|
Table of Content - Volume 19 Issue 3 - September 2021
A prospective study of functional outcome in extraarticular distal 3rd tibia fractures treated with intramedullary interlock nailing
Ranjeet Hakepatil1, Vijay Waghmare2*, Sandeep Kanthe3, Shreenivas Nalhe4
1,2,3,4Department of Orthopedics, Vilasrao Deshmukh Government Medical College, Latur, Maharashtra, INDIA. Email: drranjeet_hpatil@yahoo.com
Abstract Background: Distal tibial fractures are one of the most common long bone fractures encountered by orthopaedic surgeons in clinical practice. The best treatment for fractures of the distal tibia remains controversial. Most of these fractures require surgical fixation, but the outcomes are unpredictable and complications are common. The main aim is to assess the functional outcome of treatment of distal 3rd tibial fractures with intramedullary interlock nailing. Keywords: distal 3rd Tibia fracture, intramedullary nail, functional outcome
INTRODUCTION Tibia is the most common long bone to fracture owing to its subcutaneous nature and precarious soft tissue coverage especially in the distal one-third region.1 Distal tibia fractures without articular involvement are a common consequence of road traffic accidents or other high-energy injuries. These fractures differ from pilon fractures in terms of the mechanism of injury, management, and prognosis of the displaced bones. The proximity of these fractures to the ankle joint leads to more complications than are seen with diaphyseal or middle-third injuries. Thus, the treatment of distal tibia fractures remains problematic.2 Fractures of the lower third of the tibia are associated with an accompanying fibular fracture in about 85% of cases. These fractures are considered to be inherently unstable and frequently associated with complications like delayed union, malunion, soft tissue complications, and infection.1 Intramedullary nail fixation and plate internal fixation are the two mainstay treatments for tibial fractures, but agreement on the best internal fixation for distal tibial fractures is still controversial.3 Intramedullary nailing frequently results in malalignment, malunion, and knee pain. Tibia plating can achieve anatomic reduction, but it is associated with the risk of wound dehiscence and infection because of the minimal soft tissue cover over the anteromedial tibia.4The goals of surgical management include correction and maintenance of sagittal and coronal alignment, establishment of length and rotation, and early functional range of movements of knee and ankle.5 To avoid the complications associated with other methods of fixation, in these fractures we used an intramedullary cannulated tibial nail for fixation, utilizing the advantages of nailing. We evaluated the results and meantime of fracture union.6
METHODS This prospective study was conducted in a tertiary care center between June 2019-May 2020. A total of 64 patients were included in the study. Inclusion criteria: Age-patients between the age of 18yr to 60 yrs. of either sex who had to undergo nailing as the procedure of choice. Closed extraarticular fracture in distal 3rd tibial fracture according to AO/OTA Classification belonging to class 43A1,43A2,43A3. Fractures within 3cm to 10 cm from the joint line. Fresh injuries operated within 7 days of trauma. Exclusion criteria: Patients below age 18 and above age 60 years. Patients having open wounds. Intra-articular fracture AO/OTA classification: 43B,43C. Pathological fractures. Patients with addictions like smoking and alcoholism. Patients having neurovascular deficits. Follow-up was taken with radiographs at immediate post-op,6weeks,12 weeks,24 weeks, and 48 weeks. Olerud and Molander ankle score (OMAS) was used for functional assessment.
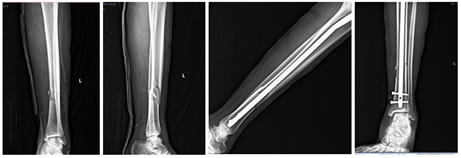
Figure 1: Pre and post operative x-rays of a patient with distal 3rd tibia fracture managed with interlock nail
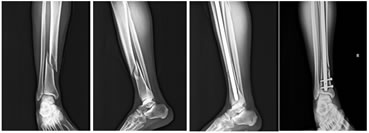
Figure 2: Pre and post operative x-rays of a patient with distal 3rd tibia fracture managed with interlock nail
Limb elevation was given postoperatively. Isotonic and isometric exercises were started on the same postoperative day. Postoperatively, antibiotics (ceftriaxone 1 gm. and amikacin 500mg) were given for 3 days. Patients were assessed clinically for wound infection, wound dehiscence, and ankle instability. Radiographs were taken on the immediate post-op day and then at 6 weeks,12weeks,24 weeks, and 48 weeks. Partial weight-bearing was allowed at 6-8 weeks and full weight-bearing at 12-14 weeks postoperatively depending upon the stability of fixation of the fracture.
RESULT Out of the total 64 patients, 46 (71.87%) were male patients and 18 (28.13%) were female patients. 39(60.93%) patients were operated for right-sided fracture and 25(39.07%) patients for left-sided fracture. Motor vehicle accident was a major mode of trauma in all cases except in 5 patients where 4 patients had a history of fall from height and 1 patient had trauma due to fall of heavy object on the leg. 29 patients were classified as 43A1 (45.31%).18 were classified as 43A2 (28.12%).17 were classified as 43A3(26.56%). In our study, the fibula was fractured in 51 patients (79.68%). Most of the fibular fractures were in the middle 1/3 rd region followed by the lower 3rd. Out of 19 lower third fibular fractures, 12 fractures were associated with ankle mortise instability and were fixed with intramedullary nails. The average time between injury and surgical fixation was 48 hours and the average duration of surgery was around 80 minutes. The average duration of stay in the hospital was around 5 days. Olerud Molander ankle score was used to evaluate functional outcomes. Functional outcome was observed as follows
The fracture was considered united when radiological evidence of callus formation was found on at least 3 cortices in AP and lateral radiographs with full weight-bearing capacity. The average time of union was around 16-20 weeks.62(96.87%) patients had union within the average period. 2 (3.13%) patients had surgical site deep infection. Implant removal was done in these patients followed by antibiotic therapy. They were continued with below-knee slab and were found to have delayed union. All the patients had satisfactory reduction with less than 5 degrees of varus-valgus angulation, less than 10 degrees of rotation, and less than 1 cm of shortening. No complications of neurovascular injuries or compartment syndrome were encountered. There were no incidences of breaking of nails or screws during the period of study. None of the patients had ankle stiffness. Patients were able to squat, sit cross-legged with no difficulty in stairs climbing.
DISCUSSION Among all lower limb fractures, distal tibia fractures accounts for about 7-10%.7-10 As distal fractures of tibia has little anterior soft tissue coverage, they are more prone to blister formation after injury. Also, complications like infection, delayed-union, and non-union are more common. Tibial fractures show the highest number of treatment alternatives.11 In recent years, intramedullary nails were commonly used as a preferred modality for treating distal tibia fractures due to more biological fixation, minimal invasiveness, minimal damage to bone and soft tissue and their successful outcomes regarding rehabilitation. Bedi et al.15 in their study on surgical treatment of non-articular distal tibial fractures reported that IM nailing is a less invasive method that does not cause soft tissue compromise, spares vascularity, and is performed without opening the fracture area.12,13 which is consistent with our study. In the present study, associated fibula fracture was present in 51 (79.68%) patients which is similar to the study conducted by C C Teitz et .al.14The distal segment of these fractures is more difficult to control with intramedullary implants because of the metaphyseal flare above the plafond.15 According to study by Bahamonde et al. poller screws, poller k wires were extremely useful in achieving acceptable reduction.16 We also found them effective in achieving reduction at fracture site. In our study, the average time required for surgery was 80 minutes which is identical with study by Somashekar D et al.17 In a study by IM and Tae, surgical site infection was found in 3% of cases which is comparable to our study.18 The fracture united in 62 (96.88%) patients in around 16-20 weeks postoperatively except in 2(3.12%) patients where delayed union was observed. At the final follow up, the functional outcome was found to be excellent which is similar to a study conducted by Yong Li et al.19 Our study has limitations like lack of comparison group with other modalities of treatment. patients were operated on by different surgeons who had different experiences.
CONCLUSION Thus we conclude that intramedullary interlock nailing has excellent results in management of distal 3rd tibia fractures considering early weight bearing, lower complications and excellent functional outcomes. Though the choice of treatment should be based on surgeons expertise and clinical circumstances.
REFERENCES
Policy for Articles with Open Access
|
|
 Home
Home