|
Table of Content - Volume 20 Issue 3 - December 2021
Evaluation of treatment of fracture neck femur with uncemented HA coated modular bipolar prosthesis
Mohd Abdul Naser1, Pramod Tupe2*, Abrar Mapkar3
1Associate Professor, 2Assistant Professor, 3Junior Resident, Department of Orthopaedics, Indian Institute of Medical Science & Research, Jalna-431202, Maharashtra, INDIA. Email: abrarmapkar@gmail.com
Abstract Background: Background: Fracture of the femoral neck has been reported with increasing incidence in recent times due to prevalence of osteoporosis. Uncemented HA coated modular bipolar hemiarthroplasty systems provide a customised press fit solution which improve the patient outcome with respect to limb length discreptancy. We report our series of 15 cases of fracture neck of femur operated over years with modular cementless HA bipolar hemiarthroplasty. Methods: 15 patients (age=50 to 70 years) with displaced femoral neck fractures were operated between January 2019 to December 2019. Cementless HA coated modular bipolar hemiarthroplasty using hydroxyapatite coated stem was done by single surgeon using same implant in all the patients through Moores approach. Clinical and radiological follow-up was done. Results: Total 15 cases with fracture neck femur were operated. The average follow up was 48 months. No intraoperative mortality was seen. 1 patient had calcar fracture of femur during canal preparation. 1 patient had delayed transient sciatic nerve palsy, and 1 patient had insignificant limb length discripency (0.5 cm). 12 patients reached to pre-injury status with average harris hip score of 88 at final follow up. Conclusions: Cementless bipolar hemiarthroplasty with hydroxyapatite coated stem is a good option for femoral neck fractures in elderly patients. Keywords: Uncemented, Elderly, Fracture neck femur, Modular Hemiarthroplasty, HA Coated.
INTRODUCTION Femoral neck fractures in elderly people result in a poor quality of life with impaired mobility and increased morbidity and inability to perform day to day activities. Sedentary lifestyle leading to a high prevalence of osteoporosis has lead femoral neck fractures to assume a major public health concern. Prosthesis as Arthroplasty was introduced by Judet et al.1 for various hip pathologies. Hemi arthroplasty is one of the most commonly done procedure for fracture neck of femur in elderly. It has provided satisfactory results in terms of pain relief, early return to pre-fall activity, reduced mortality and morbidity compared to osteosynthesis.2-4 A wide variety of cemented and un cemented versions of hemi arthroplasty are being used worldwide with debate about advantages between the two still going on5. Uncemented stem fixation lead to increased incidence of thigh pain. To address this, bioactive coating has been added to un cemented component to enhance the fixation by osseo integration of implant, of which hydroxyapatite (HA) was the most popular one. Cemented prostheses are associated with high success6 rates, but the possible effects of cement on the cardiopulmonary system, possibilities of venous and pulmonary embolization and the greater technical challenge to revision of cemented prosthesis has led surgeons to prefer un cemented implants.7-8 However Osteoporotic bone in elderly makes it difficult for the prosthesis to hold in cement less prosthesis and increases the incidence of complications like peri prosthetic fractures.9-10 HA coating accelerates bone healing and enhances the biologic fixation of implant due to its biocompatibility and osteoconductive potential. Several studies have shown that it could reduce the migration of HA-coated prosthetic components and have better results and higher survival rate than identical press-fit components.11
METHODS This retrospective clinical study was conducted on 15 patients with femoral neck fracture, operated using uncemented HA coated modular bipolar prosthesis by orthopaedic surgeons at a tertiary trauma care centre in the Department of Orthopaedics, Indian Institute of Medical Science and Research, Noor hospital, Jalna 431202 between Jan 2019 to July 2019. Fracture patterns were classified on basis of Garden12 classification of intracapsular proximal femur fractures. Inclusion criteria: 1.Patients> 50 years of age. 2.Intracapsular proximal femur fracture. 3.Closed fractures. Exclusion Criteria: 1.Neurovascular compromise. 2.Compound fractures. 3.Non united fractures. 4.Polytrauma patients. Surgical Methodology: Preoperative planning: Pre-Operative Investigations. And A dose of IV antibiotics (Inj. Cefuroxime) was given 30 minutes before the surgery13 Operative Procedure: Uncemented Modular HA coated Hemiarthroplasty using Moores approach.14 Post-Operative: Patients were asked to remain supine for the first 24 hours after surgery to reduce incidence of PDPH.patients were encouraged to mobilise using orthosis such as walkers after the first postop day.They were advised to abstain from squatting and sitting cross legged. Suture removal was done after 15 days. Pelvis with both hips radiographs were taken on the first postoperative day. All the surgeries were done in combined spinal-epidural anesthesia. The stability in the axial and rotational plane was assessed intraop with trial prosthesis before insertion of definitive prosthesis. All the patients were put on intravenous antibiotics for 5 days after surgery, followed by oral antibiotics for further 10 days. Progression to full weight bearing was at 6 weeks in most of the patients. Patients were reviewed postoperatively at 2 weeks, 6 weeks, 3 months, 6 months, 12 months, and then yearly. Harris hip scores15 and pain scoring with the visual analog scale were used as clinical outcome measures. Radiological evaluation included standard anteroposterior and lateral radiographs was done preoperatively then at first POD,3 months, 6 months, 12 months. Thereafter yearly X rays were done for evidence of stem subsidence, lysis, or loosening, acetabular erosion, protrusion or heterotopic ossification.
RESULTS Total 15 patients with 9 female and 6 male patients were included in the study. The range of age group varied from 50 to 70 years with mean age of 62 years. 1. Distribution according to Age: The mean age of patients was 63 years (range 50-70 years). Table 1: Age Distribution
2. Distribution according to Sex: There were 9 females and 6 males. Females were dominant in this case study. Table 2: Sex Distribution
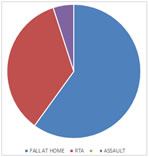
3.The mechanisms of injury included Road traffic accident in 5(35%), fall when walking and from height in 9(60%), assault in 1(5%). Fall from height was the most common cause of injury. Table 3: Mode of injury Distribution
4.The following table enlists the various intraop complications.There was minor splitting of the femoral calcar while inserting the definitive prosthesis in one patient.He was mobilised with a delay of 3 weeks and went on to recuperate uneventfully. Table 4: Intraop complications
5.The following table enumerates the postoperative complications in our enlisted patients.1 patient had an insignificant limb lengthening of <0.5cm. 1 patient developed a delayed transient sciatic nerve palsy16 3 weeks postoperatively.He regained normal function of the limb 6 weeks postoperatively. Table 5: Postoperative complications
Figure 1: Left side fracture neck of femur Figure 2: Immediate postoperative xray.
DISCUSSION The goal of an orthopaedic surgeon in management of hip disorder is a pain free hip with adequate strength and mobility to permit normal activities and function. Hemiarthroplasty is the most commonly performed surgery in fracture of the femoral neck as a lack of cambium layer and the synovial fluid of the hip joint resist union of the native femoral head with the shaft. Cemented hemiarthroplasty has advantage of early postoperative mobility because it provides early stability. Cementing of femoral stem increases the perioperative mortality due to cardiopulmonary complications like fat embolism, cardiac arrhythmias, hemodynamic abnormalities and even sudden death17. Cementing increases chances of fat embolism and also causes bone cement implantation syndrome (BCIS) which manifests as hypoxia, hypotension, and unexpected loss of consciousness, bradycardia and even cardiac arrest.The primary finding is that HA coating could improve the postoperative Harris Hip Score, reduce the incidence of thigh pain, and reduce the incidence of femoral osteolysis. Many studies have shown statistically significant increase in mortality in cemented hemi arthroplasty as compared to uncemented hemiarthroplasty18. Uncemented modular HA coated hemiarthroplasty had advantages of decreased operative time,less bleeding and lower incidence of thigh pain in comparison to cemented hemiarthroplasty. One of the most significant results of our analysis is that HA coating had less incidence of thigh pain. The advantage of an HA coating includes superior proximal femoral osseointegration and better preservation of periprosthetic bone quality. The patients with HA-coated stems demonstrated significantly lower incidence of activity-related trochanteric and thigh pain.19 The thickness and purity of HA and implant design could affect the incidence of thigh pain. The debatable point in elderly people with weaker bone stock is whether cementless stem will hold in the weaker osteoporotic bones as most of the studies have shown increased complications like periprosthetic fractures, dislocations, subsidence etc with cementless hemiarthroplasty. However, in most of such studies the comparative results are with older prosthesis. With porous or hydroxyapatite coated stems osteointegration occurs even in weaker osteoporotic bones as reported by many authors. In our operative experience we observed that with improved stem designs even in osteoporotic bones tight fit can be achieved. HA coating could increase the amount of ingrowth and attachment of bone leading to the enhanced biological fixation.20 Moreover, HA-coated Ti implants can achieve a much higher degree of bone apposition and mechanical stability compared to the implants without such a coating.21 We in our study prolonged full weight bearing by 6weeks. However by 3 months after surgery 12 out of 15 had reached pre injury activity level. Two patients continue to use walking stick because of physiological weakness.
CONCLUSION In conclusion, HA coated modular bipolar prosthesis could improve the postoperative HHS, reduce the incidence of thigh pain, and reduce the incidence of femoral osteolysis, while there was no statistical difference of femoral stem survivorship from aseptic loosening, polyethylene wear, and radiolucent lines. Results with respect to stability of implant, thigh pain, periprosthetic fractures and HHS are satisfactory and comparable to the latest literature on cemented hemiarthroplasty.
REFERENCES
Policy for Articles with Open Access
|
|
 Home
Home