Official Journals By StatPerson Publication
|
Table of Content - Volume 4 Issue 2 - November 2017
Post polio limb fracture management in a 65 years old patient
M Shoaib Qureshi*, Mangesh Panat, Pratik Israni
Department of Orthopedics, MGM Hospital and Research Centre, Aurangabad, Maharashtra, INDIA. Email: dr.m.shoaibqureshi@gmail.com
Abstract Background: Polio is a virus which affects anterior horn cells, resulting in isolated muscle weakness and paralysis. It has been estimated that approximately 80% of those with polio will experience new symptoms 30-40 years after the initial onset. This may occur as a result of overuse or premature aging of the enlarged motor units, combined with loss of motor units due to normal aging. Halstead defined PPS as the presence of two or more of the following symptoms: unaccustomed fatigue, muscle and/or joint pain, new weakness, functional loss, intolerance to cold, or new atrophy. The associated muscle weakness, primarily in plantar flexion and quadriceps muscles, affects dynamic stability in standing and ambulation. When combined with fatigue, this weakness may contribute to the occurrence of falls. Case Report: A 65 year old, post polio survivor with residual myopathy in right lower limb following trivial trauma suffered supracondylar femur fracture with intraarticular extension, as evident on plain radiograph with osteopenia, flexible elastic nails were considered instead of rigid fixation methods. Following six months, a trivial trauma resulted in a proximal tibia fracture which was managed again with flexible nails. 1 year follow-up good union with rehabilitation was achieved. Conclusion: Our experience showed that FIN is a low invasive and sufficiently stable osteosynthesis in such fractures. Left in place, nails will reinforce mechanical stability. Key Words: Supracondylar Femur Fracture, Post Polio Syndrome, Proximal Tibia Fracture, Osteopenia, Polio Virus.
Polio is a virus which affects anterior horn cells, resulting in isolated muscle weakness and paralysis. It has been estimated that approximately 80% of those with polio will experience new symptoms 30-40 years after the initial onset. This may occur as a result of overuse or premature aging of the enlarged motor units, combined with loss of motor units due to normal aging1. Halstead defined PPS as the presence of two or more of the following symptoms: unaccustomed fatigue, muscle and/or joint pain, new weakness, functional loss, intolerance to cold, or new atrophy2. The associated muscle weakness, primarily in plantar flexion and quadriceps muscles, affects dynamic stability in standing and ambulation3. When combined with fatigue, this weakness may contribute to the occurrence of falls4. Patients often have extensive muscle weakness that exists either as a remnant of the primary infection or appears and progresses later in life as a part of post-polio syndrome (PPS). In addition, other late symptoms such as muscle and joint pain, and fatigue, may contribute to the occurrence of falls5. Femoral fractures in post polio survivors are difficult to manage as the bone is often found to be weak, osteopenic hypovascular with decrease in bulk of surrounding soft tissues and these patients present with a history of low velocity trauma. Consent: The patient has given informed written consent for the case report to be published.
CASE REPORT We present a case report of a 65 year old male non (diabetic, hypertensive, smoker) who is a post polio survivor with residual myopathy in right lower limb. Patient gives history of not being able to bear weight over the right lower limb since childhood and range of motion at knee was restricted from 30 degrees to 90 degrees, he accidently slipped over the wet floor and fractured his right distal femur. On examination the knee was swollen with effusion and patellar tap was positive with crepitations felt over distal femur and tenderness, right lower limb showed severe atrophy of muscles of thigh and leg, there was a limb length discrepancy of 6 cms and no neurovascular compromise radiographs the bones around the knee joint (femur, patella and tibia) were hypoplastic and osteoporotic consistent with the typical appearance of post polio paralytic bones. It also revealed a supracondylar communited femur fracture with intercondylar non communited extension (33.C2). (Fig. 1) MANAGEMENT Patient was taken up for surgery next day, Under spinal anaesthesia with all aseptic precautions, in supine position with bolsters under knee, Under fluoroscopic guidance inter condylar fragment reduced percutanously and one 6.5 mm cc screw was drilled to hold the condyles. Two entry portals were created distal to the fracture site in the cancellous bone for insertion of 3mm pre bent TENS nail medially and laterally. Post operatively patient’s limb was protected with high above knee slab with 30 degrees flexion. DVT prophylaxis was given for 5 days during post op hospital stay. (Fig 2). Follow up x-rays at 6 weeks post op showed callus formation and above knee slab was removed on examination fracture site pain was significantly reduced and fracture appeared “gummy”. Patient was kept nil weight bearing till 3 months (12weeks) when early consolidation was seen, knee rom physiotherapy was started. Patient visited opd on monthly basis till 6 months. (Fig. 3 and 4) at 6 weeks follow up. 6 months later he fell again over his right leg as he slipped from his bed and presented to the emergency department with the complains of pain, swelling over right knee and leg. On examination it was observed patient had severe tenderness over the proximal tibia. Radiograph revealed proximal tibia fracture (41.A3), with no neuro vascular compromise. Temporary immobilization with above knee slab was done. (Fig. 5) Under spinal anesthesia, in supine position under fluoroscopic guidance 2 cm incision taken over the proximal tibia medially and laterally, entry made with awl and two 2.5 mm pre bent TENS nails inserted to cross the fracture site in antegrade fashion. Reduction confirmed under c-arm and was found satisfactory. Above knee slab was given with thromboprophylaxis.fig6 Patients were discharged within 2 days postoperatively. Range of motion and strengthening exercises followed, stitches were removed after 2 weeks. Follow-up was scheduled once per month for the first 6 months and then bimonthly for the rest of follow-up period (range 12–24 months, mean 18.4). Applying braces and gradual progression to prefracture weight bearing was dependent upon the progress of radiological union. (Fig. 7) Now at 1 yr follow up pt has union at distal femur and proximal tibia regions with rom of 20 degrees to 100 degrees. (Fig. 8 and 9) (Fig. 10, 11, 12) depict functional outcome at 1 year follow up. (Fig. 13) Post tibia impant removal. Treatment Plan: Treatment of this fracture created many dilemmas, all options like plaster, skeletal traction, proximal tibial lcp, distal femoral lcp and flexible nailing were explored. In view of the bone being very porotic, hypoplastic the distal fragment being too small we decided to go ahead with flexible nailing.
Figure 1: Figure 2: Figure 3: Figure 4: Figure 5: Figure 6:
Figure 8: Figure 9:
Figure 10:
Figure 13: Figure 1: Pre op distal femur fracture; Figure 2: Post op distal femur fracture; Figure 3 and 4: 6 weeks follow up x-ray for distal femur fracture; Figure 5 and 6: pre op xray proximal tibia fracture; Figure 7: postop xray proximal tibia fracture; Figure 8: 6 weeks follow up for proximal tibia fracture; Figure 9 and 10: 1 year follow x-ray for distal femur fracture and proximal tibia fracture; Figure 11, 12 and 13: 1 year follow up clinical photograph showing function DISCUSSION One study found that 96% of an outpatient population had osteopaenia or osteoporosis and reported a fracture incidence of 38% over 5 years (6). Another study reported that 61% of 233 community-based participants had required medical attention at some point as a result of a past fall and 35% had sustained a fracture7. Femoral bone in these patients will be smaller, deformed and osteoporotic bone, with partially paralyzed and less vascularized muscle envelope8. Conservative treatment of these fractures in the form of traction and casting will worsen the joint contracture associated with complications of bed sores and nonunion9. These patients do present considerable anesthetic risks because of the severe impairment of pulmonary and heart function. Therefore, indication for surgery should be considered carefully. Operative treatment does have advantages over nonoperative treatment at least in selected cases. Hsu et al.10 reported that, in a group of nonambulating patients with distal femoral fractures, they accepted a minimal amount of posterior displacement, which led to an increased knee flexion contracture, increased knee- and hip flexion contracture often makes transfers and also positioning more difficult or leads to an inability to stationary standing in those who do. Physiotherapists often work intensely to prevent the deterioration of knee flexion contracture. We think that, patients with pre existing knee flexion contracture and develops a fracture should also be considered for fracture management and contracture releases in same setting. Non – operative treatment in form of closed reduction is also possible but fracture will be less stable and will be difficult when mobilized. Flexible nails are just sufficient to provide stability to the fracture with minimally invasiveness and protect biology at fracture site. Locked plates at this level have proven advantages but in such a fragile bone chances of fracture above or below the plate are quite high.
CONCLUSION Our report shows that FIN is a feasible, reliable, and low invasive method in these metaphyseal osteoporotic fractures. We think that operative treatment with FIN should be discussed in those patients who need general anesthesia for fracture reduction and should certainly be considered in those patients where mobilization in the wheelchair is difficult or impossible with splints or casts if general anesthesia is arguable.
Clinical Message: In view of the this fractures, biology of the bone and soft tissue around, which was quite unpredictable, flexible stable fixation than rigid fixation options can prove to be helpful to the surgeon and his patients.
REFERENCES
|
|
 Home
Home

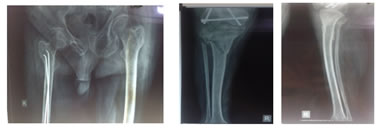

 Figure 7:
Figure 7: 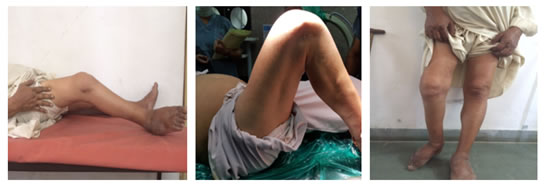 Figure 11: Figure 12:
Figure 11: Figure 12: