|
Table of Content - Volume 20 Issue 2 - November 2021
Implant assisted correction of contracture across the joints
B Sreekanth Rao1, T Zeeshan Muzahid2*, M Venkaiah3, TVG Krishna4, GVS Moorthy5
1Associate Professor, 2Assistant professor, 3Assistant Professor, 4Associate professor, 5Professor, Department of Orthopaedics, Bhaskar Medical College and Bhaskar General Hospital, Yenkapally, Telangana, INDIA. Email: bsreerao@gmail.com
Abstract Background: Orthopedic implants are commonly used to correct bony deformities and for temporary stabilization after open reduction of dislocations. They are also of great help in release of soft tissue deformity corrections and contracture release across the joints. They can be external fixators to span across the joints or internal fixators to stabilize. Ten cases of contractures at different sites of upper limb are selected for this study, including elbow, wrist, and fingers. The subjects are from semi urban and rural areas of Telangana. The etiology was burns and trauma. The age of the subjects varied from 3 years to 21 years. The contracture durations were from 3 months to 18 years. Standard preoperative evaluation was done, and permissions were taken. Under anesthesia, without tourniquet, contracture release was done. External fixator spanning across the elbow and wrist joints and Internal fixation with Kirshner wires for fingers were fixed, after obtaining the maximum correction on the operation table. Split skin grafts were applied. None of them had any vascular or neurological compromise. Subsequently dressings were facilitated without discomfort and disturbance of graft. Movements are permitted to the extent possible to maintain muscular activity and other joint mobility. Followed up for a period of 6 months to 1 year. In all ten cases, the skin graft take up was complete. There was no further contracture formation. The recovery period in all cases was pain free. The stabilization with External fixator or internal fixation facilitated usage of the limb and mobility of intact joints and muscles, from immediate postoperative period. Dressing the operated parts was easy and comfortable to the surgeon and subjects. Position of the joints of the limb and dressings are not disturbed during activities. There were no infections. The regaining of joint movements was near normal and functional. Overall psychological morale and performance in Society by operated patients improved. Keywords: Trauma, External fixator, Upper limb, Contractures, Joints.
INTRODUCTION Skeletal immobilization is one of the oldest and most used treatment modalities for the trauma patient. External fixation has evolved from being used primarily as a last resort fixation method to becoming a main stream technique used to treat a myriad of bone and soft tissue pathologies.1 Importance should be given to preservation of function of the limb in contractures due to burns and trauma, which take more time to heal and before patient resumes activities. Post-traumatic wrist and metacarpophalangeal and inter phalangeal joint contractures are incapacitating conditions. They lead to crippling deformities and interfere with the activities of daily living. Skin grafting alone is not sufficient enough to treat the contractures across joints. The use of simple instruments like external fixator and kirschner wire has proven to be effective in providing bone/joint stability and a stable bed for skin graft application. External fixators provide postoperative adjustability. A thorough understanding of the biomechanical principles of external fixation is useful for all orthopaedic surgeons as most will have to occasionally mount a fixator throughout their career1. Spanning or trans articular external fixators can be safely applied by following the basic principles of external fixation.2 Early fixation reduces pain and discomfort and improves graft take, potentially reducing the amount of surgical interventions needed.3 External fixator with single stage procedure is best option. Using skin grafts in reconstruction has its own set of problems. They are prone to contracture and recurrence that are common after contracture release and grafting. So, there is a prolonged need of splintage, removal of splints at every dressing and physiotherapy in the postoperative period. Physiotherapy should be considered in the management of cases preoperatively and postoperatively, tailored to each case.4
MATERIALS AND METHODS This prospective study was conducted from December 2017 to June 2021. Permission for study was taken from ethical committee of the institution. Patients included in study for treatment of contracture of fingers, wrist and elbow due to burns and trauma. Patients included in study for treatment of contracture of fingers, wrist and elbow due to burns and trauma. Four are children in the age of 3 to 5 years, brought by parents to hospital between 3 to 6 months after burns and trauma. Six are adults in the age of 18 to 21 years, with contracture duration between 2 months to 18 years, affecting fingers, wrist and elbow. Treatment is done with contracture release, skin grafting, K-wires and external fixator. Treatment of these patients is aimed at improving independence of daily activities and better performance. The 10 patients are from semi-urban area and were treated and followed up for period of 6 months to one year. Physiotherapy was done under supervision. Results were assessed based on - Uptake of skin graft, Anatomical alignment of joints, Functional range of movements and overall psychological improvement.
RESULTS Skin grafts were taken up, anatomical alignments of joints achieved, functional range of movements achieved in all patients. No patient needed reoperations. There were no wound infections. There was psychological improvement in some patients, who were pessimistic and used to hide their deformed joints. Post-operatively they are optimistic, psychologically highly motivated, social stigma is overcome. They are able to do the activities of daily living, driving vehicles. One young lady patient became confident to get married after surgical correction.
Table I: Age and Sex distribution.
Table II: Age and Time since injury / burns.
Table III: Number of Digits and Web spaces involved
Table IV: Wrist and Elbow requiring spanning External Fixator
Table V: Types of Fixation and Duration of treatment
Table VI: TAM Score
Table VII: Pre-Operative and Post Operative Functional Capacity.
Table VIII: Psychological improvement.
Figure 1: CONTRACTURE RELEASE, K -WIRES IN FINGERS, EASE OF DRESSING
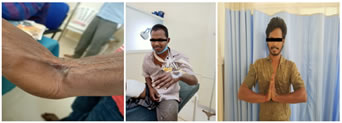
Figure 2: CONTRACTURE HAND and ELBOW, EXTERNAL FIXATOR WRIST and ELBOW, EASE OF DRESSING, PHYSIOTHERAPY, FUNCTIONAL IMPROVEMENT
Figure 3: CONTRACTURE WRIST, EXTERNAL FIXATOR WRIST EASE OF DRESSING, FUNCTIONAL IMPROVEMENT
DISCUSSION The world literature documents external fixation and distraction for extremities as an established modality for management of severe contractures following post burn and traumatic injury.5,6External fixation involve the use of percutaneously placed transosseus pins and wires secured to external framework to provide support to a limb and joint. The benefits of external fixation are numerous. When compared with internal plates and intramedullary nails, external fixators cause less disruption of the soft tissues, osseus blood supply, and periosteum.7 Unilateral frames allow the limb to remain functional, avoid complications, and provide bony stability.8 Knee flexion and extension contractures as well as ankle equines contractures have been successfully corrected with a gradual technique using a simple hinge construct.9,10 The most common risk after contracture release, despite adequate occupational therapy is recurrence. It is for this reason we utilize dynamic distraction external fixation.11 The upper limb is viewed as a mechanism to place the hand in space where it is needed to perform necessary functions. The function of a normal hand is grossly limited if active elbow flexion is absent. Lack of active elbow extension may result in an inability to stabilize paper on a desk with one hand to write with the other.12 Joint contractures are a common complication of hand trauma and can have several causes related to contractures or adhesions of the tendons, thickening of the synovium, contracture of the ligaments or joint capsule, insufficient skin cover or scarring and bone block or exostosis within the joint.13 By distraction straightening, the principles of a gradual dynamic lengthening of the skin and soft tissues are applied. All tissues get stretched out, thus maintaining a sensate pliable skin cover.14 Muscles produce force and movement and these properties can be adversely affected by contracture and contracture treatment. Therefore treatment should therefore be directed to maintain to increase contractile and connective tissue length whilst reducing stiffness and loss of elasticity. Muscle properties of force generation should be “normalized” through treatment.15Skin grafts and soft tissue procedures for the elbow and wrist can be testing, at times they do not take in when there is immoderate motion. Immobilization of these joints with the simpler splints may not be a better choice, as the surgical sites would need regular monitoring and wound care. We believe that in splints along with motion there can be wound soakage adding to infections and complications leading to disorganised graft incorporation. This study is a small case series to offer this as a technique and treatment option on post traumatic and burns contractures injuries of elbow, wrist and, hand. Evaluated and treated by contracture release, split skin grafting, the placement of a spanning external fixator, kirshner wires. This study we demonstrated that spanning external fixation, kirshner wires is an applicable option to treat these injuries. In this study all the procedures were done under general anesthesia, no tornique was used. we used kirshner wires to immobilize the finger joints after release of contractures and correction of deformities, split skin grafting done over the raw areas, secured by 3.0 silk sutures. Web spaces contractures were also attended with contracture release and split skin grafting, here to maintain the abduction between the fingers we kept cut latex glove fingers filled with water and sealed. In cases of wrist and elbow contractures after releasing of contractures and correcting the deformities external fixators were spanned across the joint. This procedure was very economic kirshner wires, external fixator easily available least expensive can be removed with ease not needing anesthesia /operation theatre charges. External fixators connecting rods and clamps can be reused after autoclaving especially in patients who cannot afford, it is like a blessing in disguise. Dressings could be changed with ease. Never needed the expensive separators between fingers as we used the least expensive easily available latex gloves and filled with water. They were very playful for the children and welcomed it with happiness. Surgery to achieve active movements in these patients to enhance function, requires committed patient compliance with treatment for retraining of the muscles used to achieve the active movements. We could win their trust, in return we motivated them throughout the period of treatment through physiotherapy rehabilitation. In all the patients post-operatively there was no neurological deficit. Donor site had no complications. After the removal of fixations patients were subjected to physiotherapy under supervision were followed for 6 months to one year. It helped them gain anatomical alignment, functional range of movements in with results ranging from good to excellent.
CONCLUSION We found that orthopedic devices are an excellent tool in the equipment of the surgeon to treat the burn, trauma joint deformities. Every patient is very different, so treatment must be modified to match the clinical observations. Consistent postoperative motion and therapy remains essential for successful outcome. The crucial key is motivated, compliant patients and their parents. The functional and stunning excellent results of these procedures, was supplemented with physiotherapy rehabilitation. It has advantages that it allows regular wound inspection without change in position and useful especially in children where it is difficult to maintain the position of joints by the conventional methods. The least cost, low distress, ease of wound care, psychological booster and minimal complications make this an alternative to the other techniques used, either as the first line therapeutic treatment option or as a last hope when other techniques have crashed. The functional, cosmetic and psychological results of this approach of treatment are exceptionally satisfactory. It was very economical pocket friendly, minimally invasive technique to treat the contractures across hand, wrist and elbow joints treated in semi-urban population.
REFERENCES
Policy for Articles with Open Access
|
|
 Home
Home