Official Journals By StatPerson Publication
|
Table of Content - Volume 3 Issue 1 - July 2017
Role of Proximal Femoral Locking Plate in treatment of Subtrochanteric Fractures; Case series
R Gokul Nath1*, Sah Ansari2
1SR, 2Senior Assistant Professor, Department of Orthopaedics, Government Tiruvarur Medical College, Dr MGR Medical University, Tamil Nadu, INDIA. Email: gokulmmc@gmail.com
Abstract Objective: The aim of our study is to evaluate the radiological and functional outcome of subtrochanteric fractures treated with PFLCP (Proximal Femoral Locking Plate). The patients evaluated for clinical and radiological outcome. Method: The study is conducted upon 25 patients with subtrochanteric fractures admitted in our hospital. Their fractures fixed with PFLCP. The operating time, blood transfusion needed preoperatively and postoperatively were taken into account. They were followed up for evaluating functional, radiological outcome and complication if any. The functional outcome measured using Harris Hip Score, The radiological outcome by union at the fracture site. Results: Among the 25 patients in the study 22(88%) patients had fracture union without any further intervention, 1(4%) had implant failure requiring implant removal and fixing with PFLP and bone grafting and Two lost follow up due to death. The average Harris Hip score of the study group is 85.217. Two patients had shortening of operated limb but less than 2cm, One had superficial infection which subsided on administering iv antibiotics. Conclusion: Fixation of unstable subtrochanteric fractures with PFLCP gives good rate of union with minimal complications and is an acceptable and feasible alternative to intramedullary devices and better than conventionally used extramedullary devices. Keywords: Subtrochanteric Fractures Plating, Proximal femur locking plate, PFLCP, Harris Hip Score.
INTRODUCTION Subtrochanteric fractures accounts for about 10-30 percentage of hip fractures commonly seen in two group of patients, one being elderly osteoporotic group followed by low energy trauma and the other being young followed by high violence trauma. These fractures are one of the difficult fractures to treat and high rates of morbidity and mortality even though operated. There are lot of debates regarding choice of implants in fixation of subtrochanteric fractures. Many studies support use of intramedullary devices for these fractures. Though intramedullary devices have advantages of load sharing property and biomechanical merits, these are not without demerits. There are difficulty in insertion, long learning curve and peri implant fractures during insertion 31, 32. Traditionally used extramedullary implants like dynamic condylar screw (DCS), dynamic hip screw (DHS) and Angled blade plate have complications like secondary varus collapse, cut-out, implant failure and limb length discrepancy, mostly shortening. Proximal femur locking plate have lesser rate of complications that are common with the above said implants used in treatment of subtrochanteric fractures. It has an anatomical contour, stable fixed angle construct with its three proximal screws that are inserted into the neck of the femur. The three proximal locking screws provide increased pullout strength which is required most in osteoporotic bone 1,2,8.The Locking plate acts as an internal fixator and splints the fracture as it does not require contact with underlying bone. Therefore it allows some amount of elasticity across the fracture site. This elasticity allows callus formation by secondary bone healing, protecting the implant and reducing the implant failure during initial stages of fracture healing. The callus seen here is a sign of flexibility and not be seen as instability or failure as of conventional rigid plating. We report here the result of a series of subtrochanteric fractures treated with proximal femur-locking compression plate (PF-LCP).The objective of this study is to evaluate the outcome of subtrochanteric fractures treated with PF-LCP MATERIALS AND METHODS This prospective study was conducted in Department of Orthopaedics, Govt Tiruvarur Medical college, Tamil Nadu Dr MGR Medical University. Patients with Subtochanteric fracture have been treated by Stabilisation with “Proximal Femur Locking Plate”. The patients were followed up to evaluate radiological outcome for fracture union and the functional outcome is measured with Harris Hip Score. The period of study is November 2014 to December 2016. Patients selection criteria are; age more than 20 yrs, closed or type 1 open subtrochanteric fractures, willingness for informed consent, previously ambulatory patients. Exclusion criteria are pathological fractures, Grade II and III open fractures, local infection, polytrauma and drug or alcohol abuse. Implants Used Proximal Femur Locking Plate(PFLCP), 7.3mm Cannulated Cancellous locking screws, 5mm Cortical locking screws, 4.5mm Cortical screws. The LCP Proximal Femoral Plate. used in our study is a limited-contact stainless steel plate with 316L configuration. These plates are side specific plates. The plate is precontoured in its proximal portion to accommodate the proximal femur. The two proximal screw holes are designed for 7.3 mm cannulated Cancellous locking screws first hole has predetermined angle of 950, the second hole has a predetermined angle of 1200 and the third locking hole is designed for 5.0mm Cortical locking screws and it has a predetermined angle of 1350. The remaining screw holes in the plate shaft are combi-holes that can accommodate both 4.5 mm cortical screws and 5mm cortical locking screws. Surgical Technique Patient after anaesthetic evaluation and getting informed written consent surgery done. After administering spinal anaesthesia patient placed on fracture table with traction. Reduction of fracture done and reduction checked with C-Arm in both AP and Lateral views. Mid lateral skin incision extending proximally from just above tip of trochanter to the level depending upon the size of the implant and fracture extension is made. The fascia lata is split along the incision line. The vastus lateralis is incised along the incision line and lateral surface of proximal femur is exposed. The reduction if not obtained by closed method can be obtained by open manipulation. The reduction thus obtained is temporarily held with K-wire or reduction clamps. The PFLP placed over lateral surface and checked with C-Arm to ensure tip of plate to be flush with tip of trochanter. Using threaded drill sleeve and drill guide, guide wire is inserted into 950and 1200 hole in respective manner, the 1350 hole is drilled with 4mm drill bit using threaded sleeve. The position is checked with C-Arm to ensure guide wire is in the neck and head. The proximal 2 holes drilled with 5mm cannulated drill bit and 7.3mm cannulated screws inserted after measurement. 1350 hole after drilling with 4mm drill bit 5mm cortical locking screw inserted after measurement, if the screw track passes through the fracture line 1350 screw hole can be left(fig 2). Then other combiholes are drilled and screws whether 4.5mm cortical screws or 5mm cortical locking screws. Wound is closed over drain. Follow Up The drain is removed after 2 days. Quadriceps strengthening exercises, Hamstring exercises, knee bending exercise, Passive and active assisted abduction exercises are started after 2 days as per the patient’s pain tolerance. Gait training is given, patient is allowed to walk non-weight bearing with support as per patient’s pain tolerance. Suture removal done on 12th POD and discharged. Patient is advised to come for follow up after 4 weeks, end of 3 months 6 months. Patient advised to walk with touch toe weight bearing at end of 6 weeks after taking x-ray. After 3 months after x-ray if adequate callus is seen patient advised for weight bearing with support as per pain tolerance of patient if not, partial weight bearing with support. Patient is followed till full functionality is achieved. Functional outcome is measured using Harris Hip score (Tab 1). RESULTS Table 1
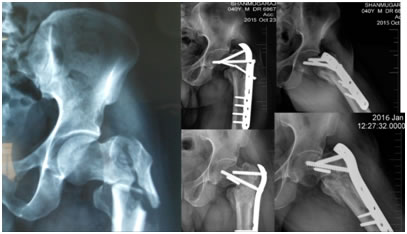
Out of 25 patients, 22 patients (88%) had fracture union without intervention, 2(8%) patients lost follow up due to death. One patient (4%) had implant failure with broken plate as the patient started full weight bearing earlier against the advice, for that patient second sugery was done, implant removed and fracture fixed with PFLP and bone grafting done, the patient had fracture union after 9 months of follow up with Harris Hip score of 87. One patient had superficial infection (4%) which was treated with antibiotic without any complication. 2 patients(8%) had limb length shortening but less than 2cm but had HHS 91 and 82.One patient presented after 6 weeks of trauma after getting native treatment and had severe comminution, hence during surgery 2 cm shortening done to achieve reduction and bone grafting done. The mean Harris Hip Score of the study group is 85.217. Mean age of patients of our study is 56.8 years. Average follow up period is 39.08 weeks. 11 patients (44%) required bone grafting as there is comminution or bone defect. 14 patients (56%) had right sided fracture. Mean operating time was 97.6 minutes. Mean number of C-Arm images used peroperatively. Functional outcome as measured using Harris Hip Score is interpreted as follows. Those with score <70 has poor outcome, 70-79 has fair outcome, 80-89 has good outcome and 90 and more has excellent outcome In our study 9 patients (36%) had excellent outcome, 12 patients (48%) had good outcome, 1 patient (4%) had fair outcome. One patient with implant failure (fig 3) with non union had undergone 2nd procedure and after follow up final HHS is 87. Two patients (8%) expired which is not related to surgery and lost follow up.
Figure 1: Comminuted Subtrochanteric fracture xrays preop, immediate post op and 8 months post op
Figure 2: Subtrochanteric fracture X Rays preop, immediate post op and 9 months post op
Figure 3: Comminuted Subtrochanteric fracture X Rays preop, implant failure and 4 months post op after second procedure
All patients in follow up gained ability to squat and walk after 6 months of surgery (fig 1), except the patient with non union, who gained ability to squat and walk after 6 months of second procedure.
DISCUSSION The important anatomical feature of the proximal femur is the neck-shaft angle that creates a unique biomechanical environment. Koch37 calculated the tension stress on the lateral cortex in the subtrochanteric region and the tremendous compression stress on the medial side The main principles in management in case of Subtrochanteric fracture are following1,2,4,5,6,7 Restoring the Postero-medial cortical stability of proximal femur which bears highest compressive stress, Maintaining anatomical angle – neck shaft angle, Restoration of angular deformities, Minimising injury to soft tissue and osseous fragments to avoid non-union, Stable internal fixation, Bone grafting in case of Postero-medial comminution.. If we follow above principles strictly good rate of fracture union and functional outcome is achieved. The main aim in treating subtrochanteric fractures is restoring the stability and early mobilisation of the patients which reduce the mortality /morbidity rates seen in patients during prolonged immobilisation. This also improves functional recovery by reducing rates of non-union, malunion and also encourages mobility. Subtrochanteric femur fractures require durable and stable implants for maintaining the stability for longer period required for healing. Though intramedullary fixation has good record for the treatment of subtrochanteric femur fractures and is considered currently gold standard treatment, some prefer extramedullary fixation and are using it with good rate of success. As newer implants and techniques are evolving, particularly with advent of locking plates and minimally invasive procedures, extramedullary devices may play a more significant role in the treatment of subtrochanteric femur fractures. A Bio-mechanical study6 conducted by Brett D Christ et al comparing Locking plates and Angled Blade plate on bone models showed PFLCP has high axial load stiffness. This study showed that PFLP with the ‘‘kickstand’’ screw (that was applied at a 1350 in third hole of proximal part) was the stiffest construct (92.2 6 17.4 Nm/m). It was 194% stiffer than the PFLP without applying the kickstand screw, 211% stiffer than the angled blade plate and 309% stiffer than the broad locking plate. The precontoured structure of PF-LCP avoids varus collapse/ malreduction. The anatomical contouring of the implant to the lateral surface the proximal femur with its tip flush with tip of the greater trochanter restores neck shaft angle relationship, thus avoiding mal-union and mal-reduction. In the study 22 out of 23 patients (95.65%) who had complete follow up had good union and functional outcome. 2 patients expired and lost follow up. Failures of the PFLCP have been reported in two case series10,33. Wieser et al 33 reported four cases of secondary varus collapse of the subtrochanteric fracture with implant failure in unstable intertrochanteric and subtrochanteric fractures. In all of these cases lack of posteromedial support and the lack of compression of trochanteric fragments leading to stress concentration at the junction of the proximal locking screws and LCP were considered to be responsible for the hardware failure. Similarly, Glassner et al10 reported seven failures of PFLCP among 10 cases in study. Of the seven cases, two were acute peritrochanteric fractures, one was an early failure of a compression hip screw, one a periprosthetic fracture at the site of a prior hip fusion, and three were non unions. In both of these series, patient and surgical technique-related factors appear to be the cause of failures rather than the weakness of construct. In our study one patient had implant failure as the patient started early weight bearing against advice and not due to the above reasons.
CONCLUSION The subtrochanteric fractures are unique type of fractures due to its biomechanical properties with high tensile stress on its lateral aspect and high compression force along its medial aspect, muscular attachments and osseus structure. Our study shows that PFLCP is an acceptable and feasible alternative in cases with lateral wall comminution where intramedullary devices are difficult to use and it is also superior to other conventionally used extramedullary devices by its biomechanical stability6 as it has high load axial stiffness than others. Good union rate and functional outcome is obtained by achieving following principles good posteromedial stability, maintaining neck shaft angle, minimal soft tissue handling, stable fixation and bone grafting in case of posteromedial comminution. As our study is level IV case series study further studies are needed to evaluate the role of PFLCP in treatment of subtrochanteric fractures.
REFERENCES
|
|
 Home
Home