Official Journals By StatPerson Publication
|
Table of Content - Volume 5 Issue 2 - January 2018
Functional outcome of tibial plateau fractures: A prospective study
Nishant Panegaon1, Vinay Patil2, Lalit Kumar Joon3*
1Assistant Professor, 2Assistant Professor, 3Postgraduate, Department of Orthopaedics, M R Medical college, Kalaburgi, 585105, Karnataka, INDIA. Email: drlalitjoon@gmail.com
Abstract Background: Knee is commonly injured joint now a day because of increased vehicular trauma and sports activities. We started our study using different methods for treatment of these fractures and studied the effectiveness of the different modalities of these treatments. Material and Method: This is a prospective study, which includes 88 cases having proximal tibial fracture. The fractures were classified using Schatzker‟s classification. Operative patients were evaluated for one year, with serial x-rays at 1,2,3,6 and 12 months. The results were evaluated using the functional grading of Rasmussen scoring system. Result: Out of 88 operated patients of proximal tibia fracture. TYPE 1 (25%) and TYPE 2 (25%) had good to excellent results, TYPE 3 (14.77%) had good results, TYPE 4 (10.23%) had excellent result, TYPE 5 (13%) and TYPE 6 (10.23%) had fair to good result. Postoperative infections were noted in 13 patients of TYPE5 and TYPE6 where severity of injury was high and landed up with stiffness of joint. Assessment was done using the Rasmussen scoring system. Conclusion: In our study TYPE 1 and TYPE 2 was the most common type of fracture pattern. Result of various type of surgeries were good to excellent for various types of fracture pattern except when complications developed in elderly patients of TYPE 5 and TYPE 6 fracture pattern in the form of infection and stiffness. Medial side buttress plating is always desirable in bicondylar fracture pattern with unstable medial condyle, to prevent delayed medial collapse and undesirable varus deformity. Key Words: Schatzker‟s classification, Rasmussen scoring system.
Fractures of the tibial plateau involve the articular surface of the proximal tibia. Tibialplateau fractures are a diverse group of fractures that represent a wide spectrum ofseverity, which ranges from simple injuries with predictably excellent outcomes afternonoperative treatment to complex fracture patterns that challenge even the mostexperienced surgeons. Certain fracture patterns have a high risk of limb-threateningcomplications such as compartment syndrome, although for other fracture patterns theserisks are negligible. New methods have changed the surgical management of both lowenergy lateral plateau fractures and high-energy medial and bicondylar fractures.1 Tibialplateau fractures represent approximately 1% of fractures in adults.Fractures in men occur at a younger age and tend to be the result of high-energy trauma; women have increasing incidence with advancing age particularly the sixth and seventh decades, which indicates these fractures are occurring in osteopenic bone.2 The principles and techniques of treating tibial plateau fractures have evolved dramatically over the last 50 years. In the decades of the 1950s, 60s, and 70s these fractures were predominately treated nonoperatively and published results indicated that favorable outcomes were possible using a variety of techniques including traction, cast bracing, and even spica casting.3,4,5,6 Apley controlled deformity using longitudinal traction, encouraged early knee motion, and reported satisfactory results.3,4 Lansinger et al. in a 20-year follow-up of patients originally reported by Rasmussen showed that nonoperative treatment for fractures with less than 10 degrees of coronal instability resulted in favorable outcomes. 7,8Duwelius and Connolly treated patients with closed reduction with or without percutaneous pin fixation and mobilized them early in a cast brace. They found 89% good and excellent clinical results.9Spica casting after closed reduction led to good and excellent results in 85% of patients. 10Cast bracing was frequently used for tibial plateau fractures as an isolated treatment with satisfactory results. 11With improved methods of internal fixation, operatively reducing and fixing tibial plateau fractures became common in the 1980s. These techniques had the advantages of reducing the articular surface, aligning the limb, and mobilizing the knee early after injury with less encumbering external devices. Similar to nonoperative techniques, favorable results were reported for the majority of patients.12,13,14. The intention of this study is to manage intra-articular fractures of proximal tibia to obtain a stable, pain free, mobile joint and prevent the development of osteoarthritis and to achieve a good functional end result by using plates and cortico cancellous screws.
MATERIAL AND METHODS In a prospective study of 88 cases having tibia plateau fracture, treated in Basveshwara teaching and general hospital attached to MR medical college in the period between Oct 2015 till Oct 2017 were included in this study. SCHATZKERS Classification is used. Inclusion Criteria
Exclusion Criteria
Management in Causality: On admission the patient was thoroughly assessed clinically. The cause of injury wasinquired; vitals parameters were checked; associated head, neck, chest, abdominal injuries were looked for. On local examination skin condition noted, fracture blisters; haemarthrosis; open or closed; distal neurovascular compromise; any signs of compartment syndrome noted. The limb was immobilised in Thomas splint in casualty, later on which was immobilised with A/K slab. Any other associated limb injury or bony injury was noted. According to the general condition and vital parameters intravenous access was sought for and intravenous fluids given accordingly. Other bony injuries were immobilized and appropriately treated. Surgically Treated Group: In the prospective study of 88 cases, depression more than 2-4 mm or split in either sagittal or coronal plane was indication for surgery. Computerized Tomographic evaluation was done in cases which had more comminution and when x-ray was inconclusive and MRI was done in suspected ligamentous and soft tissue injuries. All of the cases in this study were treated operatively, as articular surface reconstruction was the main consideration. There was no strict surgical protocol followed in treating these cases. Most of the cases were operated within 1 week of admission, after swelling and the inflammatory reactions subsided. The patient was suitably anaesthetized-regional or general. Surgery was performed in supine position with or without tourniquet control with image intensifier. All the patients postoperatively were taught and advice to do static quadriceps exercises throughout the day. Partial weight bearing was delayed until 6 weeks, full weight bearing allowed after 12 weeks, depending on the sign of union seen on radiograph. Check x-rays taken after 1,3,6 and 12months. Instruments used in proximal tibial fractures
Implants Used For Internal Fixation: Plates Butresss Plate: Types : T plate L plate Hockey stick plate Locking Compression Plate Screws Cortical screws: 4.5 mm diameter of various lengths for which 3.2mm drill bit and 4.5mm tap is used Cancellous screws
Operative Protocols: Central Depression Fracture: A window is made in the metaphyseal area below the depressed fragment, the depressed fragment elevated and autogenous corticocancellous bone graft packed beneath. Split And Depressed Fracture: Surgical intervention is necessary in a fracture more than 2-4 mm spilt and depressed. The depressed fragment is elevated and autogenous bone grafts from iliac crest are put and then fixed with suitable plates. Total Condylar Depression: Fracture of medial or lateral condyle needs appropriate reduction as malunion may develop with varus or valgus malaligment. The depressed plateau is elevated, articular surface reconstructed and fixed with buttress plate. Bicondylar Fracture: A mid line or two incision technique is used for reduction of both the condyles. Depending upon comminution fixation is done by L, T or hockey stick plate or locked plates and cancellous screws. Dual plating can be done if other side is unstable where collapse may occur. Post Operative Instructions
RESULTS Evaluated using the functional grading of Rasmussen et al.The majority of fractures occur between the age of 20 and 60 years with the maximum incidence of fracture in the age group of 30-40 years (27.27%), followed by 20-30 years (21.59%). Mean age was 43.14 years. In our study male were (79.54%) and female were (20.46%).As most of the area around our setup is rural, most of the patients in our study are farmer by occupation (45.46%).In our study, the majority of the patients treated are due to road traffic accidents or automobile accidents (85.23%).In our study, there was right sided (69.32%) predominance, compared to the left side (30.68%).Majority of patients had undergone ORIF with Buttress Plate (63.64%) Fig.2.In our study the majority of the fracture were found to be of type1- pure cleavage fracture (25%) and type2- cleavage combined with depression fracture (25%).Majority of patients (63.64%) has normal walking capacity. 34.09% of patients had range of movements more than 1400,where as none of the patients had range of movements below 300. (Fig 3) Figure 1: Figure 2: Figure 3: Association Between Type Of Fracture And Rating: COMPLICATIONS CLINICAL RESULTS: Excellent results were in (50%), good results in (39.72%), fair results in (5.68%) and poor results in (4.54%).
Table 1:
DISCUSSION The main purpose of the study is to evaluate the functional outcome of proximal tibia fracture. Our study shows the effectiveness of the operative treatment as the aim was to restore the fracture in anatomical position and fixed with suitable implant for early mobilization. The end results of 88 cases of proximal tibial fractures treated by surgical methods were summarised. The majority of fractures occur between the age of 20 and 60 years with the maximum incidence of fracture in the age group of 30-40 years (27.27% ). Proximal tibial fractures were seen most commonly in the productive and earning age group, because of present day of modernization, industrial development and two wheeler accidents due to inadequate design of bumper. Bourne in 1981 also found that the majority of the patients were aged.
Table 2:
Figure 4 Figure 5
Figure 6
between 15-55 years with an average of 38.5 years, correlates well with the study done by Seppo with 130 patients 1993, which was well correlated with our study of patients aged between 20-60 yr, average 43.14 years. In our study, majority of the patients were males (79.54%). This can be attributed to our Indian setup where the male members were given responsibilities and have to travel for their profession. Occupationally proximal tibial fractures were seen in people with high level of activity, movement and travel on bike. In our study majority of the patients were farmer (45.46%), followed by businessmen (11.36%), employees (11.36%), labor (11.36%), etc. As most of the area around our setup is rural, most of the patients in our study were farmer by occupation. As the farmers were sustain fracture, it is mainly due to automobile accidents. In our study, the commonest mode of injury was the automobile accidents or road traffic accidents being (85.23%). The next very common mode of injury being the, fall from height (10.23%) and domestic injury (4.54%).The incidence of proximal tibial fractures in our study was seen more on right tibial fractures (69.32%) than the left tibial fractures (30.68%).In our study, the majority of the fractures were found to be of type I (25% )and type I I(25%) fracture, which very well correlates with the study conducted by various authors. Type I fractures 22 in number (25%) were the most common group in our study. They were operated because the displacement of articular surface was more than 2mm with CC screw or Buttress plate. These patients achieved full ROM without any deformity and had excellent (81.81%) to good (18.18%) result. Type II fractures were 22 in number (25%). These fractures were also the most common group in our study. All of these patients were operated with Buttress plate. Postoperative follow up of these groups showed excellent (77.27%) to good (22.72%) result. Type III fractures were present in 13 patients (14.77%). These patients were operated with bone grafting and Buttress plate. All the patients showed good result.We have 9 patients (10.23%) of type IV fracture. This patients were operated with Buttress plate to prevent collapse of the fracture fragment and varus deformity. Outcome is excellent. Type V fractures were 13 in number (14.77%). Most of these fractures were displaced and comminuted. All of the patients were treated with Buttress plate from eitherside, depending on the communition. All of the patients have poor (23.07%) to good (61.53%) function. There were 9 cases of type VI fractures (10.23%) which were most comminuted and displaced. This group has poor (11.11%) to good (55.55%) results.The benefits of early knee motion after soft tissue healing, were however to be balanced by risks, including loss of fracture reduction, failure of internal fixation and compromised ligament and soft tissue healing. Schatzker, Robert Mc Broom (1978), Magonliobi and Steven, Gausewitz (1984) stated that the prognosis is given by the degree of fracture displacement, type of fracture, method of treatment and quality of post operative care. Good supervision of the knee joint is required while the patient undergoes range of motion exercises. Out of 88 cases treated surgically, 30 patients (34.09%) had range of movements more than 1400, 22(25%) had more than 1200, 28(31.82%) had it between 900 to 1200, 3(3.41%) had it between 600 to 900 and 5(5.68%) had it between 300 to 600. The benefits of early knee motion include reduced knee stiffness and improved cartilage healing. Patients who had type I and type II fractures were mobilized early and allowed early ROM and early weight bearing. Patients who had type V and type VI fractures were gradually mobilized and weight bearing was delayed, to prevent collapse of the fracture fragment and varus deformity as the strength of the construct was inadequate. Fracture blister was present in 4 case for which surgery is delayed for 2 week, after improvement in the skin condition and treatment with surgical prophylactic intravenous antibiotics. Result is fair in this case. Post operative infections were noted in 13 patients of type 5 and type 6 fractures. Out of which 5 were acute and 8 were chronic. In acute cases one required implant removal for whom external fixator was applied later on and other were managed with wound wash, intravenous antibiotics and dressing with or without vaccum assisted closure machine but showed poor result. Chronic cases were presented with discharging sinus in which wound lavage along with antibiotic therapy given and implant was removed after fracture union. These patients were managed with prolonged immobilization after surgery and delayed weight bearing which ultimately resulted in stiffness of joints. So even though meticulous articular reconstruction is achieved infection resulted in poor outcome. Inspite with all these complications we achieved 50% of excellent results with our surgical method using various fixation methods,39.72% good result, 5.68% poor and 4.54%fair results. These results were comparable to various authors. Rambold in 1992 had 93 % acceptable results using rigid internal fixation. Seppo E and Honkenen from university hospital, Tampere, inland, reported 86% of statisfactory results. Joseph schatzker, Robert Mc. Broom from the wellsetey hospital, Canada reported 86% of satisfactory results which was more than the conservative treatment. So it appears that poor results in the entire study belong to type 5 and type 6 fracture pattern and complication is mostly due to infection.
CONCLUSION The aim of the management should be to obtain stable, painfree, mobile joint and to prevent secondary osteoarthritis with good functional end result. Infection plays a vital role in influencing the result of the outcome. Rigid internal fixation is mandatory. Excellent results were obtained in 44 (50%) of cases. Majority of Type 1- Pure cleavage fractures and Type 2- Cleavage combined with depressed fractures gave excellent results when fixed with buttress plate and screws. Poor results in the entire series belong to type 5 and type 6 fracture pattern and complication is mostly due to infection.As the duration of study and follow up was short, it is difficult to comment about past-traumatic osteoarthritis. A longer follow up is required to comment about it.
REFERENCES
|
|
||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home
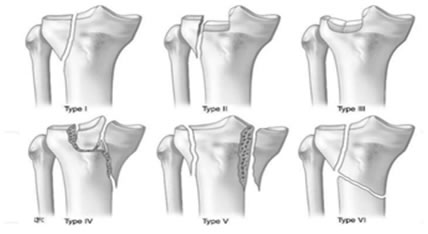
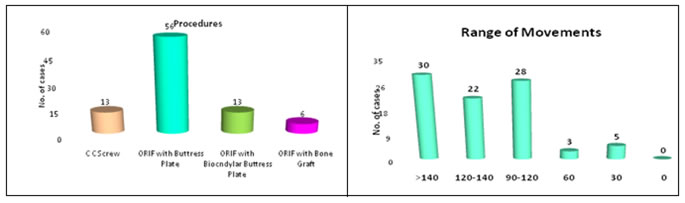
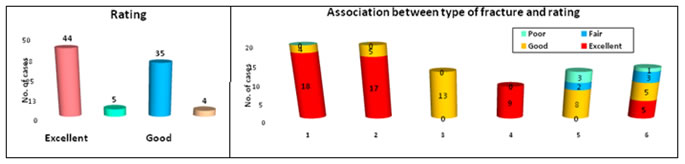 Figure 7
Figure 7