|
Table of Content - Volume 22 Issue 1 - April 2022
Outcome of Gartland Type III supracondylar fracture humerus in children
Atul A Kharat1, Mohan Murade2, Pravin Padalkar3*
1,2Assistant Professor, Department of Orthopaedics, Dr NYT IMS Medical College, Karjat, Maharashtra, INDIA. 3Professor, Department Orthopaedic Surgery, BKL Walawalkar Medical College, Dervan, Chiplun, Ratnagiri, Maharashtra, INDIA. Email: drpravinpadalkar@yahoo.com
Abstract Background: This study was undertaken to evaluate and compare clinico-radiologically the results of two most common methods of treatment namely, closed reduction and immobilization in plaster slab versus closed reduction and percutaneous K wire fixation and also to study the complications of the management Materials and Methods: the study “a comparative study of management of displaced Gartland type III supracondylar fracture humerus in children (closed reduction and plaster immobilization versus closed reduction and percutaneous pinning)” was carried out during the period of August 2017 to July 2019 in the department of orthopaedics. The age of the patient was from 4 to 12 yrs, with follow up ranging from 3 months to 1 year. A total of 98 cases were enrolled for this study. 14 cases were lost in follow up and only 84 patients completing the minimum follow up of 3 months were considered for analysis of observations and results. Out of these 84 patients 54 were treated with closed reduction and K wire fixations while remaining 30 were treated with close reduction only and all the patients were immobilised with above elbow slab. Results: Patients were followed up at regular intervals and at each follow-up radiographs were done. Flynn's criterion was used for assessing the functional outcome. As per these criteria 88 % cases of CR+ K wire group had excellent to good results while 67 % cases of CR + slab group had excellent to good results. No case of poor result was noted in k wire group. There were few complications such as elbow stiffness and cubitus varus deformity and tightness of compartment post surgery. These were more common with patients with slab Conclusion: Our study states that K wire fixation is superior over just plaster immobilization in terms of improved functional outcome and lesser complications. Keywords: Gartland, supracondylar, humerus fracture, children.
INTRODUCTION Supracondylar fracture of humerus is the most common elbow injury seen in children. Fall on outstretched hand is the most common mode of injury, which occurs in children during playing, running and fall from bicycle. Displaced supracondylar fracture humerus in children may be associated with other fractures of upper extremities depending on the mode of injury. An apparently uncomplicated fracture may lead to complication if not treated properly. This fracture occurs in the area, where brachial artery and three nerves of upper extremity are in close vicinity.1 Hence these structures are liable to get injured as a result of displaced fracture. It may be associated with swelling, limb threatening Volkman ischemia and nerve palsies on presentation and may lead to stiffness of elbow and cubitus varus deformity of elbow.2 Goals of treatment of supracondylar fracture are to achieve an excellent, functional and cosmetic result without complication.3 Many methods of treatment have evolved in management of supracondylar fracture humerus in children. These are closed reduction and immobilisation in plaster slab, closed reduction and percutaneous kirschner wire fixation, open reduction and internal fixation, Dunlop traction, olecranon traction etc.2 This study was undertaken to evaluate and compare clinicoradiologically the results of two most common methods of treatment namely, closed reduction and immobilization in plaster slab versus closed reduction and percutaneous k wire fixation.
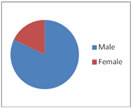
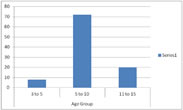
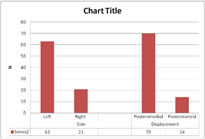
MATERIAL AND METHODS Type of study: Prospective Duration: August 2017 to July 2019 Inclusion Criteria Traumatic suprocondylar fractures with Type III Gartland, patients willing to participate in the study. The cases were grouped in two as follows. Group I: Even no cases treated with closed reduction and K wire fixation. Group II: Odd no of cases treated with closed reduction and plaster slab Group I 54 cases (37+8*+9**) and Group II 30 cases constitute the material for this study. The difference in the number of cases in the two groups is due to * 8 cases of unstable reduction with plaster slab, K- wire stabilization was done and patient included in Group I fixation. ** 9 cases of suspected of compartment syndrome were treated by CR and K wire fixation. Exclusion Criteria Type I and Type II Gartland fractures, Pathological fractures, other fracture involving the same extremity, patients not willing to participate in the study were excluded Patient followed at 1, 3, 6, 9, and 12 months and each follow-up results were assessed using Flynn's criteria.4 Table 1: Sex Distrubution in Table 2: Age group Involved in series series Table 3: Side and displacement of fracture pattern
RESULTS In the present study 98 cases of Gartland type III supracondylar fracture humerus were enrolled. Only 84 cases were taken for final results analysis as they had completed the minimum follow up of 3 months. Out of 14 cases lost in follow up, 11 were in CR+ slab group and 3 were from CR + K wire group. Out of 84 cases considered for results 54 belonged to CR + K wire group and 30 cases were of CR+ slab group. The following observations of the study are based on the follow up of 84 cases only. Around 72% patients were between 5 to 10 years of age and 82% were boys. Left side injury was 3 times commoner than right. Fall on outstretched hand was common mechanism of injury (60%). Poster medial displacement was 5 times commoner than poster lateral. 5 patients had associated distal radius fracture while vascular compromise was seen in 7 patients and one patient had nerve injury. 81% patients were treated with lateral 'K' wire fixation. 76.19% patients were having metaphyseo-diaphyeal angle between 85-100 postoperatively, indicating good reduction of fracture. However, values less than 85 and above 100 in a total of 20 cases were accepted. It was found that incidence of stiff elbow and cubitus varus was more common in patients treated with slab group (6.66%). Around 87.03 % cases treated with 'K' wire had less than 10-degree loss of range of motion. While this percentage was 56.66 % in cases treated with plaster slab alone. 6.66% (2) cases managed with slab had cubitus varus while none case of K wire group had cubitus varus. Thus showing overall results are better in 'K' wire group. As per Flynn's criteria 88 % cases of CR+ K wire group had excellent to good results while 67 % cases of CR + slab group had excellent to good results. No case of poor result was noted in k wire group while 2 patients in slab group had poor outcome.
DISCUSSION The average age incidence in the present study is consistent with other studies and shows that supracondylar fracture of humerus of immature skeleton is common during the end of first decade. This was consistent with other studies. Many studies have shown incidence of fracture higher in boys than girls same observations were made in our study. Involved site in literature was non-dominant side it was same in our study as well. Fall over outstretched hand was more common mechanism of injury. Palmer et. al (1978) in series of 78 patients of supracondylar fractures of the humerus showed 5.2% (4 cases) were having ipsilateral fracture of the lower end of the radius.5 In 1988, Pirone and Graham in their series found 9% of cases of other ipsilateral fractures.6 In the present study of 84 cases, 5.95% (5 cases) patients were associated with ipsilateral fracture of distal end radius. Pirone AM et al. (1988) observed posteromedial displacement in 68.61% cases, posterolateral in 16.05% cases and directly posterior displacement in 15.32% cases.6 In the present study of 84 cases, 80.9% (68 cases) had posteromedial displacement, 16.6 %( 14 cases) had postero lateral displaced and 2.38 % (2 cases) anterior displacement. Posteromedial: posterolateral = 5:1
CONCLUSION This study shows supracondylar fracture humerus to be more common in boys between 5-10 years' age, more on nondominant side and has posteromedial displacement. The study found that better maintaince of reduction by K wire fixation with better follow up and avoidance of complications of compartment syndrome, stiffness and cubitus varus in comparison to plaster slab. Clinical Message: This study tells that supracondylar fracture humerus is seen most commonly in non-dominant hand, most common age group is 5-10 years. K wire fixation with immobilization has better functional outcome than only immobilsation. REFERENCES
Policy for Articles with Open Access
|
|
 Home
Home