|
Table of Content - Volume 20 Issue 2 - November 2021
A study of Functional outcome and complications of open reduction and internal fixation with plate for displaced midshaft clavicle fractures at a tertiary health care centre
Sagi Radha Krishna Rao1, Pankaj Kabra2*
1,2Assistant Professor, Department of Orthopaedics, Surabhi Institute of Medical Sciences, Mittapally Village, Siddipet Mandal And District, Telangana State, INDIA.
Abstract Background: Clavicle fracture is one of the important fractures around shoulder joint. Surgical treatment is effective and with less complications than the traditional conservative methods. Aim and objective: To compare the Functional outcome and complications of open reduction and internal fixation with plate for displaced midshaft clavicle fractures at a tertiary health care centre Methodology: Present study was a prospective study conducted on patients with mid shaft clavicle fracture admitted at a tertiary health care centre. Data included sociodemographic data, clinical history, clinical examination and outcome of surgery. Primary outcome was union. Functional outcome was measured by DASH score (Disability of Arm Shoulder and Hand Score). Pain was assessed by visual analogue scale (VAS). Satisfaction with cosmetic appearance of incision and shoulder was analysed by VAS Scale. Results: Union rate was 93.3%. Symptomatic hardware was seen in 5 patients. Re operation rate was 23.33%. DASH score in patients without complications was (13.4±3.1) significantly less than DASH score in patients with complications was (21.3 ± 2). Mean pain score in patients without complications (0.4±0.1) was significantly less than in patients with complications (2.3±0.6) (p<0.05). Cosmetic appearance score was significantly higher in patients without complications than patients with complications (p<0.05).
INTRODUCTION Clavicle is an important subcutaneous bone in the human body. Clavicle fractures are common fractures with an incidence of 59.3 per 100,000 person years.1 Fractures of clavicle are common contributing 5 to 10% of all adult fractures and up to 40% of injuries around shoulder girdle.2-5 Majority of the clavicle fractures are in middle third of bone because junction between the two cross-sectional configurations occurs in the middle third and is a vulnerable area to break for fracture, especially with axial loading. Shaft fractures occur most commonly in young adults.6 Traditionally, displaced midshaft clavicle fractures have been treated conservatively. Conservative methods were applying a simple sling, clavicular brace or figure of eight bandage.7,8 Advantages of conservative methods are they are cheap, affordable and is devoid of the risks of anesthesia. Various dis advantages are high rates of non-union, symptomatic malunion and shoulder stiffness with nonoperative treatment.9,10 Previous studies reported better union rates, improved early functional outcomes, and increased patient satisfaction in surgical treatment of displaced mid-shaft clavicle fractures (DMCF).11-13 Various operative methods for treatment of mid-shaft clavicle fracture are intramedullary devices, plates, and external fixators. Plating of mid-shaft clavicle fracture is preferred method of fixation by many authors. The current gold standard in operative treatment is Open Reduction Internal Fixation (ORIF) using plates and screws. These devices aim to reduce the DMCF in a minimally invasive manner and thereby improving cosmetic satisfaction and union rates while lowering infection rates.14 Plate fixation resists the bending and torsional forces that occur during elevation of the upper extremity above shoulder level so it is better than intramedullary fixation. Plate fixation allows full range of motion to the patients. Present study was conducted to compare the Functional outcome and complications of open reduction and internal fixation with plate for displaced midshaft clavicle fractures at a tertiary health care centre. Aim and objective: To compare the Functional outcome and complications of open reduction and internal fixation with plate for displaced midshaft clavicle fractures at a tertiary health care centre
MATERIAL AND METHODS Present study was conducted in department of Orthopaedics at a tertiary health care centre. Study population was patients with midshaft clavicle fracture admitted in orthopaedic department. Inclusion criteria: 1. Patients with acute, displaced mid-shaft clavicle fractures with significant shortening (>2cm) 2. Displacement (>100% width of clavicle) or Z- type fracture pattern or significant comminution 3. Patients in the age group of 18-65 years of either sex Exclusion criteria: 1. Patients with non-midshaft fracture 2. Patients with pathological fractures 3. Patients with associated vascular and neurological injury 4. Patients with open fracture Study was approved by ethical committee of the institute. A valid written consent was taken from the patients after explaining study to them. Data was collected with pre tested questionnaire. Data included sociodemographic data, clinical history. Through clinical examination was done. All patients underwent necessary investigations like Xray, complete blood count, renal and liver function tests. Pre anaesthetic check-up was done. Prophylactic antibiotics were given before operative procedure. All surgeries were carried out under general anaesthesia. A curvilinear incision was made over the clavicle to expose the fracture. The fracture was reduced and fixed with plate placed on superior surface. Transverse fractures were fixed with axial compression. Oblique fractures were fixed with a lag screw and neutralisation plate. In comminuted fractures, bridge plate technique was used. A collar cuff sling was given for two weeks. Sutures were removed on 14th postoperative day. Patients were followed upto one year. Functional outcome was measured by DASH score (Disability of Arm Shoulder and Hand Score). DASH is a 30 points self-report questionnaire used to describe the disability experienced by people with upper limb disorders. Pain was assessed by visual analogue scale (VAS) from 0 (no pain) to 10 (extreme pain). Satisfaction with cosmetic appearance of incision and shoulder was rated on 10 point VAS Scale. Overall satisfaction with treatment was recorded on 3-point Likert Scale as unsatisfied, partially satisfied and fully satisfied. Data was entered in excel sheet and was analysed by SPSS version 20.0.
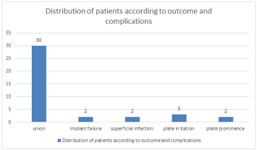
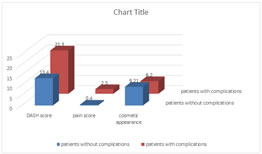
RESULTS In our study, we studied 30 patients. Majority of the patients were in the age group of 31-50 years 19(63.33%). Patients in the age group of 51-60 years were 10%. Patients in the age group of 18-30 years were 8(26.67%). Mean age of the patients in our study was 32.5 ±3.4 years. (table1) In our study, out of 30 patients, 23 patients were male and 7 patients were female. Mal e to female ratio was 3.3:1. Cause of injury in 20 patients was high energy trauma and 10 patients had low energy trauma. According to Robinson’s classification 13 belong to 2B1 and 17 patients belonged to 2B2. In our study, most commonly used plates were 3.5mm pre-contoured locking plate (46.67%) followed by 3.5 mm reconstruction plate (33.33%). 3.5 mm Dynamic Compression plate was used in 20% patients. (table 2) Fig 2 shows distribution of patients according to outcome and complications. All 30 patients have union. Two patients had implant failure due to plate breakage. Out of these plates, one was locking plate and one was reconstruction plate. Implant was removed in these patients and plate fixation with iliac crest bone graft was done. Union was observed in 18-20 weeks in these patients. Two patients had superficial infection post operatively. These patients were treated with antibiotics. Symptomatic hardware were related to plate breakage. 3 patients complained of plate irritation and 2 had plate prominence. Out of these 5 patients 2 were DCP, 2 was LCP and 1 was reconstruction plate. Out of 30 patients, 7 patients were reoperated. Fig 3 shows Comparison of outcome in patients with complications and without complications. DASH score in patients without complications was 13.4±3.1 and DASH score in patients with complications was 21.3 ± 2. This difference was statistically significant (p<0.05). Mean pain score in patients without complications (0.4±0.1) was significantly less than in patients with complications (2.3±0.6) (p<0.05). Cosmetic appearance score was significantly higher in patients without complications than patients with complications (p<0.05). Table 1: Distribution of the patients according to age group
Figure 1: Distribution of patients according to sex
Table 2: Distribution of patients according to type of plate
Figure 2 Figure 3 Figure 2: Distribution of patients according to outcome and complications; Figure 3: Comparison of outcome in patients with complications and without complications
DISCUSSION We studied 30 patients. Majority of the patients were in the age group of 31-50 years 19(63.33%). Mean age of the patients in our study was 32.5 ±3.4 years. In our study, 23 patients were male and 7 patients were female. Male to female ratio was 3.3:1. These results were comparable with Kumar Gaurav et al.15 Cause of injury in 20 patients was high energy trauma and 10 patients had low energy trauma. According to Robinson’s classification 13 belong to 2B1 and 17 patients belonged to 2B2. All 30 patients have union. Union rate in our study was 93.3%. Previous studies on primary plate fixation of acute midshaft clavicular fractures had union rates in the range of 94 to 100%.16,17 Woltz et al.13 conducted a RCT and found union rate of 97.6% (84/86) in primary plate fixation group. Two patients had implant failure due to plate breakage. Out of these plates, one was locking plate and other was reconstruction plate. Implant was removed in these patients and plate fixation with iliac crest bone graft was done. Two patients had superficial infection post operatively. These patients were treated with antibiotics. 3 patients complained of plate irritation and 2 had plate prominence. Out of these 5 patients 2 were DCP, 2 was LCP and 1 was reconstruction plate. Out of 30 patients, 7 patients were reoperated. Leroux et al. Found 24.6% reoperation rate. Isolated implant removal was the most common cause of reoperation contributing 18.8% reoperations.18 Naimark et al. in a cohort of 7826 patients, reported 12.7% hardware removal rate.19 DASH score in patients without complications was 13.4±3.1 and DASH score in patients with complications was 21.3 ± 2. This difference was statistically significant (p<0.05). Similar results were observed in previous studies.3,13,16 Mean pain score in patients without complications (0.4±0.1) was significantly less than in patients with complications (2.3±0.6) (p<0.05). Similar results seen in Kumar et al.15
REFERENCES
Policy for Articles with Open Access
|
|
 Home
Home