang Joshi2*, Kalpit Dhotkar3, Akshay Bondar4, Rohan Nagare4, Piyush Gaikwad5, Suyash Ingale6
1Associate Professor, 2Professor & HOD, 3Senior Resident, 4,5,6Junior Resident. B.K.L. Walawalkar Rural Medical College and Hospital, Sawarde, Ratnagiri, Maharashtra, INDIA. Email: joshishreerang@yahoo.in
Abstract Background: To study the MRI findings and Arthroscopic findings in all the knee joint injuries referred from Orthopedic OPD. To correlate the MRI findings with Arthroscopic findings to study their specificity and sensitivity in different knee injuries for appropriate diagnosis and management. Settings and Design: Retrospective study. Materials and Methods: 36 patients seen in B.K.L. Walawalkar Rural Medical College and Hospital between February 2021 to May 2021, clinically diagnosed to be having knee ligament/meniscus/osteochondral injury clinically underwent MRI followed by arthroscopy. MRI findings and arthroscopy findings were compared and sensitivity, specificity, PPV, NPV, accuracy, kappa and P value for each injury was calculated. Statistical Analysis: Descriptive statistics using Chi square test and predictive values was done. Results: The sensitivity, specificity, PPV, NPV, accuracy, kappa, p value was calculated (in %). For ACL it was 92, 81.8, 92, 81.8, 88.8, 0.737 and 0.001, for PCL it was 100, 100, 100, 100, 100, 1, 0.0238, for MM 81.8, 64, 50, 88.8, 69.4, 0.323 and 0.0488. For LM 66.6, 86.6, 50, 92.85, 83.3, 0.746 and 0.0001, for osteochondral defects 100, 100, 100, 100, 100, 1, 0.0238 respectively. Conclusion: MRI is most reliable in diagnosing posterior cruciate ligament injury and osteochondral defects followed by Medial meniscal injuries followed by lateral meniscus. Keywords: Anterior cruciate ligament, medial meniscus, Arthroscopy, Knee, Magnetic resonance imaging.
INTRODUCTION The knee joint is a common site of injury, mainly due to trauma, repetitive activities and sports activities. It is necessary to diagnose if injury results in fracture, ligament injury, meniscus injury or its a combination of injuries. Conventional radiography and Computerised Tomography (CT) are used to evaluate fracture patterns. Magnetic resonance imaging has a better soft tissue contrast and multi planar slice capability which has revolutionized and has become the ideal modality for imaging ligaments, meniscus and cartilage of the knee joint. Arthroscopy can be used in its dual mode either as diagnostic and/or as therapeutic tool.1 Most commonly MRI imaging is done to rule out injury to menisci, cruciate ligaments, collateral ligaments, articular cartilage, loose bodies, meniscal cysts and bony contusions. The term internal derangement was originated in 1784 by William Hey; it is now loosely applied to a variety of intra articular and extra articular disturbances, usually of traumatic origin, that interfere with the function of the joint. The structure that is "deranged" should be identified, which requires a keen sense of clinical judgement, radiographs, MRI, Arthroscopy, and at times, surgical exploration. Arthroscopy allows direct visualization of all intra-articular structures and thus provides a high level of accuracy for both diagnosis and treatment, which makes arthroscopy the gold standard for evaluation of internal disorders and other lesions of the knee2. However, arthroscopy constitutes a relatively expensive and invasive examination.3 Magnetic resonance imaging (MRI) is a non-invasive method with good soft tissue contrast, high spatial resolution, multi-parameter and multi-range imaging for the evaluation of knee lesions10. It can clearly display the injury site of the ACL, the extent of the damage, the degree of injury and the damage to the related structures. AIMS: To study the MRI findings and Arthroscopic findings in all the knee joint injuries referred from Orthopedic OPD. OBJECTIVES: To correlate the MRI findings with Arthroscopic findings to study their specificity and sensitivity in internal derangement of knee for appropriate diagnosis and management.
MATERIALS AND METHODS A retrospective study of 36 patients who came in B.K.L. Walawalkar rural medical college between February 2021 to May 2021, and were diagnosed clinically and confirmed by MRI to be having traumatic internal derangement of knee were included in the study. All patients underwent arthroscopy. All patients above 18 years of age with history of closed knee injury without associated fracture and willing for arthroscopy were included in the study. Patients < 18 years of age, patients with ferromagnetic implants, pacemakers, and aneurysm clips, open injuries, suspected tumors, diagnosed to be having inflammatory or infectious condition of knee were excluded. On admission, a detailed history including the mechanism of injury and the complaints of the patients were noted, along with a thorough clinical examination. MRI of affected limb was done. Imaging protocols: Patients were subjected to MRI after clinical evaluation according to the following protocols: Protocol: T l , STIR, PD Fat suppressed weighted sequences in coronal plane. T2, GRE, PD Fat suppressed weighted sequences in sagittal plane. T2, PD Fat suppressed weighted sequences in axial plane. T2 weighted sequences in oblique/sagittal plane. Interpretation of MRI Data: Anterior cruciate ligament tear: i) Absent ii) Present If present: Partial /Complete. Femoral attachment/ Mid substance/ Tibial attachment Posterior cruciate ligament tear: i) Absent ii) Present. If present: Partial /Complete: Femoral attachment/mid substance/tibial attachment. Medial meniscus tear: i)Absent ii) Present. If present: Anterior horn /Body/Posterior horn Horizontal /Vertical /Complex Lateral meniscus tear: i)Absent ii) Present. If present: Anterior horn /Body/Posterior horn Horizontal [Vertical /Complex. Associated Findings. MRI Diagnosis: Arthroscopy findings: All routine pre operative investigations were done prior to anesthesia fitness. Pre-operative anesthesia fitness was done. Patient was posted for planned operative knee arthroscopy procedure. Post-operative management included operated limb elevation, IV antibiotics for the first 2 days and then be shifted to oral antibiotics for 3 days. Anti-inflammatory and analgesics and other supportive drugs were given to all patients. Routinely Post-operative dressing of the surgical wound was done on 2nd and 5th day. Sutures were removed on 12th postoperative day. Patients were given Long Knee Brace when indicated. ARTHROSCOPIC SURGERY All the arthroscopic procedures were performed under spinal anaesthesia. Per Operative findings were documented in the operation theatre, which included the anatomical structure involved with the presence or absence of tears, its location, status of the articular cartilage and additional details when available. Arthroscopic examination of the knee: The knee was divided routinely into the following compartments for arthroscopic examination: 1. Suprapatellar pouch and patellofemoral joint. 2. Medial gutter.3 Medial compartment. 4. Intercondylar notch. 5. Posteromedial compartment. 6. Lateral compartment. 7.Lateral gutter and posterolateral compartment. After performing a thorough arthroscopy of the knee, the pathological lesion was identified and further surgery was carried out accordingly (partial/subtotal meniscectomy for tears, ACL reconstructions for ACL tears).
OBSERVATIONS AND RESULTSCarefully constructed drawings photographs and videos which were made to depict the pathological process as the operative procedure was performed were used.The composite data was tabulated and studied for correlation with MRI findings and grouped into four categories:
Statistical analysis was used to calculate the sensitivity, specificity, positive predictive value (PPV) and the negative predictive value (NPV), in order to assess the reliability of the MRI results.
METHOD OF ANALYSIS OF DATA Collected data was presented in the form of tables and diagrams. Sensitivity, specificity and predictive values were calculated. Data was analysed for the significant correlation between MRI knee and arthroscopic findings by kappa statistics.
Table 1: Interpretation of sensitivity
Table 2: Interpretation of Kappa Statistics
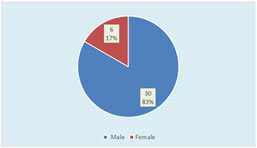
RESULTS SEX DISTRIBUTION In our study we had 36 patients, of which 30 were males and 06 were females. Table 3
Graph I: Sex wise number of cases Significant number of patients were males.
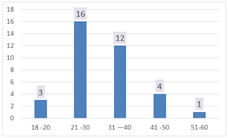
AGE DISTRIBUTION: The patients who suffered injury were with age ranging from 18 to 60 years.
Table 4
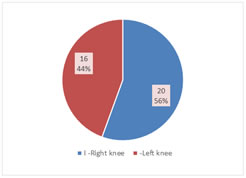
Graph 2: Age group wise Number of cases Maximum number of patients who suffered knee injuries were in the age group of 21-30 years. Table 5: Side involved
Graph 3: Number of cases The right knee joint was found to be more commonly involved than the left knee joint and there were no cases with bilateral knee involvement in our series.
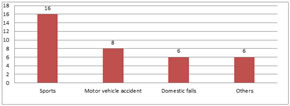
Table 6: Mode of injury
Graph 4: Mode of Injury Sports injury was the most common mode of injury.
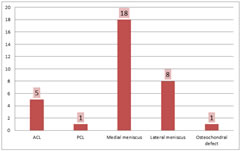
Table 7: Structures injured
Graph 5: No. of cases reported on MRI From the study we extracted the relevant data, we calculated true positive, true negative, false positive and false negatives values. The accuracy, sensitivity, specificity, negative predictive value (NPV), and positive predictive value (PPV) were calculated using the following equations, ppv = TP/(TP + FP), NPV IN/(TN + FN), sensitivity TP/(TP + FN), specificity = TN/(FP + TN) and accuracy (TP + + TN + FP + FN).
Table 8: Anterior cruciate ligament (ACL) tears
Sensitivity u- 92%. Specificity - 81.8%. Positive predictive value - 92%. Negative predictive value - 81.8%. Accuracy - 88.8%. Kappa - 0.737 — substantial. P value - 0.001 – significant. The sensitivity and specificity of MRI with respect to arthroscopy in ACL tear is 92% and 81.8%.
Table 9: Posterior Cruckate Ligament (PCL) tears
Sensitivity - 100%. Specificity - 100%. Positive predictive value - 100%. Negative predictive value- 100%. Accuracy - 100%. Kappa = I - almost perfect. P value - 0.0238 - significant
The sensitivity and specificity of MRI with respect to arthroscopy in PCL tear is 100% and 100% respectively. Table 10: Medial meniscus tears
Sensitivity - 81.8%. Specificity - 64%. Positive predictive value - 50%. Negative predictive value - 88.8%. Accuracy - 69.4%. Kappa = 0.323 – fair. P value - 0.0488 – significant. The sensitivity and specificity of MRI with respect to arthroscopy in MEDIAL MENISCAL tears was 81.8% and 64% respectively. Table 11: Lateral meniscus tears
Sensitivity — 66.6%. Specificity — 86.6%. Positive predictive value - 50%. Negative predictive value - 92.85%. Accuracy — 83.3%. Kappa = 0.746 — substantial. P value - 0.0001 - significant The sensitivity and specificity of MRI with respect to arthroscopy for LATERAL MENJSCAL tears is 66.6% and 86.6% respectively. Table 12: Osteochondral Defects
Sensitivity - 100%. Specificity - 100%. Positive predictive value - 100%. Negative predictive value - 100%. Accuracy - 100%. Kappa = I - almost perfect. P value - 0.0238 significant. The sensitivity and specificity of MRI with respect to arthroscopy in OSTEOCHONDRAL INJURIES is 100% and 100%. Table 13: Accuracy of MRI
DISCUSSIONIn the study of 36 patients, 30 were males and 06 were females. The age group ranging from 18 to 60 years. The youngest male patient was aged 18yrs and the oldest male was 45yrs and the youngest female was aged 34yrs and the oldest female was aged 58yrs. This showed that there was a tendency of males being injured and getting operated at the earlier age. A Study done by Fritz et al. showed males are most likely to suffer knee injuries since they are active in sports and the right knee was are more frequently injured than left. In the present study males comprise the predominant number of patients who suffered knee injuries who are actively involved in sports. Young patients of age group 20 - 30yrs are the maximum who suffered knee injuries. In our study 16 patients were falling in this age group comprising 44.5% of the patients. Right knee was involved in 20 cases and left was involved in 16 cases and no bilateral involvement. Meniscal tears were classed as torn or not torn. Anterior cruciate ligaments (ACL) and posterior cruciate ligaments were either completely torn or not. Any other knee pathologies including osteochondral defects, bone oedema and chondral lesions were grouped together as other pathology. False positives and false negatives MRI studies have higher false positive than false negative results. We also found this to be true when examining the combined results from meniscal lesions and ACL tears. Meniscal Injuries:Medial meniscus injury and lateral meniscus injury occurred with equal frequency. There were 14 medial menisci injuries and 14 lateral menisci injuries in this study. In our study MRI detected 18 cases of medial menisci injury, arthroscopy confirmed only 11 cases. Sensitivity and specificity of MRI with respect to Arthroscopy is 81.8% and 64% showing an average correlation with arthroscopy in diagnosing medial meniscal injuries. A study by Pappenport et al. showed accuracy rate of 90% for MRI in the detection of Meniscal tears compared with the arthroscopy. Elvenes et a15 in their study found the sensitivity, specificity, positive and negative value of MRI for medial meniscus tears were 100%, 77%, 71% and 100%. In the present study sensitivity, positive and negative predictive value are 81.8%, 64%, 50% and 88.8% respectively and did not correlate with the findings of above mentioned studies. Overall, MRI has a higher sensitivity (81.8%) than specificity (64%), and a higher NPV (88.8%) than the PPV (50%). In our study we found that sensitivity, specificity, positive and negative predictive value of MRI compared to arthroscopy was less compared to the other studies. In our study MRI detected 08 cases of lateral meniscal injury and arthroscopy positive cases are 06 out of 36 cases. Sensitivity and specificity of MRI in relation to Arthroscopy is 66.6% and 86.6%. It had a fair correlation with arthroscopy in diagnosing lateral meniscal injuries. Positive predictive value of MRI in detecting lateral meniscus injuries is 50% with negative predictive value of 92.85%. Overall, MRI has a higher specificity (86.6%) than sensitivity (66.6%), and a higher NPV (92.85) than the PPV (50%). Elvenes et al5 in their study found that sensitivity, specificity, positive and negative predictive value of MRI for MM were 100%, 77%, 71 % and 1000/0 respectively, while values for LM were 40%, 89%, 33 %, and 91% respectively. Overall accuracy of MRI for MM and LM combined was 84%. On basis of high negative predictive value, they concluded that MRI is useful to exclude patients from unnecessary arthroscopy. In our study MRI has a higher false positive i.e. high sensitivity and low detecting meniscal tears. If MRI is used as the only form of pre-operative screening for this condition, then there may well be unnecessary arthroscopies performed. False positive MRI scans seen in the posterior horn of the medial meniscus may reflect an inability to completely visualize the area. The occurrence of the false positive and false negative meniscal tears at MRI imaging has been noted earlier. There are explanations for this apparent discrepancy between findings at MR Imaging and arthroscopy Mink et. al.6
Some false positive findings on MRI can be attributed to inadequate visualization of the meniscus at surgery and to the fact that the diagnosis of a tear can be subjective. False positive MRI scans seen in the posterior horn of the medial meniscus may reflect an inability to completely visualize the area at arthroscopy, and tears that extend to the inferior surface of the meniscus may be difficult to see. Cruciate ligament lesions: Among the structure involved in knee injuries ACL injury is the most common accounting for 25 cases in MRI of which 2 were false positives and arthroscopy detected 23 of the 25 cases plus 2 new cases from the remaining (false negative of MRI). Sensitivity and Specificity of MRI with respect to Arthroscopy is 92% and 81.8% a fair correlation with arthroscopy in diagnosing ACL tears. Positive predictive value of MR is 92%. Negative predictive value of MRI is 81.8%. Out of 36 cases MRI detected 1 PCL injury which was confirmed by arthroscopy and hence Sensitivity, specificity and positive and negative predictive values remains at 100% and shows excellent correlation in detecting PCL injuries. PCL injuries are most commonly associated with chip fractures near the tibial attachment. MRI is accurate in identification of ACL tears, ranging from 93% to 97%. In one of our chronic IDK knee MRI shows ACL incompetence but intact fibers, however clinically patient had instability and at arthroscopy showed a chronic tear partially healed by fibrosis which was inefficient and required a reconstruction. The sensitivity and specificity in various studies have shown to range between 61% and 100%, and 82% and 97% respectively.7 in our study the PPV and negative predictive value was 92% and 81.8% respectively. The positive predictive value and negative predictive value range from to 76% and 70% to 100% respectively. 1 case of PCL tear was detected both by MRI and Arthroscopy. The use of MRI to identify PCL tears has proven to be extremely accurate. This might be expected in light of the fact that the PCL is usually very easily visualized as a homogenous, continuous low signal structure. Several studies have reported sensitivity, specificity, accuracy, positive predictive value and negative predictive value to be 99-100%.8 In our study too the sensitivity, specificity, accuracy, positive predictive value and negative predictive value was 100%.7 Articular cartilage injuries: Out at 36 cases of knee injuries MRI detected 1 case of Osteochondral defect and arthroscopy 1 case. Sensitivity of MRI is 100% with specificity of shows excellent correlation with Arthroscopy in diagnosing articular cartilage injuries. Positive predictive value of MRI is 100% with negative predictive value of 100%. The high accuracy of detection of Osteochondral defect in comparison with the mcniscal results is unusual. This might be explained because there were fewer cases available. The extent of cartilage abnormalities can be concealed when MRI is used as the only diagnostic tool. Arthroscopic evaluation is more useful than radiographs or MRI to grade osteoarthritis and assess surface cartilage abnormalities. There are studies that support the view that the diagnostic accuracy of the MRI could affect in a critical way the treatment pathway of knee injuries. MC Kenzie et al.9 have studied 332 patients' diagnosis before and after MRI. The diagnosis was initially based on the clinical examination and the therapeutic procedure was decided before MRI. 57 from 113 clinically positive before MRI meniscal tears were not confirmed with MRI. This result lead to revaluation and differentiation of treatment in 62 percent of the patients. From those patients programmed for surgery only 38 percent finally underwent arthroscopy. In another study, Weinstabl et al.10 randomly distributed patients with positive meniscus rupture tests in two groups. All the patients in the first group had MRI examination before arthroscopy. In this group only 2 percent of patients didn't have positive findings during arthroscopy. Second group patients underwent arthroscopy, based only to the findings of clinical examination. In this group, only in 30 percent of patients, arthroscopy confirmed the findings of clinical examination. The sensitivity for diagnosing isolated medial meniscal tears in Rubin's series11 was 98% and it decreased when other structures were also injured. The specificity in isolated lesions was 90%. In a multi centric analysis Fisher12 reported an accuracy of 78 to 97% for the anterior cruciate ligament and 64-95% for medial meniscus tears. The menisci are composed of fibrocartilage and appear as low signal structures on all pulse sequences. The sensitivity and specificity of MRI in detecting meniscal tears exceeds 90%.13 Ryan et al.14 in a prospective study of comparison of clinical examination, MRI, bone SPECT to detect meniscal tear reported high diagnostic ability of MRI along with bone SPECT to detect meniscal tears, with a sensitivity and specificity of 80% and 71% respectively. Simultaneous injury to several supporting structures is relatively common in the knee. When more than one lesion was present completely correct diagnosis was rendered only 30% of the time. This phenomenon was reported by Rubin11 In a prospective study reported by Imhoff et al., the negative predictive value was 94% but the positive Predictive value was only 54%. They concluded that due to a high negative predictive value, a normal MRI scan allows eliminating a meniscal lesion and so there is no need for a diagnostic arthroscopy. They suggested that due to low positive predictive value of MR. It should not be routinely used to confirm clinical diagnosis and its use should be limited to those cases where clinical examination is inconclusive. A diagnostic arthroscopy would be a better choice in those cases. However, in our study, MRI showed false results in significant proportion. For example as far as medial meniscus concerns there were 09 false positive and 02 false negative diagnosis whereas for lateral meniscus there were 04 false positive and 02 false negative diagnosis (PPV and 50%; NPV 88.8% and 92.85%; for medial meniscus and lateral meniscus tears respectively). There are several explanations for the misleading results of MRI regarding the menisci. Firstly, meniscal tears and meniscus degenerative changes have the same appearance in MRI, by giving high signals within the meniscus.15 Diagnosis then depends on the expansion of the high signal line towards meniscus articular surface16 Moreover, one of the most frequent causes for false positive MRI regarding the lateral meniscus is the misinterpretation of the signal coming from the inferior knee artery 17 Helman et a118 accredited in this structure about 38% of false positive MRI results. Often, the popliteal bursa or Humphreys' ligament may mimic posterior lateral meniscal tears as well.18,19 Mckenzie et a120 summarized the four most common reasons for false positive diagnosis:-
Disruption of the anterior cruciate ligament, a major stabilizer of the knee, leads to loss of stability of the knee and potentially significant dysfunction, although the ACL is the most frequently torn ligament of the knee; the ACL tear has remained clinically elusive. These injuries account for a large number of referral to hospitals. The evaluation of these lesions remains a difficult clinical problem. The MRI is a frequently used diagnostic modality for these internal derangements because of being non-invasive, painless and unassociated with risk of radiation. As far as the cruciate ligaments are concerned, our study showed that from the 25 ACL ruptures diagnosed during arthroscopy 02 of them were missed by the MRI; leading to NPV of MRI for ACL ruptures of 81.8%. Causes of that target loss are easily recognised; firstly; in cases with ligament ruptures without mucosum rupture, MRI gives false negative results. Additionally, ruptures near ligaments insertion may be missed and MRI examination reveals an intact ACL. On contrary, false positive ACL ruptures occur in cases of intrabody mucosal or eosinophilic degeneration of ACL.22,23 The accuracy, sensitivity and specificity values for knee lesions vary widely in literature. Rubin et a111 reported 93% sensitivity for diagnosing isolated ACL tears. Similarly several prospective studies have shown a sensitivity of 92-100% and specificity of 93-100% for the MR imaging diagnosis of ACL tears.12,24,25 The posterior cruciate ligament can be examined very well with MRI. Bibliography refers accuracy in ruptures higher than 90%.12,26,27 In our study we evaluated only 01 PCL rupture and it was identified by MRI (accuracy 100%; sensitivity 100%; specificity 100%). Even though our results agree with the bibliography data, the number of cases is too small for statistical significant conclusions. However, surgeons must always bear in mind that PCL is difficult to investigate during arthroscopy because of its anatomic position, and many times there are false negative results. In many cases, subchondral bone bruises that are frequently described in MRI, are mistaken with chondral defects, leading to false positive results. They remain though important cause of pain and morbidity. Additionally, one must never forget that pre operative MRI mainly focuses on meniscal and cruciate ligament injuries. As a result, Chondral lesions are often underestimated and misdiagnosed by MRI.28,29 Post operatively new examination with MRI that focus on chondral defects leads to improvement of the diagnostic results.28,29,30 Other authors however, like Heron et al.31 have shown that MRI can satisfactorily reveal the 2nd and 3rd grade chondral defects as well as damages at the patellar articular cartilage, but is not accurate for smaller injuries like fibrilization or small Assuring in articular hyaline cartilage. Similar results were reported from Ochi et al.30 who showed that the sensitivity of MRI increased (from 40%-71%) when MRI reading was done retrospectively, after the arthroscopic findings were registered. Especially, in chondral lesions with full thickness loss of cartilage and large deep erosions the retrospectively calculated MRI sensitivity was 100% and 75% respectively. On the other hand site surface injuries, fibrilization or shallow small cuts were not well described, not even post arthroscopically. Furthermore, according to Mori et al.29 usage of modern, improved techniques, can not only reveal the size of chondral lesions but to distinguish partial from full depth chondral damages as well. There is no doubt that the radiologist's experience and training are very important factors in interpretation of MRI. At the same time, reliable statistical data of the diagnostic value of the MRI are also related to the independent base of reference. Regarding knee MRI, in most of the studies and in our study as well, the base of reference is arthroscopy. This presupposes that arthroscopy is 100% accurate and allows for the diagnosis of every possible knee pathology. This is not always the case21,32. Arthroscopy is a technically demanding procedure and the results are varying according to surgeon's experience, especially in difficult cases. From the 15 false positive results of our study, the majority referred to posterior meniscus tear. Nevertheless, the belief is that, even in these cases, the meniscal pathology existed but failed to be discovered during arthroscopy.17,33 Especially the inferior surface of posterior aspect of the medial meniscus is difficult to be reached with a probe and often rupture at that point can be missed. Nowadays, the overall accuracy of arthroscopy varies between 70-100% depending on the surgeon's experience.21,34,35,36 This fluctuation inevitably raises questions regarding the reliability of MRI results classifications on true or false.20 In the everyday practice, based on clinical examination that comes first, surgeons decide whether must proceed to further laboratory tests, MRI, conservative or surgical treatment. But how precise can clinical examination be? There seems to be disagreement regarding the answer to this question. Investigations support that the accuracy of clinical examination compared with arthroscopic findings ranges between 64-85%.37,38 Rose et a123 found that clinical examination is as accurate as MRI in diagnosing meniscal tears and ACL ruptures, so they concluded that MRI because of its high cost is not necessary in patients with clinical suspicion of meniscus and cruciate ligament tears. Similar conclusion was reported by Boden et al.39 who supported that when clinical examination sets the diagnosis of meniscus damage, MRI will not change treatment decisions. On the Other hand, Ruwe et al.40 reported that preoperative MRI can prevent unnecessary arthroscopy in 50% of patients, so is of great value and must be done preoperatively. Boeree et a141 believe that clinical examination is of minor significance with sensitivity in diagnosing medial meniscus, lateral meniscus and ACL tear of 67 %, 48% and 55% respectively. Similar conclusions were reported by Jackson et a142 who concluded that negative MRI for meniscus and cruciate ligament tears can discourage diagnostic arthroscopy even if clinical examination is positive for injury.
CONCLUSION Knee joint injuries are common. The need to accurately evaluate the knee injuries is very crucial for the proper management and outcome otherwise it will lead to chronic debility to the patient. Magnetic resonance imaging (MRI) is of great aid in the diagnosis of knee lesions. Most diagnostic studies comparing MRI and arthroscopy have shown good diagnostic performance in detecting lesions of the menisci and cruciate ligaments. Nevertheless, arthroscopy has remained the reference standard for the diagnosis of internal derangements of the knee, against which alternative diagnostic modalities should be compared. Although MRI is being used with increasing frequency, it is unlikely to replace clinical diagnosis. It should be used in connection with clinical findings and history to provide a more complete picture, especially in complex injuries, as history and examination alone may be unreliable in less clinically evident situations, MRI still remains the only available means to diagnose in a acute/painful knees. Also it is difficult to assess the injury status and the severity in a multi ligamentous knee injuries by clinical methods alone. In these situations MRI becomes mandatory for the treating clinician. But in situations of chronic instabilities with clinically noticeable findings MRI may not be of significant value and hence can be avoided in clinically proven cases of knee instabilities. In conclusion, the present study supports that MRI is helpful in diagnosing meniscal and cruciate ligament injuries. Nowadays patients' expectations are maximal and taking into account that MRI false or misleading results can be as high as 20-30 percent in specific knee pathologies, it is concluded that arthroscopy still remains the gold standard in diagnosing the internal knee lesions. Undoubtedly new techniques and more tomograms will improve MRI's accuracy leading to better diagnostic accuracy in knee Injuries. In any case, what one must always have in mind is that diagnosis alone is not the end point of the treatment and does not solve the problem. It is the beginning of new thoughts and actions one must follow to achieve accurate prognosis and correct treatment. In order to plan and apply the correct treatment pathways, the most important is not the cost effectiveness or the statistical data. Clinical experience and adequacy of the surgeon always have the greatest values, when it comes to the assuring optimal treatment to the patient. Our study found that the accuracy of the MRI scan in diagnosing internal knee injuries is maximum in PCL and Osteochondral defects, followed by ACL and MENISCAL lesions. The routine use of MRI scan to confirm diagnosis is not indicated, as the positive predictive value of the scan is low for all lesions. In the presence of positive clinical signs, proceeding to arthroscopy is recommended. The negative predictive value of a scan was found to be high for all structures of the knee joint and hence a 'normal' scan can be used to exclude pathology, thus sparing patients from expensive and unnecessary surgery and also freeing up valuable theatre time. In this scenario the accurate and careful clinical examination remains the primary necessity in diagnosing internal knee injuries.
REFERENCES
Policy for Articles with Open Access
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home