Official Journals By StatPerson Publication
|
Table of Content - Volume 4 Issue 1 - October 2017
A prospective study of the effect of platelet rich plasma (Autologous) injection in osteoarthritis of knee joint (2015-17)
S Venkat Raman1, P Sugnaneswar M S2*, M E Luther3, G Umakanth4
1Associate Professor, 2Assistant Professor, 3HOD and Professor, Department of Orthopaedics, Kamineni Institute of Medical Sciences, Narketpally, Nalgonda, Telangana, INDIA. Email: drgnaneswar@gmail.com
Abstract Osteoarthritis (OA) of the knee is one of the main causes of musculoskeletal disability. PRP (Platelet Rich Plasma) (Autologous) injection into the knee is a safe method without any major complications. PRP injection is neither a substitute for Total Knee Replacement nor does it prevent further progress of the disease, except relieving the pain, and stiffness of knees. The mechanism and duration of action of PRP is still not completely understood, and requires further detailed study. We can safely conclude that autologous PRP injection into the knee, in early Osteoarthritis (Grade I and Grade II) of Ahlback’s Radiological grading does give relief from pain, stiffness and improves functionality, without any major side effects and can be recommended as a viable modality of treatment. Key Words: Osteoarthritis (OA), Platelet rich plasma (PRP), injection.
Osteoarthritis (OA) of the knee is one of the main causes of musculoskeletal disability1. Osteoarthritis is a common, debilitating disease which is associated with a large societal and economic burden, in addition to the physical and psychological sequelae, it often manifests in the affected individual2. Osteoarthritis is the fourth leading cause of “years lived with disability” (YLD), accounting for 3.0% of total global YLD’s. As per WHO by 2030, the demand for total knee arthroplasties will increase up to 670%3. Pathogenesis: Osteoarthritis (OA) is a degenerative condition involving cartilage, bone, synovium, ligamentous capsular structures, and surrounding muscles. It is characterized structurally by synovial inflammation, degradation of articular cartilage, loss of joint function, active bone remodeling and angular deformity or malalignment. Although a variety of synovial fluid markers provide insight into the biological response of joints to injury, no chemical or anatomic (imaging) biomarkers have been identified that monitor the development and progression of OA or the response to therapy. OA is thought to be highly cytokine-driven, and is associated with mechanical stress resulting from overloading of subchondral bone from dysplasia, malalignment, and trauma. The small protein mediators (cytokines) provide chemical signaling or “cross-talk” among involved tissues. These signaling molecules incite inflammation in the synovium, remodeling subchondral bone, and enzyme activation and extracellular matrix degradation in the articular cartilage.4 The Concept of Intra Articular Cellular Therapy: The studies of intra-articular cellular therapy injection for osteoarthritis and focal cartilage defects in human knee suggests positive results with respect to clinical improvement and safety. Numerous injection therapies have been proposed including hyaluronic acid (HA), platelet-rich plasma (PRP), bone marrow aspirate concentrate, and other stem cell therapies, either autologous or allogenic cells. The cell dose, number of injections, varied from study to study. The use of MRI and arthroscopy for follow-up assessment also varied widely in their results. There are several possible mechanisms of action for transplanted cells including (1) homing of cells to sites of degenerative or missing cartilage, followed by proliferation and differentiation into functional cartilage or cartilage like tissue (2) repopulating of progenitor cell pools on the surface synovium or existing cartilage that may subsequently migrate into regions of cartilage damage or augment the ability of existing cartilage to resist degradation, (3) repopulating of a cell pool that modifies the intra-articular milieu either through cell – cell interaction or through secretion of soluble factors to reduce inflammation and /or activate catabolic agents. To date, the presumed mechanism of action of the cellular therapies has been left largely unaddressed in the clinical literature7. The cell source (Peripheral blood, bone marrow aspirate (BMA), fat), anatomic location (buttocks, retropatellar fat pad) and method of harvesting and processing are essential variables that receive specific characterization to ensure reproducibility and systemic refinement in future work 7. In our study autologous PRP injection has shown promising results. Physiology Of Platelet Rich Plasma: PRP has increased concentrations of PDGF (Platelet Derived Growth Factor), VEGF (Vascular Endothelial Growth Factor), TGF-beta-1 (Transforming Growth Factor}, and EGF (Epidermal Growth Factor) compared with their concentrations in whole blood. PRP in OA knee joints8 delivers natural growth factors and their cytokines containing anabolic and catabolic factors in supraphysiologic concentrations directly into the site of injury to potentially optimize the healing environment. Maintaining a natural ratio of growth factors may provide a homeostatic environment and theoretically provide an abundance of healing factors without disrupting their in vivo relationships.9
MATERIALS AND METHOD It is a prospective longitudinal study on 31 primary osteoarthritic knee joints, selected from the Outpatient Department of Orthopaedics, Kamineni Institute of Medical Sciences, Narketpally, Nalgonda District, Telangana State. Clinical examination and x rays of the knee joints were done, and blood samples of the patients were collected and PRP prepared in the Department of Transfusion Medicine of the same institute. Infiltration was done in the Operation Theatre under strict aseptic conditions. Patients were assessed with WOMAC (Western Ontario McMaster Universitiy Arthritis Index) scoring pre injection of PRP and post injection period of 1 month and 6 months. A reduction in WOMAC score was suggestive of improvement in the patient’s condition. Inclusion Criteria
Exclusion Criteria
Ahlback Radiological Grading of Osteoarthritis of Knee Joints (Image – 1) Grade I: Joint Space narrowing (< 3mm) Grade II: Joint space obliteration Grade III: Minor bone attrition (0-5mm) Grade IV: Moderate bone attrition (5-10mm) Grade V: Severe bone attrition (>10mm) Patient Selection All patients with primary osteoarthritis of knee joints were evaluated clinically using WOMAC scoring and by radiographs. Based on Ahlback’s radiological grading, patients with Grade I and II Osteoarthritis were selected irrespective of age, sex and socioeconomic status. Selected patient‟ s blood samples were sent for complete blood picture, erythrocyte sedimentation rate, C-reactive proteins, random blood sugar and HIV and HbsAg status. Patient blood was evaluated to assess the white blood cell count and platelet count prior to the infiltration. Patients with elevated white blood cells, and platelet counts less than 100000/cubic mm, elevated erythrocyte sedimentation rate and positive C-reactive proteins, random blood sugar levels beyond 80-140 range, HIV and HbsAg reactive patients were excluded from the study. Selected patients WOMAC score was recorded in a separate chart for each patient and follow up scorings were noted down in the same chart of the patient. Consent: Verbal, and written consent was obtained after thorough counseling the patients. Standard Operating Procedure For The Preparation Of Platelet Rich Plasma (Prp): In the Department of Transfusion Medicine, from each patient 50 ml of venous blood was collected from the antecubital vein atraumatically in an effort to avoid irritation and trauma to the platelets with a syringe, blood was transferred to the vacutainers of 4.5 ml containing CPD-A1 (citrate phosphate dextrose and adenine) as an anticoagulant. The tubes were then centrifuged for 15 minutes at 1500 rpm on a table-top centrifuge, and the blood was separated into PRP and residual red blood cells. Hereafter, the procedure was completely performed inside the biosafety cabinet. The PRP was then extracted through a pipette and transferred to a test tube. The final PRP was assessed for platelet count and was supplied for injection in a 10-Ml syringe (approximately 8 Ml per knee). Total leucocyte count and platelet count were measured from the patients peripheral blood as well as in the final PRP. Total leucocyte count was zero in our PRP, The mean platelet count concentration achieved by our method was more than five times the platelet count of blood of that patient. Method of Injection: In the operation theatre with the patient in supine position, the knee was scrubbed, painted and draped with sterile towels. With the patient’s knee in 60 degrees of flexion, under aseptic conditions, 8 ML platelet concentrate was injected into the knee joint with an 18- gauge needle without local anesthetic. 1 ml of CaCl 2 (calcium chloride) was injected in a ratio of 1:4 for every 4 Ml of PRP. After the procedure Robert Jone’s compression bandage was applied and the knee was immobilized for 10 minutes. For any possible side effects like dizziness, or sweating patients were observed for 30 minutes. During the follow-up period, nonsteroidal anti-inflammatory drugs were not allowed, and Tramadol (dosage, 50 mg orally, bds) was prescribed in case of discomfort; all patients were asked to stop medications 48 hours before follow-up assessment. Outcome Measures: Each patient was allotted a separate WOMAC chart till complete follow up. Each knee was scored separately as we were considering each knee as a separate unit. Initial WOMAC score was recorded prior to the administration of PRP infiltration i.e. on day 0 and after the infiltration, patients were asked to come for review after the end of the 1st and 6th month.. A decrease in the WOMAC score was considered as improvement in the patient’s condition. WOMAC score is measured in its individual variables and in total. As we have not found the grading of results of WOMAC score, in the literature, we have graded it to quantify the results. Outcome measured is quantified in percentage of improvement. 85-100% improvement: excellent 70-84% improvement: good 55-69% improvement: fair < 55% improvement: poor The means of the each parameter and total WOMAC score were calculated and ANOVA (Analysis of Variance) done for all the cases. OBSERVATIONS AND RESULTS In this study, 31 osteoarthritic knee joints, out of which 19 patients were of Ahlback’s radiological grade I, and 12 patients with Ahlback’s grade II – (table-1), were selected in the Orthopaedic Outpatient Department. 12 patients were with bilateral early osteoarthritis and 7 patients were unilateral (table-2,) 4 patients selected were males and the remaining 15 patients were females (table-3,).
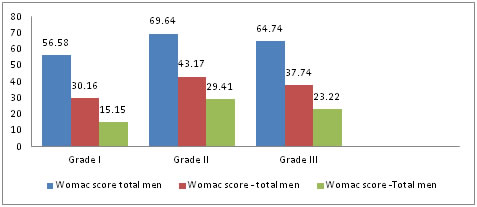
Figure 1:
Effect of PRP on Pain: In this study, the pain scores of the patients have decreased on the day of injection to one month and six months. Their mean scores have decreased from the day of infiltration to one month and six months. It means that there is definite decrease in the pain after infiltration, but on seeing the individual pain scores, for one case, pain has subsided completely. Over all, the pain intensity has decreased in severity. Since p-value is less than significance level (p<0.05), Null hypothesis cannot be accepted. Hence it can be concluded that the efficacy of the PRP treatment from zero day to sixth month is statistically significant. Similar results are seen from the results from one month to six months follow up. Effect of PRP on stiffness: In this study, the stiffness scores of the patients have decreased on the day of infiltration to one month and six months. Their mean scores have decreased from the day of infiltration to one month and six months. It means that there is definite decrease in the stiffness after infiltration, in one case there was no stiffness prior to the infiltration, and there was no stiffness in 10 knee joints at six months follow up, i.e. stiffness had completely subsided. Over all, the stiffness intensity had decreased in severity. Since p-value is less than significant level (p<0.05), Null and hypothesis cannot be accepted. Hence it can be concluded that the efficacy of the PRP treatment from zero day to sixth month is statistically significant and improved. Similar results are seen from one month to six months follow up. Effect of PRP on functionality: In the present study patients the functionality scores of the patients have decreased from the day of injection, to one month and six months. Their mean scores have decreased from the day of infiltration to one month and six months. It means that there is definite improvement in the functionality after injection, but on seeing the mean functionality scores, in no joint the functionality scores have completely subsided. Over all the functionality restriction decreased in severity. Since p-value is less than significance level (p<0.05), Null hypothesis cannot be accepted. Hence it can be concluded that the efficacy of the PRP treatment from zero day to sixth month is statistically significant and improved. Similar results are seen from one month to six months. Effect of PRP on total Womac score: In the present study the total WOMAC scores of the patients have decreased from the day of injection to one month and six months (table-4, chart-1). Their mean scores have decreased from the day of injection to one month and six months. It means that there is definite decrease in the total WOMAC score after injection, but on seeing the mean total WOMAC scores, in no joint the scores have reduced to zero. Over all, there was decrease in severity of pain and stiffness. Since p-value is less than significance level (p<0.05), Null hypothesis cannot be accepted. Hence it can be concluded that the efficacy of the PRP treatment from zero day to sixth month is statistically significant and shows improvement. Similar results are from one month to six months follow up. (table-5, chart-2) RESULTS
Table 4: Comparision of means of WOMAC score – Total on ‘0’ day, 1st month, 6th month of grade I and Grade II Osteoarthritis of knee joints (n=31) based of ANOVA
Figure 2: WOMAC score – total score Assessment
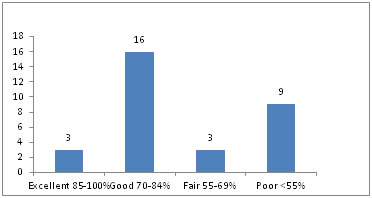
Table 5: Analysis of results of all knee joints according to the working classification (n=31)
Figure 3: Analysis of results of all knee joints according to the working classification (n=31)
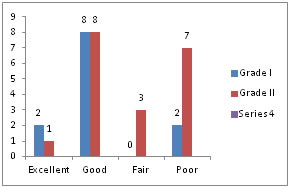
Table 6: Comparison of results of grade I and grade II knee joints according to the working classification (n=31)
Figure 3: Comparison of results of grade I and grade II knee joints according to the working classification (n=31)
DISCUSSION Articular cartilage lesions and degeneration are difficult to treat and present a challenge for orthopaedic surgeons because of the distinctive structure and function of hyaline cartilage and its inherent low healing potential. For therapeutic intervention, laboratory investigations are focusing on the possibility of preserving normal homeostasis or blocking or at least delaying the need for more invasive surgical procedures. Current pharmacologic interventions may only temporarily reduce chronic pain, but for the time being, no proven disease modifying therapy is available10. In this prospective study, WOMAC scores were evaluated pre-injection and post-injection period on first month and sixth months. There is a correlation in Grade I and Grade II mean WOMAC scores. In Grade I, the mean WOMAC score of pain, stiffness and functionality is lower than the Grade II osteoarthritis knee joints. There was no control group in this study. The number of platelets used are more than 5 times the base line, as all the patients are selected were having more than one lakh platelets, so every patient got more than 5 lakh platelets per ml, which is prepared by single spinning of the sample for 15 minutes with 1500 RPM( Rotations per minute) and leucofilters were not used. Kon et al in 2011, used double spinning with more than 5 times the base line platelets activated with CaCl2 and gave more than three doses of injection with 2 weeks interval9. Patel et al in 2013, used single spinning technique with leuco-filters. They have given two injections of PRP activated with CaCl2, each 8 ml, with 3 weeks gap. Their platelet count is less than 5 times the base line1, 11. In 2011, Filardo et al, used 5 ml PRP with 5 times the platelet count prepared from double spinning technique and activated with CaCl2. They have infiltrated three injections of PRP with one week gap. In 2012 they compared the single versus double spinning and found no significant difference in the results. All the patients who have received the PRP have shown decrease in the pain, stiffness and functionality 47. Cerza et al in 2012 used 5ml of PRP not activated with CaCl2, platelet count less than the 5 times the baseline with single spinning and without leuco-filters. They have infiltrated four injection with each one week gap. The idea of using CaCl2 was, it activates the platelets12. Spakova et al in 2012 did similar study, PRP prepared after spinning it for three times and without using leuco-filters and they have used three injections with one week gap. They have stated that the leucocyte content did not seem to induce negative effects or to impair the potentially beneficial effects of PRP, even when used in joints. However, they cannot conclusively claim that increased white blood cells in PRP have positive effect on knee joint13. The preparation of PRP, number of platelets, amount of PRP infiltrated, and frequency of injections were not uniform. Different researchers have used different methods of preparation, different amount of PRP and at different time periods. Thus we can conclude that the method of preparation of PRP; the platelet count to be achieved before infiltration; the usage of leucofilters; the number of injections for each knee joints; the duration between injections; all are varying and nothing is standardized at present. In this study all the patients have shown decrease in the WOMAC score. Their mean pain, stiffness and functionality scores have decreased. The decrease in WOMAC score continued upto six months. The improvement in our patients could be explained by the fact that injected platelets might have acted at different levels and were not stimulating the chondral anabolism or slowing the catabolic process. As we have given a working classification to assess the results, 3 joints have shown excellent results, 16 joints have shown good results, 3 joints have shown fair results and 9 joints have shown poor results. Though the mean pain scores have deceased in all the patients, the efficacy had been varied from the patient to patient. Results were poor in obese, female patients with active labor work. Five patients who have used NSAIDS (Nonsteroidal anti-inflammatory drugs) against the medical advice have shown poor results. But it is not clear that how the obesity with active labor work and NSAIDS have their isolated effect on knee joints. The results show better improvement in grade I osteoarthritis knee joints than grade II knee joints. Grade I patients shown 73.01 percentage of improvement, whereas grade II patients shown 56.82 percentage when evaluated with WOMAC score. But the difference is not statistically significant. In every patient there is decrease in WOMAC score, but in no one it has reached „0‟. It means that PRP delays the osteoarthritic progression in the joints, but it has not cured osteoarthritis. To evaluate its duration of action long term follow up studies are required. Filardo et al. in 2012, have also shown similar results, better results are seen in early osteoarthritis knee joints than advanced arthritic knee joints in their comparative study done between PRP and Hyaluronic Acid treatment of osteoarthritis of knee joints13, though they have not found significant improvement in PRP group when compared with hyaluronic acid. in their previous study in 2011, the final evaluation confirmed that female patients showed the poor results, which probably due to gender specific biological and biomechanical characteristics, which might influence the etiopathogenesis, the effects of the growth factors and ultimately, the clinical response to treatment. In this study no gender specificity was calculated. Spakova et al. in 2012, in their study found statistically significant improvement in WOMAC score, VAS and pain relief when compared to viscoelastic supplementation14. Kon et al. in their study in 2011 had shown significant improvement in all parameters of the WOMAC score in the group of patients who were infiltrated with PRP upto 6 months follow up. But the condition of the patients were decreased from 6 months to 12 months follow up, i.e the effect of PRP decreasing from 6 months onwards.Some influencing factors were detected, in particular it was observed that young male patients were the best responding group, especially in case of simple chondropathy without signs of oateoarthritis12. In a later study evaluating the same patients at 24 months of follow up confirmed this trend with a further decrease in the clinical outcome, thus concluding that intra articular therapy with PRP is time dependent with an average duration of 9 months and better and longer results are achieved in younger patients with lower levels of joint degeneration. They have also stated that PRP has no beneficial effect in advanced Osteoarthritis. Older and more degenerated joints present a low percentage of living and vital cells, therefore a low response potential to the growth factors. Extensive structural joint damage in severe osteoarthritis is hardly reversible. The biologic changes induced by PRP may only weakly influence older joints with higher degenration15. In this study the results have shown that the effect of PRP sustained for 6 months with continuous decrease in all parameters, i.e. pain, stiffness and functionality of the WOMAC score. As this study was done for only six months, this study cannot explain the duration of action of PRP in treating Osteoarthritis of knee joints. Filardo et al. in 2012 found that there was worsening of the condition of the patients by the end of 9 months, it means that the duration of action of PRP was 9 month, but still needs further studies to conclude the duration of action of PRP13. Immediate post injection all patients have complained of severe pain but no systemic and long term complications noted during the course of study. Sandeep Patel et al, in 2013, in their study have documented some systemic adverse effects. Which were immediate and systemic rather than local and were of short duration not lasting more than 30 minutes. But they have not explained the characteristics of the adverse effects. They have attributed these adverse effects to the higher number of platelets in the infiltrating PRP sample and the possibility of CaCl2, which was used as an activating agent1. Kon et al. in 2010 and Sanchez et al. in 2007 have reported some injection pain, local inflammation of short duration and reaccumulation of effusion, but the exact numbers were not mentioned12. All the patients have shown improvement at around fifteen days. Therapeutic benefit might not be because of chondrogenesis, because it would have taken more time for the patients to perceive this benefit. Filardo et al in 2012 have shown worsening of WOMAC score from nine months onwards13, it implies that if the chondral remodeling was the cause for the improvement of symptoms, the benefit would have started later and lasted for a longer duration. Sandeep patel et al. in 2013, through their study stated that the improvement in patients of osteoarthritis of knee joints is not because of the stimulation of the chondral anabolism or slowing the catabolic process1. PRP may influence the overall joint homeostasis, reducing synovial membrane hyperplasia and modulating the cytokine level, thus leading to an improvement in the clinical outcome, even if only temporarily and without affecting the cartilage tissue structure and joint degeneration progression. This study has its limitations,
Further studies are required to better understand the mechanism of action of PRP, the dosage of PRP, duration of action, frequency of injections, its composition and role of CaCl2 in its activation. It is necessary to understand the results of PRP, whether they are temporary or permanent. Different platelet concentrations and application modalities have to be studied further.
CONCLUSION
REFERENCES
|
|
 Home
Home