Official Journals By StatPerson Publication
|
Table of Content - Volume 5 Issue 1 - January 2018
Prospective study of functional outcome of complex extra-articular metaphyseal proximal tibial fractures managed primarily with definitive external fixation
Sachin Kamble1, Atul S Dhepe2*, Rashant Ghule3
1Junior Resident, 2Sr. Resident, 3Assistant Professor, Department of Orthopaedics, Government Medical College Latur, Maharashtra, INDIA. Email: dratuldhepe@gmail.com
Abstract Aim of the study is the functional outcome of complex extra-articular, metaphyseal proximal tibial fractures primarily managed by definitive external fixation. The present study included the prospective analysis of 20 patients of high energy trauma with complex compound extra-articular proximal tibial fracture presented to trauma unit of orthopaedics, Govt Medical College Latur from September 2015 to August 2017. Key Words: extra-articular metaphyseal proximal tibial fracture.
The complex1 proximal tibial fractures, especially in high-energy trauma with associated extensive soft tissue damage, are the most challenging fractures for the Orthopaedic Surgeon to treat not only for the osseous damage but also for the restoration of the soft tissue envelope as well and pose a therapeutic dilemma. Ttreatment of these complex fractures is intended by minimal intervention so as to reduce soft issue complications and postoperative stiffness of the knee joint. Over the years, many treatment modalities have been proposed for these complex proximal tibial fractures. All of them, from simple traction to demanding surgery, presented fair results but also serious complications. Open reduction and Internal fixation with various types of plates and screws is one of the most commonly used modality. Despite the advantages of direct visualization, proper and stable reduction of the fracture surface as well as the acute repair of soft tissue injuries, internal fixation also presents serious disadvantages, including skin or soft-tissue necrosis caused by surgical manipulations on an already damaged soft-tissue envelope and the high rate of infection, deformities, stiffness of knee joint which may compromise the final result.2,3,10,11 The use of a "minimal invasive technique", an external fixator, in the treatment of complex proximal tibial fractures may provide fair reduction results without endangering the soft-tissue elements. Moreover, it facilitates the access to any endangered soft tissue elements requiring interventions along the treatment period.4-9 The recent advances in an external fixation systems including hybrid fixator and their use in proximal tibial fractures has shown promising results.12 It is safe, versatile and effective in providing stability and has minimal impact on underlying soft tissues. It also facilitates early knee motion thus achieving optimal knee function.13 Our present study is confined to assess the clinical outcome and radiological bony union of complex compound extra-articular, metaphyseal proximal tibial fractures primarily managed by definitive external fixation.
MATERIALS AND METHODS The present study included the prospective analysis of 20 patients of high energy trauma with complex compound extra-articular proximal tibial fracture presented to trauma unit of orthopaedics, Govt Medical College Latur from September 2015 to August 2017. Inclusion Criteria: Patients with age above 18 years of both sex. complex compound extra-articular proximal tibial fractures including metaphyseal and metaphyseo-diaphyseal fractures. Exclusion Criteria: Patients with intraarticular(extending to knee joint) fractures. Associated knee dislocations Isolated Diaphyseal tibial fractures. Age below 18 years Methodology: All patients were assessed by thorough clinical examinations to rule out compartment syndrome, neurovascular deficit. Preoperative blood and radiological investigations including anteroposterior and lateral view x ray of tibia and knee joint. 3D CT was done wherever necessary. Uniplanar/biplanar, unilateral/bilateral, delta frame ring fixator was applied in all patients with definitive fracture reduction and thorough debridement lavage done for those with open soft tissue injuries. Intraoperative reduction confirmed by fluoroscopic examination. Approximate stayed sutures were taken for contaminated soft tissues. Postoperative Protocol: From the first postoperative day, patients were put on a physiotherapy regimen consisting of knee mobilization exercises, both passive and active-assisted subjective to pain of patients. Pin tract cleaning with hydrogen peroxide and povidone iodine was done daily.14Sutures removal varied from patient to patient depending on condition of wound. Toe touch partial weight bearing was allowed until radiological union was evident and then gradually to full weight bearing. The fracture union was determined using radiographic and clinical assessment at follow up visits every 4 weeks upto 24 weeks postoperatively. The patient was looked for complications, if any and functional outcome was assessed using the KSS (Knee Society score) criteria.15,16 External fixation was removed once patient walked full weight comfortably with evident solid union on x ray.
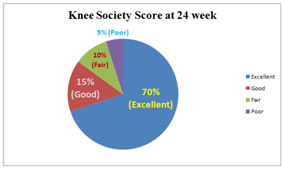
RESULT The data of 20 patients was analyzed prospectively over the above mentioned period. The mean age of patients was 39.4 years (28-54years). 16 were male (80%), while 4 were female(20%), male to female ratio being 4:1. Eight cases involved left tibia (40%) and twelve were right sided (60%). Mean duration of achieving range of knee movements postoperatively was 7.8 days (4-13 days), while that of full weight bearing walking was 12.5 weeks (10-16 weeks). Average duration of follow up was 24 weeks (18-34 week). Mean range of flexion at 24 weeks was 115o (100o-125o).Final outcome at 24 week was assessed using Knee Society Score. In our study, excellent results (KSS > 80) were seen in 14 patients (70%), good results (KSS 70-79) were seen in 3 patients (15%), fair (KSS 60-69) in 2 patients (10%) and poor (KSS < 60) in 1 patient (5%).
Figure 1: Pintract infections occurredin 2 cases (10%), which were managed by intravenous followed by oral antibiotics and regular pin site dressings. The KSS of these two patients was fair at the end of 24 weeks. One patient developed deep infection which not responded to antibiotics which eventually turned up into tibial osteomyelitis. Thorough debridement, sequestrectomy and saucerization was performed at 18 weeks, and antibiotic impregnated beads were kept for four weeks, and at the visit of 22 week definitive open reduction and internal fixation with plating was done. Patient was followed thereafter every 4 week. Patient performed well at the end of one year follow up. Systemic complications and significant functional impairment due to varus/valgus instability were not seen.
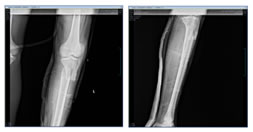
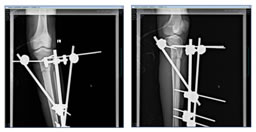
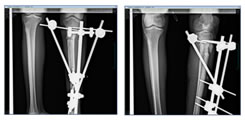
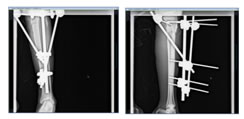
Figure 2(a): Preoperative radiographs( Anteroposterior and Lateral view) Figure 2(b): Postoperative Radiograph Figure 3: Follow up at 4 weeks Figure 4: Follow up at 8 weeks Figure 5: Follow up at 12 weeks
Clinical Photograph Figure 6: Intraoperative At 2 weeks follow up At follow up 24 weeks (Functional KSS) Figure 7: After implant removal DISCUSSION The advent of newer devices and techniques has led many surgeons to use external fixators for the definitive management of the comminuted proximal tibial fractures with excellent outcome.17-20 The Canadian Orthopaedic Trauma Association,21 reported lower rate of early postoperative complications and better functional score in patients treated with external rather than internal fixation, for these fractures. Even in the presence of severe soft tissue compromise, the external stabilization systems, in contrast to traditional techniques of internal fixation, allow for early surgery and hence, early stabilization of the fracture with minimal devitalization.17 Faldini et al, in their study on use of external fixators for proximal tibial fractures reported that average healing time was 24 weeks, nonunion occurred in 1 (3.33%) patient, varus deformity in 2 (6.25%) patients, and the mean knee ROM was 105° (range 75°–125°).22 Catagni et al, in their series of high energy complex tibial plateau fractures treated with external fixator, reported excellent and good results in 30 (50.85%) and 27 (45.76%) patients.23 Weiner et al, were able to obtain a closed reduction in2/3rdof their patients although the other one third required an arthrotomy to obtain an acceptable reduction. They documented an 82% good or excellent result and only one deep infection.24 Comparing treatment of high-grade tibial plateau fractures internal fixation and external fixator, Veri et al. noted high rates of wound complications and reoperation in the open reduction internal fixation utilizing single incision with dual plates group. Their results also suggested that hybrid external fixation is an effective and safe method with a low wound complications rate and early functional return.25 In our study of 20 patients, 14 patients (70%) were found to achieve excellent Functional outcome in the form of Knee Society Score more than 80, good outcome in 3 patients (15%) with KSS in the range of 70-79. Delayed functional outcome with fair results were found in two patients (10%) who acquired pin tract infection initially. Poor results were found in one patient (5%) with associated severely contaminated soft tissue injury preoperatively who subsequently developed deep infection n required staged debridement, sequestrectomy, antibiotic impregnated beads and finally definitive internal fixation. So, at the end of 24 weeks all patients performed well except for one patient. The limitations of this study may have been a lack of direct comparison with other treatment methods, nevertheless it does support the use of external fixator in the management of high energy complex compound proximal tibial fractures with the advantage of minimal surgical intervention in already compromised soft tissue envelope and early mobilization avoiding the stiffness of knee joint. This study can provide a platform for a more detailed comparative study envisaging different treatment modalities in use for such fractures.
REFERENCES
|
|
 Home
Home