|
Table of Content - Volume 22 Issue 1 - April 2022
Evaluation of Type III and IV radial head fractures treated with radial head prosthesis: A retrospective study
Shreerang Joshi1, Akshay Bondar2*, Piyush Gaikwad3, Suyash Ingale4, Rohan Nagare5
1Professor & HOD, 2,3,4,5Junior Resident, Department of Orthopedics, B.K.L. Walawalkar Rural Medical College and Hospital, Sawarde, Ratnagiri, Maharashtra, INDIA. Email: akshaybondar1995@gmail.com
Abstract Background: Radial head fractures are one of the common fractures around the elbow. In recent times radial head is considered as an important stabilizer of the elbow, hence preserving or replacing it is gaining popularity for maintaining elbow stability. For type III and IV radial head fracture which cannot be fixed its excision has been practiced extensively. However it cannot be performed in case of associated ligament injuries. Radial head arthroplasty tries to solve these problems. Aim: To evaluate the functional outcome of type III and IV radial head fractures treated by radial head prosthesis. Materials and methods: In a retrospective study, 10 patients of type III and IV radial head fractures who were managed using modular radial head prosthesis from April 2018 to May 2021 at BKL Walawalkar rural medical college and hospital Dervan were included in the study. These cases were evaluated on basis of demographic variables, mechanism of injury, post-operative range of motion, complications and Mayo Elbow Performance Index (MEPI). Results: Most common age group in our study was <40 years (60% cases), female to males ratio was 2:1, fall was the most common mode of injury, right side was involved in 80% cases, 8 cases of type III and 2 of type IV were seen, range of motion improved significantly over 6 weeks period, MEPI was excellent in 7 cases (70%), good in 2 cases (20%), fair in 1 case (10%) and no case with poor result. Complications in 2 cases were noted, 1 case of elbow stiffness and 1 of infection which were treated successfully. Conclusion: Radial Head Prosthesis is a viable option in communited and irreparable radial head fractures. Proper preoperative planning, good Intraoperative technique and rigorous postoperative rehabilitation gives predictable results. Keywords: Radial head fracture, radial head arthroplasty, radial head replacement, fracture of elbow, modified mason’s classification, elbow dislocation, Mayo elbow performance index.
INTRODUCTION Radial head fractures account for almost 1.7% to 5.4% of all fractures and one third of all the elbow fractures. Most of these injuries are a result of fall onto an outstretched hand, high-energy injuries representing falls from height or during sports. This happens when radial head impacts with the capitellum. This may occur with a pure axial load, with a posterolateral rotatory force, or as the radial head dislocates posteriorly. It is frequently associated with injury to the ligamentous structures of the elbow.1 According to studies by the Mayo foundation, the medial collateral ligament (MCL) is the primary stabilizer of the elbow joint and the radial head is second in importance in the stabilization during loading and valgus stress.2 Therefore, from the biomechanical point of view, in the presence of injury of the MCL, coronoid fracture or lesions of the lateral collateral ulnar ligament (LUCL), the radial head is considered a structure of fundamental importance.3 Mason’s classification is most commonly used classification for describing radial head fractures. For type I fracture there is no doubt that it should be treated conservatively. Undisplaced or minimally displaced type II fractures can be managed conservatively in a manner similar to type I fractures.4 Acute mechanical block in displaced type II fractures is best treated by open reduction and internal fixation especially in young and active individuals.5,6,7 Type III comminuted fractures are high energy injuries and are currently treated by osteosynthesis or early complete excision of the radial head or radial head replacement. Type IV fracture-dislocation injuries should be treated by immediate reduction of the dislocation and treatment of the fractured radial head. The goal of operative treatment for radial head fractures, whether with open reduction and internal fixation (ORIF) or prosthetic joint replacement, is to avoid subluxation or dislocation of the elbow joint by recreating the radio-humeral joint to achieve stability and joint alignment.8 Resection of the radial head is usually done in older patients with complex isolated fracture. This also can be considered in fracture-dislocation without a fracture of the coronoid, in patients without signs of longitudinal or medial instability, in elderly or low demanding patients.9-13 In many studies, results and limitations of radial head excision have been described when used for treatment of complex fractures. In the long term it can lead to valgus instability, longitudinal instability, positive ulnar variance with pain in the wrist, lack of strength and appearance of ulnohumeral degenerative changes.14,15 Two recent prospective randomized trials have demonstrated improved outcomes in radial head prosthesis compared to osteosynthesis (ORIF) for complex unstable radial head fractures, with a greater frequency of complications in ORIF, such as premature failure of the synthesis and non-union.16,17 One of the study determines three fragments to be the cut-off number in order to proceed with prosthesis implant as the preferred treatment.18 The radial head prosthesis is intended to prevent proximal migration of the radius in response to axial loading of the forearm. It resists valgus and posterior elbow instability by providing effective radio capitellar contact that approaches that of the native radial head. It facilitates uneventful healing of the medial collateral and interosseous ligaments, as well as the distal radio ulnar joint.19 Because of the above mentioned complications, many orthopedic surgeons favour radial head arthroplasty as primary option of treatment in radial head fractures for Mason type III and IV.19 AIM: To evaluate the results of radial head replacement for type III and IV radial head fractures in terms of functional outcome.
MATERIALS AND METHODS We included 10 patients of type III and IV radial head and neck fractures according to Mason's classification. They were admitted and treated in the orthopedic department of B.K.L. Walawalkar rural medical college and hospital, Dervan with radial head prosthesis from April 2018 to May 2021. Severely comminuted fractures of the head and neck of radius i.e type III and type IV, skeletally mature patients, patients giving consent for the surgery were included in the study. Type I and type II fracture patterns that can be managed conservatively or by simple internal fixation, open fractures, other fractures around the elbow, presence of any infection, children with fracture of radial head and neck were excluded from the study. A well informed and written consent was taken from patient and relative in their local language. Pre-operatively patients were evaluated on admission, a detailed history including the mechanism of injury and complaints of the patients were noted, along with a thorough clinical examination. Radiographs of affected limb and contralateral normal limb in antero-posterior and lateral view were taken. For primary treatment immobilization was given in the form of above elbow slab. All routine investigations were done and pre-operative anaesthesia fitness was taken. Patient was posted for radial head replacement with radial head prosthesis. Templates were available to facilitate preoperative implant selection based on radiographs of the injured and normal contralateral elbow. Prophylactic antibiotics were given intravenously pre operatively 30 minutes before skin incision to cover the common bacteria associated with postoperative surgical infections. Under general or regional anaesthesia, the patient was positioned in the supine position. A sandbag was placed under the ipsilateral shoulder to assist in positioning of the elbow across the chest. The operative arm was placed over a padded bolster with a sterile tourniquet in place. After routine preparation and draping, Kocher approach was marked. Skin incision was placed. A full-thickness fascio-cutaneous flap was elevated. This exposure provided access to the radial head, capitellum, and lateral collateral ligament. The medial flap if needed was elevated to expose the coronoid and medial collateral ligament. The fascial interval between the anconeus and extensor carpi ulnaris was identified and developed.
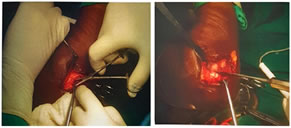
Figure 1: Kochers approach Exposure of radial head Figure 2: Excision of radial head Excision of the fragments of the radial head was facilitated with the use of an image intensifier and a pituitary rongeur. Generous joint irrigation was performed to remove all loose intraarticular debris. Varus, Valgus and axial stress tests were done to check LCL, MCL and interosseous ligament, to confirm need for radial head replacement. A modular radial head implant system was used. Measurement was taken after excision of radial head. Appropriate size press fit modular radial head prosthesis was inserted.
Figure 3: Measurement of radial head prosthesis Modular press Figure 4: Post op check xray fit radial head prosthesis in-situ
After radial head replacement the elbow was placed through an arc of extension while carefully evaluating for elbow stability in pronation and supination. Closed suction drain was used for 24 hours. Haemostasis was achieved and wound was closed in layers. If the elbow was stable it was splinted in full extension with anterior plaster slabs, avoiding pressure over the olecranon and wound. If there was some residual instability it was splinted in 900 flexion and supination. Postoperatively patients were given antibiotics and anti-inflammatory medicines for 3 days post op as per our institutional policy. The elbow was started with active flexion and extension exercises throughout a full arc of motion 3 days after surgery. A collar and cuff was worn during the day between exercises. A static progressive extension splint was used at night. Patient assessments was done of the basis of range of motion (ROM) at 2 and 6 weeks post op, stability and functionality was assessed according to the Mayo Elbow Performance Score (MEPS) at the final follow up. Statistical Data analysis was done using the SPSS (Statistical Package for the Social Science) Version 17 for windows. A p-value of 0.05 was accepted as the level of statistical significance.
OBSERVATION AND RESULTS: Table 1: Age distribution
Above table shows an age wise distribution of our study. Out of 10 cases, 6 cases were <40 years and 4 cases were >40years (40%). The mean age was 39.8 years. Maximum age was 56years, minimum age was 30 years.
Table 2: Sex distribution
Out of 10 patients majority were females i.e 7 cases and 3 were males.
Table 3: Mechanism of injury
The above table tells us about the mechanism of injury most of the cases i.e 70% were due to history of fall and remaining were due to RTA. Table 4: Side dominant distribution
The above table, shows that in our study, 8 cases (80%) were right side dominant and 2 cases (20%) were left side dominant.
Table 5: Mason's classification
Above table shows that in our case study group out of 10 cases, 8 cases (80%) were under Modified Mason's classification type Ill and 2 cases (20%) were under Modified Mason's classification type IV. Table 6: Associated injury wise distribution
Above table shows that in our study group out of 10 cases, 8 cases, (80%) were not associated with any ligamentous injury, 1 case of each LUCL and MCL injury was noted.
Table 7: Post operative flexion at 2nd and 6th post op week in study group
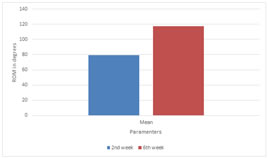
The table and bar diagram shows that the mean flexion at 2nd week post-op was 79.33 degrees which improved to 117.33 degrees at 6 post-op week. The t value and P value (<0.0001) was found to be very significant.
Graph 1: Post Operative Flexion
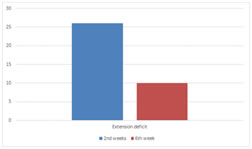
Table 8: Post-operative extension deficit at 2 nd and 6th post op week in study group
The table and bar diagram shows that the mean extension deficit at 2nd post-op week (26 degrees) improved to (10 degrees) at end of 6th post-op week. The t value (3.21) and P value (<0.005) was found to be significant.
Graph 2
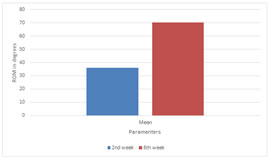
Table 9: Post-operative range of pronation at 2 nd and 6th post op week in study group
The table and bar diagram shows that the mean pronation at end of 2nd post op week was 20 degrees which improved to a mean of 66.17 degrees at end of 6th post op week. The t-value (45.80) and P value (<0.0001) was found to be significant. Graph 3: Post Operative Pronation
Table 10: Post-operative range of supination at 2 nd and 6th post op week in study group
Graph 4: Post Operative Supination The above table and bar diagram shows that the mean supination at end of 2nd post-op week was 36 degrees and it improved to a mean of 70.33 degrees at end of 6th week post-op. The t value of 36.11 and P value (<0.0001) was found to be significant. Table 11: Mepi wise distribution
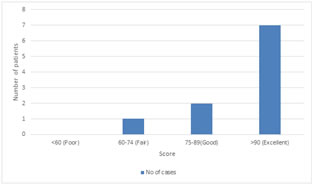
Graph 5: Mayo Elbow Score
In above table and bar diagram shows that in our study group out of 10, 7 cases (70%) had MEPI score (Mayo Elbow Performance Index) >90 which indicates excellent result, 2 cases (20%) had MEPI score 75-89 which is good result and 1 case (10%) had MEPI score 60-74 which indicates fair result. Figure : Supination at time of discharge Figure : Pronation at time of discharge
DISCUSSION The treatment of radial head and neck fractures is still controversial, despite many trials and studies. Plenty of implants have come up in the recent past, but no single implant is universally accepted for the operative management of these fractures. We compared our results with other established studies for radial head and neck fractures treated with press fit modular radial head prosthesis. In our study, the range of age was (30-56 years) with mean age at presentation was 39.8 years, with the most common age at presentation being <40yrs i.e. 6 cases (60%) and >40 years being 4 cases (40%) which corresponds to Hung-Yang Chien et al.20 who retrospectively examined 13 patients with radial head fractures. In his study the mean age at presentation was 38.6 years. In a study done by Vidisha Kulkarni et al.21 the mean age was 40.43 years, maximum age in the study was 55 and minimum age was 26. In our study we had 7 females (70%) and 3 males (30%). Hung-Yang Chien et al.20 in their study out of 13 patients, 9 patients were male and 4 patients were female. According to the study done by Vidisha Kulkarni et al.21 out of 30 patients, 18 cases (60%) were male and 12 cases (40%) were female. Rahul Kadam et al.22 in a study of 18 patients noted 12 were males and 6 were females. In our study, female preponderance was more because in our set up there were females who were involved in outdoor activities like farming or working as a labour. The main mechanism of injury in our study was due to fall i.e 7 cases (70%) and 3 cases (30%) was due to Road Traffic Accident (RTA) which corresponds to Hung-Yang Chien et al.20 in their study, out of 13 patients, in 11 patients the mechanism was by fall and in the other 2 patients, was RTA and Judo. Rahul Kadam et al.22 noted mode of injury in 8 of them was a fall on an outstretched hand, 6 of them had a RTA and 4 had history of assault. Vidisha Kulkarni et al.21 found most common mode of injury as RTA in 18 cases (60%) and fall in 12 cases (40%), In our study, out of 10 cases, 8 cases (80%) had right side elbow injury and 2 cases (20%) had left side elbow injury which corresponds to Hung-Yang Chien et al.20 in their study, 7 out of 13 patients had right side elbow affected and for the remaining 6 patients left side elbow were affected. Vidisha Kulkarni et al.21 reported 16 cases (53.33%) of right sided fracture and 14 (46.67%) of left sided. Modified Mason's classification has been used in our study to classify fracture types of all 10 patients; out of which 8 cases (80%) were type III and 2 cases (20%) were type IV which corresponds to study done by Vidisha Kulkarni et al. who noted 22 cases (73.33%) of type III and 8 cases (26.67%) of type IV. Hung-Yang Chien et al.20 in their study found that all the 13 patients had type Ill fracture types. Out of 10 cases, the Mayo elbow performance index (MEPI) in 7 cases (70%) was excellent results, 2 cases (20%) good results, 1 case (10%) fair results and none had poor result which corresponds to Hung-Yang Chien et al.20 Out of their 13 patients, 8 patients had excellent results, 3 good results, and 2 fair results. According to Vididsha Kulkarni et al.21 , in their study, 20 cases (66.67%) had excellent results, 8 cases (26.66%) had good results, 1 case (3.33%) had fair results, and 1 case (3.33%) had poor result. Rahul kadam et al.22 shows excellent result in 13 (72%) of the patients good results for 3 (17%) and fair result in 2 (11%). Eight cases (80%) out of 10 cases had no complications, 1 case (10%) had infection and 1 case (10%) elbow stiffness. Hung-Yang Chien et al.20 in their study out of 13 patients, 2 patients had elbow stiffness 6 months after Radial Head Replacement. Vidisha Kulkarni et al.21 reported in 30 patients which were operated for radial head arthroplasty out of that 1 patient came with complex regional pain syndrome (3.33%) and 1 patient (3.33%) came with joint stiffness.
CONCLUSION Radial head prosthesis gives excellent functional outcomes in Modified Mason’s type III and IV radial head fractures with lower complication rate and early mobilisation. The key to successful management of radial head for type III and IV is in planning the surgery beforehand. However, our study is limited by a small sample size and relatively short follow up period. A long term follow up with more number of cases is required to assess further effectiveness of radial head prosthesis in radial head and neck fractures.
REFERENCES
Policy for Articles with Open Access
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home