Official Journals By StatPerson Publication
|
Table of Content - Volume 1 Issue 1 - January 2017
Postpartum pubic separation over 5 cm, in 28 yr old female, treated by stainless steel (SS) wiring through obturator foramen
Nilesh Keche1*, Kiran Patil2, Harshal Kalambe3
1Assistant Professor, 2,3Residents, Department of Orthopaedics, Dr. V. M. G. M. C., Solapur, Maharashtra, INDIA. Email: nileshjkeche.keche3@gmail
Abstract The post partum pubic symphysis separation is an uncommon complication after term vaginal delivery. It occurs more commonly due to manual pressure applied to the pelvis in a latero-lateral and antero-posterior direction during normal vaginal delivery. The reported incidence of peripartum pubic separation varies from 1 in 300 to 1 in 30,000 deliveries. Mild separation of the symphysis pubis up to 0.5 to 1 cm during pregnancy is considered physiological. As per knowledge of author only handfull cases are reported in literature, Here we have a case of 28 year old female with postpartum pubic separation 5.1 cm, treated surgically by using stainless steel (SS) wiring through obturator foramen, which is new and more physiological technique for treating pubic separation. Pubic symphysis is a secondary cartilaginous joint where always a micromotion in vertical direction during one stance and walking is present. Hence our less rigid SS wire construct never obliterate micromotion which is more physiological. Operative treatment by an open reduction and stainless steel wiring through obturator foramen yielded excellent results. Keywords: Postpartum, Pubic Symphysis, Separation, Stainless Steel (SS) Wire, Obturator Foramen.
INTRODUCTION Rupture of pubic symphysis is an uncommon event after vaginal delivery. Reported incidence varies from 1 in 300 to 1 in 30,000 deliveries1.The pubic symphysis is a secondary cartilaginous joint. It is joint that allows limited micromotion except under hormonal stimulation during birth when it becomes progressively loosen. In normal conditions these movements are up to 1.3 mm.2 Starting from the seventh month of pregnancy a widening of the pubic symphysis occurs up to 4-8 mm. Thus separation up to 0.5 to 1 cm consider physiological during pregnancy, greater separation can lead to tenderness on palpation and disability to ambulate3. Factors that contribute to a rupture of pubic symphysis are rarely defined. Nevertheless, it seems clear that multiparity, macrosomia accompanied by cephalopelvic disorder, McRoberts maneuver, forceps, maternal connective tissue disorders, prior pelvic trauma, and hyperflected legs may predispose to pubic symphysis diastasis3,4,5. Diagnosis can be confirmed rapidly by pelvic X-ray. Additionally, MRI serves to exclude soft tissue injury. However, there is no consensus on the optimal therapy6,7. Typically, a conservative treatment is performed comprising pelvic girdle, analgesia, bed rest in lateral decubitus, and physical therapy1,3,8-13 In cases of extreme pubic symphyseal rupture with pelvic instability or persistent pain after conservative therapy, operative treatment is a successful alternative method5,7,14 -16. A diastasis of the pubic symphysis after birth is a rare but painful complication that causes serious distress to the patient. Clinically, the patient complains of pain, with swelling and sometimes deformity appearing in the involved area. The pain increases when manual pressure is applied to the pelvis in a latero-lateral and antero-posterior direction. When this occurs, adequate treatment should be given while keeping in mind the symptoms and separation gap. Here we have a 28 year old female patient with post partum pubic separation over 5 cm without sacroiliac joint disruption, treated successfully by stainless steel (SS) wiring through obturator foramen, which provide physiological micromotion at pubic symphysis joint as compare to other rigid methods of fixation.
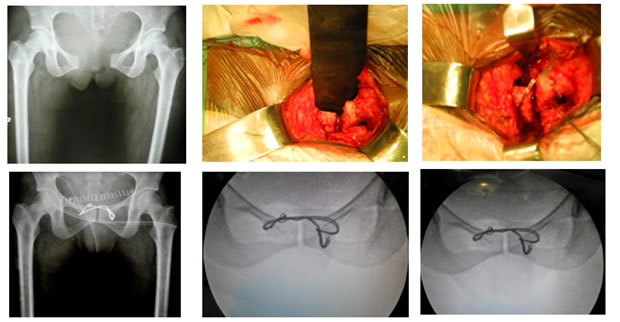
CASE HISTORY We present a case of spontaneous symphysis pubis separation in a healthy primigravida, after a straightforward, uncomplicated, non-operative, term vaginal delivery. Patient was a 28-year-old primigravida with no previous medical or surgical history. She had an uneventful antenatal history, and all her routine antenatal blood investigations and ultrasound scans were normal there were no history of trauma. She had an uncomplicated normal vaginal delivery. Clinically, the patient complained of pain, with swelling. Pain radiating to bilateral buttocks and thighs. A pelvic X-ray and CT Scan (Figure-1) was done, revealed a wide separation of the symphysis pubis measuring about 5.1 cm. The sacro-iliac and hip joints appeared intact. A conservative approach to management was undertaken. The patient was advised strict bed rest with a suitable pelvic-immobilising device. But after 2 weeks patient still complained a similar pain consistently that aggravates with movement. Thus surgical fixation method of management was decided. We had taken approach anteriorly through pfannensteil incision to pubic joint. Reduction was done by giving lateral compression. By using stainless steel (SS) wire through obturator foramen (figure 2 and 3), figure of 8 arrangement of fixation constructed and immediate postoperative pelvic X-ray (figure-4) showed reduction of pubic separation. postoperatively advise bed rest for 1 month. One month later she was seen at the outpatient clinic. She was able to walk independently with walker and no longer experienced any pain. A pelvic C – arm shoot (figure-5) after 1 month taken, showed stable fixation with no pubic separation. 6 months after the delivery, she was reviewed again at the outpatient clinic. This time, she was found to be in better health. She had pelvic C – arm shoot (figure-6), which showed the persistence of reduction with normal alignment of symphysis pubis joint.
DISCUSSION This case illustrates the rare occurrence of pubic symphysis diastasis in a healthy primigravida following an uncomplicated term vaginal delivery. Postpartum pubic symphyseal rupture was diagnosed on clinical grounds and the diagnosis was confirmed by radiography with an anteroposterior X-ray of the pelvis, which showed diastasis of the pubic rami. Although the initial clinical examination and diagnostic investigation are straightforward, the optimal way of treating a peripartumpubic symphysis rupture is discussed controversially. Several reports have shown that a conservative therapy is a reasonable approach1,3,10–13. Even in cases of large symphyseal rupture, a successful conservative therapy has been reported. However, other works have demonstrated the limitations of a conservative treatment. For instance, Kharrazi et al.5 presented four cases of pelvic and sacroiliac joint rupture after vaginal birth; in those women undergoing conservative therapy, posterior pelvic pain remained for more than two years. In addition, Rommens15 reported three cases of postpartum pubic symphysis rupture with persisting pain after conservative therapy. Those patients did not recover completely until they were operated by an open reduction and internal plate fixation. Niederhauser et al.4 demonstrated a similar case; after a symphyseal rupture occurring in a spontaneous vaginal birth with shoulder dystocia, conservative treatment failed to provide an optimal outcome. A 25mm gap was still present after 3 months and pain also persisted. Finally, surgical treatment by means of an open reduction and internal fixation yielded optimal results. Chang and Wu 16 showed that, in case of contraindication of a plate fixation due to a contaminated pelvic environment, an external fixation can be an equivalent surgical method of pubic symphysis diastasis. Dunivan et al.7 also underlined the advantages of an immediate external fixation in a case of pubic symphysis separation. As a consequence, these works suggest the indication of an operative approach if a gap of the pubic symphysis is larger than 40mm5,7,14,15. As we highlight in our case report, we agree with this threshold. In our case pubic separation found to be 5.1cm, here in our case conservative approach fails to reduce symptoms hence we treated patient by open reduction and fixation by Stainless Steel (SS) wiring through obturator foramen, which allows more physiological micromotion in vertical direction during one stance weight bearing and walking which is present there in normal pelvis and restricted by other method of rigid fixation2. Thus our case report is unique in having large pubic separation, and also unique in treatment by open reduction and fixation by more physiological Stainless Steel wiring through obturator foramen providing micromotion at symphysis pubis joint.
REFERENCES
|
|
 Home
Home