|
Table of Content - Volume 21 Issue 1 - January 2022
A study of dynamic hip screw fixation for trochanteric fracture of femur at a tertiary health care centre
Sagi Radha Krishna Rao1, Pankaj Kabra2*
1,2Assistant Professor, Department of Orthopaedics, Surabhi Institute of Medical Sciences, Mittapally Village, Siddipet Mandal And District, Telangana State, INDIA.
Abstract Background: Hip fractures are leading cause of morbidity and mortality in the elderly population. Hip fractures lead to most severe health problems and reduced quality of life. Aim and objective: To study the effectiveness and complications of dynamic hip screw fixation for trochanteric fracture of femur at a tertiary health care centre Material and methods: Present study was a prospective study carried out patients with intertrochanteric fracture of femur. Data included sociodemographic data, clinical history and through clinical examination. All patients were treated with Dynamic Hip Screw fixation. Outcome and complications were noted. Results: Salvati Wilson Hip evaluation, Excellent score (>31) was observed in 30% patients. Good score (24-31) was seen in 43.33% patients. Position of implant at follow up remained same in 28 (93.33%) patients. one patient had coxa vara and one had loosened screw. Mean time taken for full weight bearing was 12.1±2.3 weeks.
INTRODUCTION Increase in elderly population of the world leads to increased incidence of hip fracture. There were an estimated 1.66 million hip fractures world-wide in 1990, the number of hip fractures is expected to reach 512,000 in the year 2040.1 intertrochanteric fractures contribute 50% to fractures around hip. Cause of injury in 90% of intertrochanteric fractures is through osteoporotic bone (elderly patients) due to simple fall.2,3 Other causes are Road Traffic Accidents and fall from height.3 These fractures are associated with significant morbidity and mortality. 30% of elderly patients die within 1 year of fracture. It affects quality of life of a person. So these fractures should be treated effectively. Rigid fixation with early mobilization of the patient is the goal of treatment in intertrochanteric fracture of femur. Restoration of mobility in patients with intertrochanteric fracture ultimately depends on strength of surgical construct. Many devices can achieve rigid fixation in intertrochanteric fracture but the Dynamic Hip Screw is the most commonly used device.4 The DHS lag screw easily glides within DHS plate barrel for controlled collapse and impaction of fragments leading to uneventful healing and early mobilization.5 As intertrochanteric fractures are most commonly observed in elderly population, more care and effective treatment is needed. A combination of orthopaedic surgery and early postoperative physio therapy and ambulation is the best approach for these fractures. Present study was conducted to see the effectiveness and complications associated with Dynamic Hip Screw fixation in intertrochanteric fractures. Aim and objective: To study the effectiveness and complications of dynamic hip screw fixation for trochanteric fracture of femur at a tertiary health care centre
MATERIAL AND METHODS Present study was a prospective study carried out in department of Orthopaedics at a tertiary health care centre. Study population was patients with trochanteric fracture of femur. Inclusion criteria: 1.All fractures of trochanter as classified by Boyd and Griffin stable ,unstable and comminuted fractures 2.Fractures of trochanter above age of 18 years 3. Patients willing to participate in the study Exclusion criteria: 1. Compound fractures associated with vascular injuries, ipsilateral shaft fractures and pelvic fractures 2. Old malunited fractures 3. Trochanter fractures associated with neck of femur/head of femur. 4. Trochanter fractures associated with shaft of femur 5. Trochanteric fractures associated with dislocation of hip/knee Study was approved by ethical committee of the institute. A valid written consent was taken from the patients after explaining study to them. Data was collected with pre tested questionnaire. Data included sociodemographic data, clinical history and through clinical examination. Routine blood investigations like, Complete blood count, urine routine, bleeding and clotting time, blood urea, serum creatinine, random blood sugar, Electro cardiograph (ECG), chest X-rays were done in all patients. Pre anaesthetic check up was done in all patients. Incision was made over proximal femur laterally beginning from the middle of the greater trochanter extending distally. By retracting, vastus laterals muscle and its origin from the inferior border of the greater trochanter. Exposed vastus laterals is then divided near linea aspera. The vastus laterals muscle retracted posteriorly and then perforating branches of profunda femoris identified and ligated. After dividing muscle along the femur for required distance, it is elevated with a periosteal elevator and lateral and anterolateral surfaces of femoral shaft exposed. Point of insertion was made at lateral aspect of femoral shaft midway between anterior and posterior cortices approximately 2 cms below the flare of grater trochanter (i.e. vatus lateralis ridge). An entry point was made using power drill with the help of image intensifier. Using fixed/dynamic angle guide measuring 130/135/140, guide pin mounted on a T handle inserted till the resistance is felt. A 130/135/140barrel plate was secured to femoral shaft and fixed with 4.5mm cortical screw. Compression screw is then inserted into the distal end of lag screw and tightened to compress the fracture after release of the traction. Final position is conformed, joint movement checked passively (for short movements). Wound washed thoroughly and closed in layers and sterile dressing applied over a suction drain in required cases. Clinical evaluation was done assessment for pain, swelling, infection and mobility, deformity, wound status, limb length, walking ability determined on follow up. Radiographic assessment was done at each visit to see Normal and stable fracture union, Migration of screw, Cutting out of screw and Implant failure. Clinical evaluation was done assessment for pain, swelling, infection and mobility, deformity, wound status, limb length, walking ability determined on follow up. Salvati and Wilson hip scoring system was used for evaluation. Patient was initially observed in the recovery room later shifted to ward. Adequate analgesics, I.V antibiotics given up to 72 to 48hours post operatively. Post OP check X-rays obtained. After Parenteral antibiotics oral antibiotics were administered till sutures removed. Oral antibiotics were continued after discharge if infection was found. Drain was removed at end of 24 hours. Wound inspected at 2nd post op day. Alternate suture removal done and by 10th day all sutures were removed. Patient was made to sit up on bed and Static quadriceps exercises started from 2nd day. Patient were followed up regularly upto 6 months after discharge. Partial weight bearing allowed from third week and full weight bearing from sixth week with walker. Data was entered in excel sheet and analysed with SPSS version 20.0.
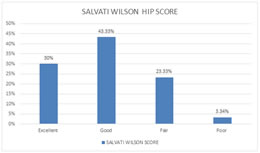
RESULTS In our study, we studied total 30 patients. Majority of the patients 10(33.34%) were from the age group of 71-80 years followed by 61-70 years 07(23.33%). Patients in the age group of 31-40 years were(2) 6.66%. None of the patient was below 20 years. Male and female follow the same pattern of age distribution. In our study, out of total 30 patients, 19 (63.33%) were male and 11(36.67%) were female. male to female ratio was 1.72:1. (table 1) In our study, right sided fracture were 17(56.67%) and 13 (43.33%) fracture were of left side. Out of 30 patients, Fall was most common reason for injury seen in 26(86.67%) patients. RTA was seen in 4(13.33%) patients. We found more cases were displaced intertrochanteric fractures Type II (46,67%) common in the present study followed by type III fractures (23.33%). 20% fractures were type IV and 10 % were type I fractures. (fig 1) During immediate postoperative X-ray by position of implant majority had central position 21(70%) then posterior 6(20%) and least were found in superior 3(10%). Table 2 shows Distribution of patients according to post operative wound complications. Normal healing was seen in 26(86.67%) patients. superficial infection was observed in 2(6.67%) patients. These patients were treated with higher antibiotics. Delayed healing was observed in one patient with deep infection but healed well after debridement and IV antibiotics for 3 weeks. One patient had bed sores. The mean duration of hospital stay for the patients was 15.7±3.8 days. Table 3 shows Distribution of patients by postoperative complications at 6 months follow up. In our study, Majority of the patients complained of pain. Occasional pain was seen in 20%(6) patients and mild to moderate pain was seen in 3.33% (1) patients. Pain was relieved by medications. Limping was seen in 5(16.67%) patients. knee stiffness and shortening was seen in 2(6.67%) patients each. Coxa vara was observed in one patient. Knee stiffness improved by physiotherapy. Fig 2 shows distribution of patients according to Salvati Wilson Hip evaluation. Excellent score (>31) was observed in 30% patients. Good score (24-31) was seen in 43.33% patients. Fair score (16-23) was seen in 23.33% patients. Poor score (<16) was seen in 3.34% patients. 27 (90%) patients had score above 20. In our study, position of implant at follow up was remained same in 28 (93.33%) patients. one patient had coxa vara and one had loosened screw. Mean time taken for full weight bearing was 12.1±2.3 weeks. We find most of the patients 13(43.33%) were able to bear weight between 12 and 15 weeks. (Table 4)
Table 1: Distribution of patients according to age group and sex
Table2: Distribution of patients according to post operative wound complications
Table 3: Distribution of patients by postoperative complications at 6 months follow up
Figure 1: Distribution of patients according to SALVATI WILSON HIP SCORE
Table 4: Distribution of patients according to Time taken for full weight bearing
DISCUSSION In our study, we studied total 30 patients. Majority of the patients 10(33.34%) were from the age group of 71-80 years followed by 61-70 years 07(23.33%). Similar results were seen by RC Gupta et al.5 and Mohanty SP et al.6 where they noted majority patients were above 60 years. In our study, Male to female ratio was 1.72:1. GS Kulkarni 7 et al. found 55% patients were female and 45% were male. In our study, right sided fracture were 17(56.67%) and 13 (43.33%) fracture were of left side. Similar to our study, Right sided fractures were more in study by Wade P A and R C Gupta et al.5 Contrast to our study, by Cleveland et al. observed left sided fractures commonly. Out of 30 patients, Fall was most common reason for injury seen in 26(86.67%) patients. RTA was seen in 4(13.33%) patients. We found more cases were displaced intertrochanteric fractures Type II (46.67%) common in the present study followed by type III fractures (23.33%). These results are comparable with Arun K umar Singh et al.2 in which Type II were common followed by Type III and Type IV. During immediate postoperative X-ray by position of implant majority had central position 21(70%) then posterior 6(20%) and least were found in superior 3(10%). Similarily Mulholland and Gunn et al. had same observation and they recommended central placement of screw. Significant association was observed with implant position. Superior position was associated with implant failure cut out and other complications. The mean duration of hospital stay for the patients was 15.7±3.8 days. Richard F Kyle 9 observed that mean duration of stay was 18 days. In our study, Majority of the patients complained of pain. Occasional pain was seen in 20% (6) patients and mild to moderate pain was seen in 3.33% (1) patients. Limping was seen in 5(16.67%) patients. knee stiffness and shortening was seen in 2(6.67%) patients each. Excellent score (>31) was observed in 30% patients. Good score (24-31) was seen in 43.33% patients. 27 (90%) patients had score above 20. Al- Yassan et al. observed that 78% patients had scores above 20 points. 10 Two cases had implant failure. GS Kulkarni et al. found failure rate of 6.3%.7
CONCLUSION Dynamic hip compression screw an effective device with less complications for the treatment of trochanteric fractures.
REFERENCES
Policy for Articles with Open Access
|
|
 Home
Home