Official Journals By StatPerson Publication
|
Table of Content - Volume 1 Issue 2 - February 2017
Study on the proximal femoral nail fixation for unstable trochanteric fracture
A V Shabi1*, S Abdul Hameed Ansari2
1,2Sr. Assistant Professor, Department of Orthopaedics, Government Thiruvarur Medical College, Vilamal, Thiruvarur, Tamil Nadu, INDIA. Email: dr.shabi@yahoo.com
Abstract To assess the clinical, radiological and functional outcome of unstable trochanteric fracture when treated with PFN. Totally 20 cases of unstable trochanteric fractures selected for this prospective study at Department of Orthopaedics, Govt. Thiruvarur Medical College and Hospital during the period of May 2010 to May 2017. PFN is a significant advancement in the treatment of unstable trochanteric fractures which has the unique advantage of closed reduction, preservation of fracture hematoma, less tissue damage during surgery, early rehabilitation and early return to work. Key Words: Intramedullary Nailing Proximal Femoral Nail, DHS, Unstable Trochanteric Fracture.
INTRODUCTION Trochanteric Fractures are one of the devastating injuries in elderly. Intramedullary nailing1 with proximal femoral nail2 has distinct advantages over DHS3, for Unstable Trochanteric4 fractures. Proximal femoral nail has the unique advantages of closed reduction, preservation of fracture Haematoma, Less Tissue damage during surgery, early rehabilitation and early return to work. Incidence of per operative and Post operative femoral shaft fractures in PFN can be reduced by good Pre-operative planning, correct technique, adequate reaming of femoral canal and insertion of implant by hand.
MATERIALS AND METHODS Totally 20 cases of unstable trochanteric fractures selected for this prospective study at Department of Orthopaedics, Govt. Thiruvarur Medical College and Hospital during the period of May 2010 to May 2017. All 20 hips were treated with Proximal Femoral Nail all the patients came for regular follow up and they were included in the study. The age group varied from a minimum of 30 years to a maximum of 84 years and average age was 56.3 years. Mean follow up was 15.4 months of the 20 patients 16 were male and 4 were female. Right side involved in 8 cases Left side involved in 12 patients.18 patients were manual labourers, two were sedentary workers. All the fractures were classified according to Boyd and Griffin classification for Inter- trochanteric fractures. Only type III and Type IV were included in the study. MODE OF INJURY RTA (Road traffic Accidents): 13 Accidental fall: 7, The average interval from the injury to the time of surgery was 6.6 days. All the patients were managed initially with skeletal traction before taking up for surgery. Pre operative planning Pre operative templating with AP – Roentgenogram of injured hip was used to measure the nail diameter and lag screw length. Implants and Instruments F1 Length of short PFN - 1350 25 cm Length of Long PFN - 1350 36, 38, 40, 42 cm Proximal Diameter 15mm Proximal Nail Angulation 60 Distal diameter 9, 10, 11,12mm Lag screw diameter 8 mm Derotation screw diameter 6.2mm Distal locking bolt 4.9mm Jig for proximal and distal reamers and for locking Guide wire 2 mm Canulated step reamer guide wire sleeve and drill sleeve
Figure 1
Anaesthesia, positioning and image intensifier: Surgery was done in standard radiolucent fracture table with patient in supine position with use of image intensifier. Sub Arachnoid block was used for all patients. Surgical technique: All the fractures were treated with initial closed reduction with alignment of the medial cortex. In two patients we could not achieve closed reduction and in those cases open reduction was done. Incision: The approach for PFN is a 5 cm incision extending proximally from the tip of the greater trochanter followed by careful separation of the abductors. Entry pointF2: The point of entry is the tip of the greater trochanter at the midpoint in the anteroposterior diameter and is made with a curved awl under c- arm guidance. Guide wire insertion and reaming: The guide wire is inserted using a tissue protector. The position of guide pin is checked in AP and lateral views. Entry point is reamed using 15mm entry point reamer and distal reaming of canal is done with graded canulated reamers, whenever necessary. C- ARM PICTURE
Figure 2: Entry Point F2 Figure 3: Proximal Targeting F3 Figure 4: Distal Targeting F4 Nail Insertion and Proximal targetingF3: The nail is inserted with the help of the jig over the guide wire. Fluoroscopic images are taken when the nail is being introduced to check for any peroperative femoral fractures. The nail along with the jig is inserted by hand by gentle twisting movements. Once the nail is positioned appropriately the guide wire is removed and drill sleeve are attached to the jig and through a stab incision over lateral thigh the drill sleeves are pushed upto the lateral cortex one for compression screw and one for derotation screw. The guide pin is then passed into the head and neck using guide pin sleeve. The guide pins are advanced upto 5mm short of articular surface of femoral head. Proximal locking with the compression screw along the inferior part of the neck is done first followed by the superior derotation screw of appropriate length as measured preoperatively and peroperatively. Distal Targeting F4 Distal locking is also done with the aid of jig and two distal locking screws. For long PFN – distal locking is done with free hand technique. Operating time was calculated from the start of surgical incision to wound closure and the duration of image intensifier in patient treated with the PFN was calculated in seconds. Blood loss was calculated from the number of surgical mops that were used, each mops corresponding to 50ml of blood. Operative time varied from 45 minutes to 95 minutes with average of 67.8 minutes. Blood loss varied from 150 ml to 350 ml with mean of 232.5 ml Post operative Protocol Knee and hip mobilization started on first post operative day. Patients were allowed partial weight bearing with aid, as tolerated. Sutures were removed on the 12th post operative day. In one patient who had bilateral Trochanteric fracture rehablitation was delayed. Time for fracture healing was evaluated according to radiographic and clinical criteria. Clinically Union was observed as the absence of Tenderness (or) pain with full weight bearing. Patients were evaluated clinically and radiologically at 3 weeks interval for first 3 months and there after monthly for the next 3 months and bimonthly for next 12 months. During follow up the Harris Hip Score was evaluated at 3 months and 6 months post operatively. Various parameter like pain, limp, use of support, distance walked, stair climbing, sitting, absences of deformity, range of motion were evaluated using Harris Hip Score. RESULTS Table 1
DISCUSSION The PFN is an effective intramedullary load - sharing device. It incorporates the principles and theretical advantages of the Zickel Nail, Dynamic hip screw and locked intramedullary nail.
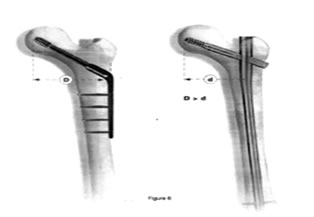
Figure 7: Side Plate Figure 8: Intramedullary System
Biomechanically PFN is more stiff, it has shorter moment arm i.e. from the tip of lag screw to the center of femoral canal whereas the DHS has a longer moment arm undergoes significant stress on weight bearing and hence higher incidence of Lag screw cut out and varus malunion. The larger proximal diameter (15 mm) of the PFN given additional stiffness to the nail. Minimal blood loss, shorter operative time, early weight bearing are all advantage of PFN whereas the DHS has a longer operative time and more blood loss.
Table 2
In the current study the union rate was 100% with two case of varus malunion. There were no cases of preoperative and postoperative femoral fractures. The average blood loss in patients treated with the PFN nail was 233 ml. The results were comparable with Bellabarba et. al. 2000.
Average operating time in our series was 67.8 minutes. In our initial cases operating time was on the higher range (Range 45 – 95 min). With experience the operating time reduced. Results were comparable to the series of Bellabarba et. al. 2000.
The use of image intensifier was 117 seconds in patients treated with the PFN, which is considerably less than that of Halder’s series (5.4 minutes in Halder et. al. 1992 series). In comparison, mechanical failure of DHS occurs in 10 to 20% of cases primarily due to cutting out of the lag screw superiorly (Wolfgang, Bryant and O’Neill et. al.1982). The operative blood loss in patients treated with DHS is higher (250 ml in Radford et. al… 1993 series). Full weight bearing is delayed in patients treated with DHS (Leung et. al... 1992). Peroperative and postoperative femoral fractures have been documented in patients treated with the PFN. Multiple factors have been implicated like implant design and operative technique. Decreases in implant curvature, diameter, over reaming of femoral canal by 1.5 to 2mm, insertion of the implant by hand and meticulous placement of the distal locking screws without creating additional stress risers decreases the complication rate of femoral shaft fracture (I.B. Schipper et.al. 2004). Patients with narrow femoral canal and abnormal curvature of the proximal femur are relative contra-indications to intramedullary implants (Halder et.al 1992). We have followed these recommendations in our series. Hence in our series we don’t have encountered any preoperative and postoperative femoral shaft fractures. A larger cohort of patients is necessary to document the incidence of preoperative and postoperative femoral shaft fractures, which is a limitation of our study. In our series the incidence of abductor lurch in the post operative period was 17.5% Gluteus medius tendon injury has been reported in 27 % patients with the use of Trochantric entry nails (Mc Connell et. al. 2003). The abductor lurch may improve in many numbers of patients and may remain static in some patients. Since the follow – up period of this study is short which is a limitation of our study, we could not definitely quantify the number of patients who developed permanent damage to abductor musculature. In short the PFN is a better implant with distinct advantages over the DHS. With adequate surgical technique, the advantages of the PFN increases and the complication rate decreases.
CONCLUSION Intramedullary nailing with the PFN has distinct advantages over DHS like shorter operating time and lesser blood loss for unstable trochanteric fractures. Early mobilization and weight bearing is allowed in patients treated with PFN thereby decreasing the incidence of bedsores, uraemia and hypostatic pneumonia. The incidence of preoperative and postoperative femoral shaft fractures in PFN can be reduced by good preoperative planning and correct technique, adequate reaming of the femoral canal, insertion of implant by hand and meticulous placement of distal locking screws. PFN is a significant advancement in the treatment of unstable trochanteric fractures which has the unique advantage of closed reduction, preservation of fracture hematoma, less tissue damage during surgery, early rehabilitation and early return to work.
REFERENCES
|
|
 Home
Home