Official Journals By StatPerson Publication
|
Table of Content - Volume 1 Issue 2 - February 2017
Antibiotic impregnated PMMA coated nails for Infected nonunion of long bone diaphyseal fractures
P V Thirumalai Murugan1*, B Jeyakumar2
1Associate Professor, 2Professor, Department of Orthopaedics, Government Theni Medical College, Tamil Nadu, INDIA. Email: drthiruortho@gmail.com
Abstract Background: Management of infected nonunion of long bones is a major challenge. The problem in treating them are 1) Infection. 2) poor soft tissue envelope. 3) Instability. 4) Deformity. The principle in treating these comp; icated issue, Eradication of infection – convert the septic nonunion to an aseptic nonunion. Stable fixation by external or internal methods. Bony union. Chronic infection of bone with nonunion and/or bone defects is traditionally treated by a 2-stage procedure involving initial debridement and antibiotic delivery and then definitive internal fixation. Alternatively, external fixators are used to provide stability. Advantage: 1) multiple procedures. 2) prolonged course of treatment Disadvantage: 1) poor patient compliance. 2) pin tract infections. 3) muscle contracture & joint stiffness. 4) Systemic antibiotic toxicity. Surgical technique: A technique with which antibiotic cement-coated interlocking intramedullary nails are prepared in the operating room with the use of nails and materials that generally are available is herein described. Although useful for all infected nonunions and/or segmental bone defects, this technique is particularly useful for patients who are not ideal candidates for external fixation and for those who do not want to have an external fixator applied. Materials and methods: This technique was used in a series of 10 patients. 10 cases of post traumatic infected non-union, 8 cases – femur , 2 cases – tibia were treated 8 cases – compound fractures, 2 cases – simple fracture. Exclusion Criteria: 1) anticipated shortening > 2 cms. 2) poor soft tissue envelope. Results: 9 cases were followed for an average of 2 years (6 months to 2.5 years). We lost follow-up in 1 case. Radiological evaluation was done at 6 weeks, 12 weeks and 6 months. All cases went on for union between 6 to 12 months. Nail removal at 18 months. one patient had persistent sinus discharge but the fracture unite Conclusion: Antibiotic impregnated PMMA coated nails for infected nonunion may control infection and achieve bony union , with better patient compliance. Key Words: Antibiotic coated nails, Infected non union femur, Infection non union.
INTRODUCTION Nonunion in the presence of infection presents with the dual problems of controlling infection and providing stability. Traditionally, the treatment strategy consists of surgical debridement with local and systemic antibiotic delivery and then a second procedure for stability, generally either internal or external fixation. Special reconstructive procedures and soft tissue procedures might also be necessary. Local antibiotic therapy is a useful technique that results in high local concentrations of antibiotics with minimal systemic levels. This method in the form of antibiotic impregnated polymethylmethacry late (PMMA) beads is used in the treatment of osteomyelitis and open fractures.
SURGICAL TECHNIQUE Figure 1 Figure 2 Figure 3 Figure 4 Legend Figure 1: Thorough debridment of non union site; Figure 2 & 3: Preparation of PMMA antibiotic coated nail; Figure 4: Insertion of nail. The surgical technique involves a series of steps, each of which is critical for successful results. The first step is careful preoperative evaluation of culture and sensitivity results and radiographs. The second step involves thorough debridement of the infected bone and soft tissues and then copious lavage. All the nonviable and infected tissues, including the skin, soft tissues, and bone, undergo debridement until bleeding viable tissue is present at the resection margins (the Paprika sign in the case of bone). Inadequate debridement leaves nonviable or infected tissue secluded from the microcirculation, resulting in recurrence of infection despite local and systemic antibiotic delivery. This in turn facilitates biofilm formation, which protects the pathogens from antibiotics and host defense mechanisms. The third step is the preparation of the antibiotic cementcoated interlocking intramedullary (IM) nail under sterile conditions in the operating room. While a team of surgeons perform debridement of the infected nonunion site, another surgeon prepares the nail on a separate sterile table. Molds (templates) are usedto provide a uniform cement mantle of 1 mm circumferentially around the IM nail, starting from just distal to the proximalinter locking holes and extending to the tip of the nail One gram of vancomycin and 3.6 g of tobramycin are added to each batch of bone cement (40 g) for all patients except those with a history of allergies to these antibiotics. The bone cement is placed into each side of the mold with the use of a cement gun nozzle while the cement is still in a liquid state. Then the IM nail is placed in the mold and the second mold is placed over it. The nail with antibiotic cement coating is removed after the cement sets (usually in 8 to 10 minutes). The next step is to ensure that the antibiotic cement coated IM nail is suitable for insertion into the bone. An osteotome is used to remove excess cement from the surface of the cement-coated nail. In addition, if necessary to facilitate insertion of the locking screws, any cement covering the distal interlocking holes can be removed by using instruments with pointed tips. The final steps in this technique involve preparation of the IM canal and insertion of the antibiotic cement-coated nail. Reaming of the IM canal is performed to 1 mm more than the diameter of the antibiotic cement-coated nail. One millimetre of cement mantle coating is provided around the nail; the final diameter of the antibiotic cement-coated nail is therefore 2 mm more than the IM nail itself. ‘‘Cement-nail de bonding’’ (separation of the cement from the IM nail) can occur during insertion of antibiotic cement-coated IM nail. This can be prevented by adequate over-reaming of the canal. However, when this does occur, the de bonded cement is removed and a new antibiotic cement coated nail is prepared and used. Exchange nailing, if necessary, is done without an antibiotic coating (generally to a larger nail for additional stability) if the infected nonunion has been converted to a nonunion without infection. If there is no infection and union has occurred, the antibiotic-coated IM nail can be left in situ permanently. If both infection and nonunion persist, the IM nail is exchanged for another antibiotic cement-coated IM nail, generally 6 to 8 weeks after the index surgery. If removal of an antibiotic cement-coated IM nail is indicated, it is performed in a standard fashion with care taken to prevent cement-nail debonding. If debonding does occur, the cement mantle can be removed with reasonable ease by using a J-hook which usually is used forcement removal during revision total joint arthroplasties.
MATERIALS AND METHODS This technique was used in a series of 10 patients.
Exclusion Criteria
RESULTS
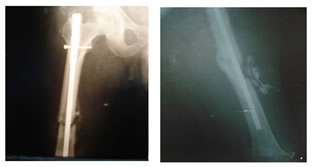
Figure 5: 45 years female with 6 months old infected nonunion femur. Picture 6: x ray showing PMMA antibiotic nail and beads
Picture 7: Fracture healing after 1 and 2 years. Figure 8: clinical photo of healed wound
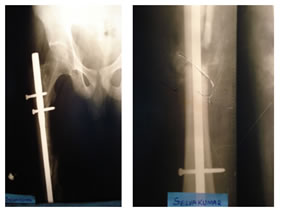
Figure 9: 40 years male with 1.5 years infected nonunion Figure 10: immediate po with PMMA coated nail and bead. Figure 11: 8 months po showing union. Figure 12: infected nonunion 10 months old Figure 13: 10 months post op showing healing
Figure 14: Clinical photo showing healed wound with no discharge DISCUSSION Infected nonunions and segmental bone defects demand treatment methods that offer control of infection and provide stability to the bone to promote union. Surgical debridement and use of local and systemic antibiotics help in achieving control of infection. Local delivery of high concentrations of antibiotics achieves control of infection while avoiding systemic complications of antibiotic use. Various methods of local antibiotic delivery are used, including antibiotic cement beads and spacers, bioabsorbable delivery vehicles such as calcium sulfate, and synthetic polymers. The most common infecting organism in the literature and in our study is Staphylococcus aureus . S. aureus also occurs in combination with other pathogens in 65% to 70% of patients. Aminoglycosides and vancomycin are common choices for local delivery of antibiotics because of their broad spectrum of activity, heat stability, and low allergenicity. As such, antibiotic-impregnated bone cement used for treatment of established infection still requires hand-mixing of higher dosages of various antibiotics into bone cement by the treating physician as a clinician-directed application. Elution of antibiotics from PMMA beads follows a biphasic pattern, with an initial rapid phase and a secondary slow phase. Elution is at its maximum during the first day, greatly declines on the second day, and then gradually decreases over time and seems to stabilize between days 5 and 10. Beads implanted in patients for fewer than 10 weeks elute considerably higher antibiotic levels than do beads implanted for more than 14 weeks. Animal and clinical studies consistently have shown high local concentrations and undetectable or very low serum levels of the locally delivered antibiotics with no systemic toxicity. The safety of local antibiotic therapy has been well documented in clinical studies. The systemic absorption of the locally delivered antimicrobial agent is limited and results in extremely low serum levels, which have ranged from 0.3 to 0.5 mg/mL in the case of gentamicin. With our technique, vancomycin and gentamycin are added to bone cement. As discussed earlier, these antibiotics are effective against many of the bacteria generally found in our patients. Furthermore, they have been shown in clinical and experimental studies to be heat stable, with good elution properties from bone cement, and have little deleterious effects on bone healing. Stability at the nonunion site can be provided with the use of internal or external fixation. A combination of an IM nail with vancomycin and gentamicin beads or antibiotic-impregnated cementinserted into the site of infection has been reported for treatment of infected nonunions. However, this might require an additional procedure for removal of the cement beads or cement mass. The use of guide rods coated with antibiotic-impregnated cement prepared by using chest tubes as molds has been reported as the first stage of treatment in infected nonunions.23 However, this approach requires removal of the cement-coated rods after 6 weeks and insertion of IM nails for providing stability to the nonunion. Our technique was developed based on these observations with the goal of combining the 2 procedures into a single surgery. In our patients, the combination of good bone stability and antibiotic delivery provided the environment for eradication of infection, promotion of bone union, and improved mobility with immediate partial to full weight bearing. External fixators have been used for the treatment of infected nonunions. However, the use of external fixators is associated with a high incidence of pin site infections and soft tissue transfixation by pins and wires causing muscle contractures and joint stiffness. This is more pertinent in cases of femoral nonunions than in cases of tibial nonunions. Moreover, some patients do not consent to the use of external fixators because of cosmetic reasons. Additionally, some patients are not ideal candidates for the use of external fixators because of poor compliance with treatment, including pin sitecare, or because of obesity, which increases the risk of pin site infections. These patients can directly benefit from the antibiotic cement-coated nail method. In summary, control of infection and stability to promote union has traditionally been provided by 2 separate procedures, methods that have proved to be efficacious in the past. However, both these goals can be achieved in half the patients. with 1 surgical procedure in a variety of scenarios by using the technique of antibiotic cement-coated IM nail. These are cases that would have alternatively required circular external fixation and bone transport to achieve adequate stability and bone union. This 1-step surgical procedure eliminates the complications that can occur secondary to the use of external fixation and bone transport. It may also reduce the morbidity of 2 surgical procedures and inpatient admissions required for the 2-stage procedures or for the application and removal of external fixators to that of a single procedure and inpatient admission. Additional procedures may be required with both treatment methods for achieving control of infection, bony union, or soft tissue coverage. REFERENCES
|
|
 Home
Home