Official Journals By StatPerson Publication
|
Table of Content - Volume 4 Issue 2 - November 2017
A prospective clinical trial to study the efficacy of biological membrane in the management of diabetic foot ulcers
Sambandhamurthy Venkat Raman1, Pendyala Sugnareshwar2*
1,2Associate Professor, Department of Orthopaedics, Kamineni Institute of Medical Sciences, Sreepuram, Nalgonda, Telangana, INDIA. Email: drvraman@gmail.com
Abstract Objectives: To study the role of Biological Membrane in the management of diabetic foot ulcers. Methods: Biological membrane alone was used as a definitive wound cover in 23 cases. In the remaining 77 cases definite cover like skin graft/ flap was done after preparing the wound with biological membrane. Results: All the wounds healed completely without complication with Biological membrane alone or with definite procedure like skin graft or flap cover. Conclusion: Biological membrane can be used either as a primary skin cover, or to prepare the wound for subsequent skin graft or flap cover. Key Words: Diabetic foot ulcer, Biological membrane.
Certain categories of wounds, in particular, such as those caused by diabetes pose formidable problems. One of the most common complications of diabetic foot ulcer is secondary infection and considerable fluid loss from the exposed areas1. A large diabetic foot ulcer denuded of its epithelial covering wound heal by scarring or by the in growth of the epithelium from its margins. In small diabetic foot ulcer epithelial growth would occur, though at a small pace and some of the epithelial covering process may be hampered by exogenous infection of the raw area. The provision of some cover over the diabetic raw area, it could be arranged may facilitate the growth of the epithelial cells over the raw area2. Every surgeon attempts for the early closure of the diabetic raw area through various techniques available with him. But there are many occasions when the surgeon is unable to close the wound, due to the severity of the wound, the general health condition of the patient and various other associated factors. It is for these purposes that denuded areas need a temporary cover (Generally classified as skin substitutes) till such times that the body is able to manufacture a cover of its own or till such times as the surgeon is able to cover it either by a skin graft or a flap. Biological membrane are natural, easily available, and ready to use nonimmunogenic, non-pyrogenic and hypoallergenic. In general, biological dressings are the logical best candidate for the management of wounds since they create the most physiologic interface between the wound surface and the environment. This allows the body’s reparative and immune system to function most efficiently. Homograft, Amniotic membranes and collagen category. Among these, collagen established as an effective cover for wounds3. The present article includes our experience of biological membrane (Photo No. 1) in management of diabetic foot ulcer.
Figure 1: Biological membrane after opening pack
MATERIAL AND METHODS In this present study, a total number of 100 patients with diabetic foot ulcers where included and managed during the period of September 2003 to September 2005. This study was done in the Department of Orthopaedic surgery at Mediciti Institute of Medical Sciences, Ghanpur, Medchal, Ranga Reddy (Dist) A.P. India. Diabetic foot ulcers in both type I, and Type II diabetes mellitus were included in our study. All patients were carefully examined clinically. Basic investigation (Hemoglobin, total count, differential count, bleeding time, clotting time, erythrocyte sedimentation rate, HIV, HBs Ag, complete urine examination blood glucose, blood urea, serum creatinine etc) were done for all patients to rule out underlying systemic ilinesses and for fitness for anesthesia. For all cases wound swab was sent from the ulcer for culture sensitivity mainly to know the type of organism and its sensitivity to antiboitcs. Blood glucose was controlled with insulin and / or oral hypoglycemic drugs. Endocrinologist’s opinion was taken for all cases for medical management of diabetes mellitus. After thorough debridement of ulcer, Biological membrane was applied at two to four day intervals till ulcer healed or became fit for definitive cover. Biological membrane is commercially available in 5x5 cm, 10x10 cm, 10x25 cm, and 15x30 cm sizes.(Photo No. 1). The right dimension of Biological membrane was selected for application after removing from sterile pack. After washing sterile saline solution, Biological membrane was firmly applied on to the ulcers and air bubbles beneath were eliminated. This was covered with non adherent paraffin gauze piece. Ulcers were inspected in once in 3 to 5 days depending on the condition. Status of bacterial growth, time taken for wound to become sterile, time taken for the appearance of the granulations, time taken for healing, and complications were noted. Those patient who were unfit for surgery / anesthesia or not willing for surgery were treated by repeated applications of biological membrane alone at two to four day interval. Remaining wounds managed by definite procedures like skin grafting of flap cover. After complete healing these patients were followed up weekly for 1 month and then fortnightly for three months. RESULTS Table 1: Distribution of cases with respect to age and sex
Table 2: Distribution of cases with respect to type of Diabetes
Table 3: Distribution of cases with respect to size of wound
Table 4: Distribution of cases with respect to site of wound
Table 5: Distribution of cases with respect to infection
Table 6: Distribution of cases with respect to side
Table 7: Distribution of cases respect to procedure
COMPLICATIONS In our study, no observable complications were noted. None of the patients developed hypersensitivity reactions to biological membrane.
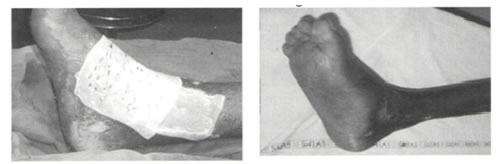
Figure 2: Diabetic ulcer great toe
Figure 3: Figure 4: Figure 5:
Figure 6: Figure 7: Figure 8:
Figure 9: Figure 10: Figure 3: covered with biological membrane; Figure 4: Uclear healed in 2 weeks with biological membrane alone; Figure 5: Diabetic ulcer foot; Figure 6: With biological membrane; Figure 7: Uclear healed in 3 weeks with biological membrane alone; Figure 8: Diabetic ulcer foot Figure 9: Ulcer prepared with biological membrane; Figure 10: After Screen grafting
DISCUSSION Diabetic foot ulcer are becoming a problem in management in day to day surgical practice. The 21st Century is witnessing a drastic change in the life styles of urban dwellers, centering on sedentary life styles, drastic change of diet etc. and diabetes and its attendant complications like non healing foot ulcers are becoming very common4. The patient may be unfit for any definitive procedure (skin graft, flap cover) because of infection, unhealthy granulations, poor vascularity and Biological membrane as a skin substitute / temporary cover appears to be the best alternative. Biological membrane is a natural, sterile, ready to use, non- pyrogenic, economical, easily available, easy to apply, with no local or systemic antigenic properties, no complications, available in a variety of sizes, to suit any wound size. They form the best interface between wound and environment, thus allowing the body’s natural, immune and reparative system to work efficiently.5,6 Chemically the bovine skin dermis collagen used as biological membrane is very similar to the human dermis, and also there is no risk of Hepatitis-B or HIV. There is also a long shelf life under normal storage conditions. Biological membrane is commercially available as a wet sheet form. It is mostly composed of type I Type 3 Collagen. Biological membrane is currently commercially available in International quality FFS Aluminium pouch packing containing sterile preserving liquid medium (a mixture of isopropyl alcohol and water) sterilized by Gamma irradiation. Biological membrane in wet form is most preferred, established and of proven efficacy, because of its excellent tear and tensile strengths and handling properties.6 Histopathological studies of the subcutaneously implanted collagen sheet under the skin of mice have revealed that this tissue does not raise any allergic phenomenon. There is no evidence of foreign body rejection. Like cat –gut, which is also made of collagen, the sheet is retained in the tissues and gradually absorbed by inflammatory cellular activity and the fibrous tissues replaced by fibroblasts. The granulation tissue developed at a normal rate and the cellular events were precisely similar to those occurring in normal wounds. In our study, age groups ranged from 20yrs to 70 yrs and males were more commonly effected (table 1). Type II Diabetes was predominant (table 2). Maximum number of wounds were > 10cm and planter side of the feet were predominating (Table 3 and4). Maximum number of cases had Pseudomonas sp. infections with right foot predominantly effected (Table 5and 6). Those patients who were unfit for surgery / anesthesia or not willing for surgery were treated by repeated applications of Biological membrane alone (Table No 7, Photo No.2-7). Remaining wounds were prepared with biological membrane and later managed by definitive procedure like skin grafting or flap cover (Table No 7, Photo No. 8-10). In our study no noticeable complications were seen. In our experience biological membrane has proved ideal in preventing contamination and thus infection, encouraging granulation reducing the bacterial load of the wounds, and of use as a temporary cover (skin substitutes ) till wound is fit for definitive cover (skin graft/ flap). In those patients who are unfit for surgery / anesthesia or not willing for surgery biological membrane can serve as a definitive cover with repeated applications.
CONCLUSION Biological membrane is a safe, economical effective, non allergic easily available skin substitute with good handling properties, for the treatment of diabetic foot ulcers. It can be used either as a primary skin cover, or to prepare the wound for subsequent skin graft or flap cover. Biological membrane has all the properties of an ideal skin substitute like good adherence, water vapour transport, elasticity, intact bacterial barrier, non-antigenic, non-toxic, anteseptic, haemostatic, easy to apply and remove, with adequate tear strength and economical.
REFERENCES
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home