|
Table of Content - Volume 21 Issue 1 - January 2022
Novel method of unilateral instrumental stabilisation with transforaminal debridement and fusion of lumbosacral tuberculosis
Anil kumar D N
Associate Professor, Department of Orthopaedics, Ayaan Institute of Medical Sciences, Hyderabad, INDIA. Email: anildn@gmail.com
Abstract Background: Tuberculosis of the lumbosacral junction is rare, accounting for approximately 3% of vertebral column tuberculosis In tuberculosis with extensive injuries of the lumbar spine and lumbosacral junction requiring long fusion to the sacrum, the loss of sacral bone for implant anchoring changes the fixation options suitable for these patients. Materials and methods: The study is retrospective observational study. Four patients were admitted due to lumbar and back pain. Three patients reported decreased lower limb weakness including 2 with grade II muscle power and 2 with grade III. Three cases had decreased knee and ankle reflex. Results: The mean operation time was (100.5 ± 24.2) minutes. The average intraoperative blood loss was (180 ± 50) ml. Intra operatively there was extensive destruction of pedicles and vertebral body noted at right side in three patients and one on left side, hence unilateral stabilisation was done on sound side. Conclusion: Along with conventional ante-tuberculosis medication, one stage posterior transforaminal debridement, autograft fusion and unilateral instrumental fixation is an efficacious and safe intervention for lumbosacral tuberculosis.
INTRODUCTION Tuberculosis of the lumbosacral junction is rare, accounting for approximately 3% of vertebral column tuberculosis.1,2 Common surgical interventions of spinal tuberculosis include surgical debridement, bone fusion and grafting, etc. The goals of surgical treatment of spinal tuberculosis are to accelerate nerve functional recovery, prevent spinal deformity and maintain spinal stability. Early-stage lumbosacral tuberculosis has been successfully handled with chemotherapy. For patients with advanced stage tuberculosis affecting extensive lumbosacral region, loss of lumbar lordosis and lumbosacral biomechanics should be scheduled to undergo surgery.3 The management of tuberculosis involved in the lumbar spine and lumbosacral junction is entirely different when treating the disease of either of these regions individually. The goals and principles of clinical treatment of extensive disease involving both the lumbar spine and the lumbosacral junction have been rarely described in the literatures.4 The instrumentation at the lumbosacral junction is technically demanding considering complicated topical anatomy, unique biomechanics characteristics and the difficulty in internal fixation adjacent to the affected bones. In this investigation, 15 patients diagnosed with lumbosacral tuberculosis were scheduled to receive posterior debridement, bone fusion, lumbar and sacral pedicle screw fixation or lateral internal fixation. Favorable clinical outcomes were obtained.
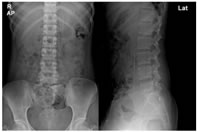
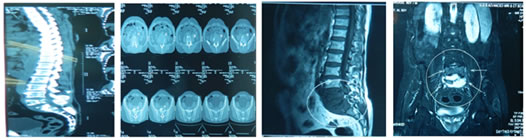
MATERIALS AND METHODS Baseline data The study is retrospective observational study conducted in Ayaan institute of medical sciences during december 2019 to march 2021. Among 4 patients 3 were male and 1 female, aged 17 to 67 years with a mean age of (40.6 ± 12.3) years. 2 cases had a medical history of pulmonary tuberculosis. Patients presented with varying degree of fever, night sweat and toxic symptoms induced by tuberculosis. Four patients were admitted due to lumbar and back pain. Three patients reported decreased lower limb weakness including 2 with grade II muscle power and 2 with grade III. Three cases had decreased knee and ankle reflex. Imaging diagnosis Preoperative X-ray (Figure 1), CT scan (Figure 2A) and MRI (Figure 2B) examination revealed that L4-S1 vertebral involvement in 1 patient, L5-S1 in 3 cases. Imaging findings demonstrated the signs of intervertebral space narrowing in all cases. Bone destruction and sequestration were observed in the diseased vertebrae. Cold abscess formation was noted in the psoas muscle. Presacral abscess noted in two cases.
Figure 1: Preoperative anterolateral X-ray revealing the narrowing of intervertebral space among L5-S1 vertebra.
Figure 2: Preoperative CT scan (A) and MRI (B) displaying the L5-S1 vertebral injury and intervertebral space narrowing Figure 3: Postop x-ray
Preoperative preparation Prior to operation, all patients underwent X-ray, CT scan and MRI examination of the lumbosacral region. Laboratory tests were performed. Nutrition supporting therapy was delivered simultaneously. Surgical intervention The patients received endotracheal intubation under general anesthesia in a prone position. The median incision was made, the supraspinal ligament was preserved and the diseased vertebra and two surrounding vertebrae were exposed. Decompression management was delivered at the side with extensive abscess, and intact vertebral lamina, zygapophysial joints and joint capsule were retained at the contralateral side and unilateral pedicle screw instrumentation done... After proper internal fixation, the radian between the lumbar and sacrum almost returned to normal the nerve root was carefully protected. Subsequently, through transforaminal approach... The abscess fluid was discharged. The necrotic and granulation tissues were thoroughly removed until healthy endplate surface. The autologous iliac bone was implanted in the vertebra or the vertebral defect. And the incision was sutured in layers over drain
Postoperative management Conventional antibiotics therapy was delivered via intravenous drip for 48 h. Liver protection therapy and nutritional support treatment were strengthened. Administration of albumin was delivered when necessary. Postoperative nursing care should be enhanced to prevent the incidence of deep vein thrombosis and other postoperative complications. After confirming the diagnosis by HPE and GEN X PERT ante tubercular treatment stared by daily regimen and for 12 months treatment was continued in all the four case which they tolerated well, the drainage tube was removed when the drainage volume declined below 50 ml/d. On a regular basis, all patients were required to receive routine blood test, liver and kidney function test, erythrocyte sedimentation rate test and detection of C-reactive protein levels with a time interval of 5 to 7 d. At approximately 1 week after surgery, the patients remained physically stable and were advised to do physical activities using brace protection for 6 to 8 months. X-ray imaging test was performed to evaluate the status of bone fusion once every 3 months.
RESULTS The mean operation time was (100.5 ± 24.2) minutes. The average intraoperative blood loss was (180 ± 50) ml. Intra operatively there was extensive destruction of pedicles and vertebral body noted at right side in three patients and one on left side, hence unilateral stabilisation was done on sound side. All patients were followed up for 14 to 18 months. Preoperative neurology muscle power was grade II in two patients and grade III in other two. At the final follow up all four patients recovered fully with good evidence of fusion across segment All patients presented with neither Dural nor the great artery injuries. There was no wound and implant related complications No sinus tract was formed. For male patients, no symptoms of retrograde ejaculation occurred. Pathological diagnosis results confirmed the incidence of chronic inflammatory changes accompanied by sequestration. Erythrocyte sedimentation rate and C-reactive protein levels returned to normal range after anti-tuberculosis treatment for 2 to 6 months. The bone fusion rate achieved up to 100%. No signs of loosening internal fixation were observed. According to the criteria of bone tuberculosis healing,4 all patients were completely recovered. No indications of tuberculosis recurrence were documented.
DISCUSSION Clinical treatment of tuberculosis of the lumbosacral junction remains a controversial and challenging task for surgeons. Few studies have been performed focusing on the surgical intervention in advanced lumbosacral junction tuberculosis. Previous studies5-7 have reported that patients receiving non-surgical treatment developed a high incidence of kyphosis associated with trunk shortening. Advanced-stage tuberculosis with extensive destruction of the lumbosacral spine leads to the occurrence of kyphosis or hypolordosis, accompanied with back pain and difficulties during childbirth. Due to complicated local anatomy, the unique biomechanics, and difficult fixation in the surrounding diseased bone, instrumentation at the lumbosacral junction is highly technically demanding. In tuberculosis with extensive injuries of the lumbar spine and lumbosacral junction requiring long fusion to the sacrum, the loss of sacral bone for implant anchoring changes the fixation options suitable for these patients. In this investigation, 4 patients diagnosed with lumbosacral tuberculosis were scheduled to undergo posterior transforaminal debridement, bone fusion, unilateral lumbar and sacral pedicle screw fixation. Lumbosacral tuberculosis is adjacent to the rectum, iliac vessels and ureter, where the abscess is likely to form. Hence, thorough removal of the diseased tissues is a highly demanding task. In addition, inflammation is involved with surrounding nerve vessels, which enhances the tissue fragility, increases the risk of vascular injury and elevates the incidence of retrograde ejaculation after sympathetic nerve damages. Therefore, in our experience, we were not expected to thoroughly eliminate the granulation tissues in front of and bilateral to the vertebra to avert the incidence of vertebral injury. The abscess fluid was discharged as possible. Meantime, the necrotic tissues between the vertebra and invading into the vertebral canal should be fully eliminated, which could enhance the bone fusion rate and accelerate nerve functional recovery. In this study, neither the great artery injury nor retrograde ejaculation occurred before, during and after the procedures. All patients presented with bone fusion The goals of conventional treatment of lumbosacral tuberculosis are to correct and prevent a lumbar kyphosis, decompress the neural elements, restore or preserve a normal lumbosacral angle, and maintain the vertebral height and global spinal stability. Due to the complex lumbosacral anatomical structure, posterior surgery has been widely accepted as an ideal surgical approach, which can thoroughly eliminate the lesions, proper vertebral canal decompression and effectively support the bone graft.8-10 Anterior debridement and fusion with a strut graft can prevent and lessen a kyphosis, but there is a high incidence of graft-related problems, such as high incidence of the great artery injury, limited correction angle, difficulty in internal fixation and slow rehabilitation. Another common option is anterior debridement, bone grafting combined with posterior internal fixation, which not only incorporates the advantages of anterior surgery, but also supports the spine using three columns. Application of this approach can reconstruct the spinal stability, decrease the incidence of bone graft slippage and collapse, and enhance the bone fusion rate.11-12 In addition, anterior combined with posterior approach requires long operation time and yields severe surgical injury, which is not applicable to the elderly patients diagnosed with lumbosacral tuberculosis. In this investigation, posterior transforaminal debridement, bone grafting combined with unilateral internal fixation is not one of the conventional options for treatment of lumbosacral tuberculosis. However, it has multiple advantages of small surgical trauma, short operation time and three column supporting force, etc. It is suitable for patients with slight vertebral collapse, mild lumbar kyphosis, slight abscess surrounding the vertebra, lesions located between two vertebrae or at the posterior margin of the vertebra.13-14 Nevertheless, the scope of lesion elimination is constrained, especially the diseased tissues in front of or on the contralateral side of the diseased vertebra. It is not applicable to those with extensive destruction of the spine and lumbosacral junction. Therefore, prior to the formal surgery, those with severe and extensive involvement of lumbosacral tuberculosis were excluded from the subsequent surgical procedures. Our experience obtained from this clinical trial reveals that similar to other types of tuberculosis; anti-tuberculosis medication therapy remains the fundamental treatment for lumbosacral tuberculosis. It is not required to eliminate all the diseased bone within the vertebra, whereas the abscess fluid outside the vertebra should be thoroughly discharged and completely irrigated using normal saline solution. Another advantage of posterior approach is that it merely destroys unilateral articular process and vertebral lamina, but retains the joint capsule of the adjacent articular process and exerts no influences upon the spinal stability. In this investigation, all patients had successful bone fusion, no incidence of grafting slippage or kyphosis. The principles of our screw use in this study are that the screws with unilateral fixation can be utilized for patients without risk of developing post op kyphosis in properly selected patients with adequate ante tubercular treatment...
CONCLUSION Along with conventional ante-tuberculosis medication, one stage posterior transforaminal debridement, autograft fusion and unilateral instrumental fixation is an efficacious and safe intervention for lumbosacral tuberculosis.
REFERENCES
Policy for Articles with Open Access
|
|
 Home
Home