Official Journals By StatPerson Publication
|
Table of Content - Volume 5 Issue 1 - January 2018
A study of functional outcome of distal tibial fractures treated with distal metaphyseal locking plates
Pendyala Sugnaneswar1, Anil Kumar Chitumalla2*, M E Luther3, P Vamshi Krishna4
1Associate Professor, 2Assistant Professor, 3Professor and HOD, 4Internee, Department of orthopaedics, Kamineni Institute of Medical Sciences, Sreepuram, Narketpally Mandal, Nalgonda-508254, Telangana, INDIA. Email: drgnaneswar@gmail.com
Abstract For the past decade, plating using fracture reduction has been successful in treating complex fractures of the lower extremity, especially distal tibia. The goal of this technique is to apply stable plate fixation while maintaining the fracture biology and minimizing soft tissue problems. Recently, there has been an increasing trend toward use of a locking plate for treatment of complex fractures of the distal part of the tibia. Compared with a conventional plate, a locking plate imparts a higher degree of stability and provides better protection against primary and secondary losses of reduction and minimization of bone contact. This prospective study on 24 cases of fractures of distal tibia using metaphyseal locking plates, either by open or closed method (MIPPO) yields excellent results as evaluated by Olearud and Mollander scoring system. Key Words: LCP, MIPPO, Locking Plates, Distal Metahysis.
Distal tibial fractures comprise 1-10% of all lower extremity fractures. The treatment of such fractures poses a great challenge to the orthopaedic surgeon1. The challenges are in the form of poor status of the soft tissue envelope, compound fractures and intra articular fractures. In the first half of the last century these fractures were deemed to be non amenable for surgical reconstruction2. Conservative treatment by cast application led to prolonged immobilization of ankle and knee. Stiffness and arthritic changes of ankle affects the quality of life3. However, with better understanding of the anatomy and a better classification of such injuries, surgical treatment has been offered initially with caution and is now practiced on a regular basis4. The many modalities of surgical treatment include intramedullary nailing, plate fixation and external fixation for compound fractures5. Distal metaphyseal plating is one of the accepted modalities of treatment in the last few years6. Certain principles of treatment are followed.
Classification of fractures: Although there are a number of classifications of distal tibial fractures, we have used AO/OTA classification of the distal tibia, which is logical and provides a guide for treatment and probably prognosis. Studies have indicated that good reliability is only achieved at the type A, type B, and type C levels, and that at the nine group and certainly the 27 subgroup level, the classification is not reliable10. The soft tissue injuries are classified as per the Gustilo and Anderson classification and Grade 2 and Grade 3 compound fractures are excluded in this study. Initial Evaluation and Management: A careful history of the mode of injury and mechanism of injury, the likelihood of associated injuries, and the presence of underlying medical conditions that can affect treatment or healing were ascertained. The mechanism of injury provided insight into the amount of energy imparted to the bone and soft tissue at the time of fracture, which was crucial for surgical planning and for advising the patient on prognosis12. Details such as the height of fall or the speed of a motor vehicle accident were therefore important. In open fractures, assessing the environment in which the injury occurred would guide antibiotic treatment. The patients were carefully examined for associated injuries. Once life threatening injuries had been ruled out or adequately addressed, attention was focused on the ankle injury. Deformity of the leg, ankle and foot was often apparent on initial inspection. The neurological and vascular status of the foot was evaluated. When pulses were absent, the leg and ankle were realigned, and then the vascularity reassessed. Splinting the leg and ankle prevents further soft tissue trauma13. Open wounds were inspected to determine their extent and the amount of contamination. The condition of the skin was carefully examined, including the amount of swelling and the presence of fracture blisters14. Tense soft tissue swelling was frequently present, and it was assessed by both inspection and palpation. The presence or absence of skin wrinkles has been recommended as one way to assess the degree of soft tissue swelling. The true extent of the soft tissue injury may not declare itself initially, so the leg and ankle must be frequently reassessed15. Local examination of the injured extremity was observed for swelling, deformity and loss of function. Palpation revealed tenderness, crepitus and abnormal mobility at the fracture site. Distal neurovascular status was assessed by the posterior tibial artery and dorsalispedis artery pulsations, capillary filling, local temperature, pallor and paraesthesia. Antero-posterior and lateral radiographs of the affected leg along with ankle were taken and the fracture patterns were classified based on the AO/OTA classification of fractures of distal tibia. CT scan was done in case of comminuted intra articular fractures. Arterial colour Doppler was done to rule out any vascular injury wherever necessary. The limb was then immobilized in an above knee Plaster of Paris slab till swelling subsided and definitive fixation with locking compression plate done. Patients with open fractures were graded using the Gustilo Anderson classification. Grade 1 compound fractures were treated by cleaning of the wound with copious amount of normal saline and antibiotics were started. This is followed by primary wound closure. The limb was then immobilized in an above knee plaster of paris slab till definite fixation of fracture. Radiological investigations: Standard radiographs in Antero posterior, lateral view of the leg and ankle and mortise views of the ankle were taken when indicated. Repeat radiographs with the limb provisionally reduced provided more information about the fracture pattern is necessary16. Proximal extension of the fracture or suspicion of more proximal injury mandates full-length tibia and fibula radiographs. Some surgeons find views of the contra lateral ankle helpful as a template for preoperative planning. CT scanning was the optimal adjunct to plain radiographs for further imaging of articular fractures of the lower extremity17. It provides more information than plain films and frequently alters the surgical plan. Two-dimensional axial CT scanning helped to define the severity of the injury and aids with surgical planning18. Pre-operative Planning: All the patients were taken for surgery after pre anesthetic checkup and routine hematological investigations. Appropriate informed and written consent was taken. A dose of tetanus toxoid and antibiotic (inj ceftriaxone 1gram intravenously 30 min before surgery) was given pre-operatively. Preparation of the part was done a day before the surgery. Instruments and implants were checked and sterilized beforehand. MATERIAL AND METHODS This is a prospective study from October 2013 to September 2017. Patients with fractures of lower third tibia were admitted to the Department of Orthopaedics, KIMS, Narketpally were taken for this study after obtaining their informed, valid written consent. Inclusion Criteria
Exclusion Criteria
Surgical technique
Postoperative care: Intravenous antibiotic regimen was continued for 5-7 days after the surgery. Another 5 days of oral antibiotics were advised for open reduction and internal fixation. For MIPPO technique, 2 days of intravenous antibiotics were used and then converted to oral antibiotics for another 5 days. Rest of the postoperative care was same for both groups. Suture removal was done at 10th-12th post operative day. The drain was removed 2 days after the operation. Active ankle and knee joint motion was allowed as soon as patient could tolerate pain. After the soft tissues healed and postoperative swelling was diminished, the patients were allowed non weight-bearing ambulation with crutches. Progressive weight bearing was encouraged once there was radiographic evidence of callus formation. Bone union was assessed in the outpatient clinic at 4 weeks, 8 weeks, 12 weeks, 24 weeks and 9 months postoperatively. Clinical evidence of infection, incision breakdown, and skin necrosis was recorded. FOLLOW UP: Follow up evaluation is done at 4 weeks, 8 weeks, 12 weeks, 24 weeks.
OBSERVATIONS AND RESULTS The present study consists of 24 cases of fracture of the distal end of tibia. All the cases were operated using locking compression plate. The study period was from October 2013 to September 2017. Functional results were evaluated based on classification system for result of treatment by Oleurd and Mollander scoring system. All Patients were followed up at regular intervals i.e., 4 weeks, 8 weeks, 12 weeks, and 24 weeks. Final assessment at the end of 36 weeks.
Table 1: Oleaurd and Mollander scoring system was used in this study to assess the results
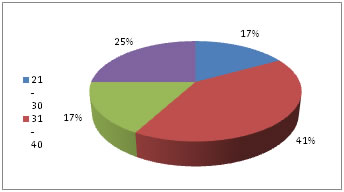
Table 2: Age distribution of patients under study (n=24)
Figure 1: Age distribution (n=24)
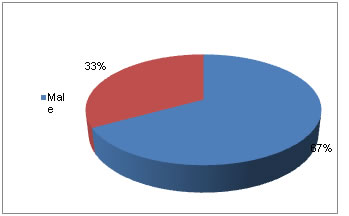
Table 3: Sex distribution of patients under study (n=24)
Figure 2: Sex distribution of patients under study (n=24)
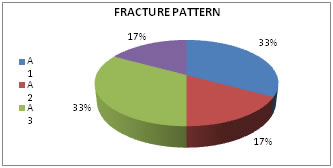
Table 4: Fracture pattern of patients under study (n=24)
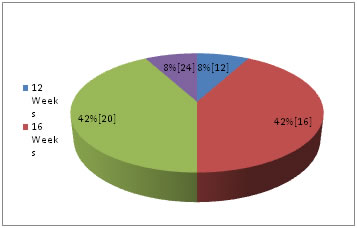
Figure 3: Fracture pattern of patients under study (n=24) Table 5: Radiological Union
Figure 4: Radiological Union (n=24)
Table 6: Functional Outcome
Table 7: Post operative complications of patients (n=24)
Table 8: Comparison of fracture pattern with other studies
Table 9: Comparison of functional outcome
DISCUSSION Fractures of distal tibia are among the most difficult fractures to treat effectively. The status of the soft tissues, the degree of comminution sustained at the time of injury affect the long term clinical results. The goal of operative treatment is to obtain anatomic realignment of the joint surface while providing enough stability to allow early motion. This should be accomplished using techniques that minimize osseous and soft tissue devascularization in the hope of decreasing the complications resulting from treatment. This study evaluated the results and compared them with those obtained by various other studies utilizing different modalities of treatment, our analysis is as follows.
SUMMARY In the present study, 16 cases with fractures of distal tibia in adults were surgically managed by open reduction and internal fixation and 8 cases by minimally invasive percutaneous plate osteosynthesis (MIPPO) using LCP between October 2013 to September 2017 at Kamineni Institute of Medical Sciences, Narketpally. All patients were evaluated clinically and radiologically before and following surgery, for an average period of follow up to 9 months.
CONCLUSION According to present study, 16 patients with fractures of the distal tibia had undergone open reduction and 8 cases by closed reduction through MIPPO techniques of application of the locking compression plates. Locking compression plates (LCP) have the biomechanical properties of internal and external fixations, with superior holding power because of fixed angular stability through the head of locking screws independent of friction fit. Minimally invasive medial plating will restore limb alignment and yield successful clinical outcomes for high energy metaphyseal fractures of the distal tibia19. Despite the significant reoperation rate and prolonged time to union, most patients can expect a predictable return of function. Strong consideration should be given to adjunctive measures in at-risk patients, including those with highly communicated fracture patterns, bone loss, or Type II or III open fractures20. Locking compression plating has resulted in the effective stabilization of these fractures. It does provide adequate stability and allows early motion. The open reduction helps in achieving reduction in difficult situations. Locking compression plating has the greatest advantage in open reduction or closed method (MIPPO. With locking compression plates, anatomical reduction and fracture heamatoma is not disturbed much. Locking compression plating is also effective in extra articular fractures. Intramedullary nails often do not provide enough stability and external fixators usually applied for primary stabilization and until soft tissue edema get subsided and delays the return to work. It is a simple, and straight forward application and has a reduced surgical time in extra articular fractures and intra articular fractures due to newer anatomically contoured locking compression plates for the distal end tibia fractures. Although, a larger sample of patients and longer follow up are required to fully evaluate this method of treatment, we strongly encourage its consideration in the treatment of such complex fractures.
REFERENCES
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home