Official Journals By StatPerson Publication
|
Table of Content - Volume 5 Issue 3 - March 2018
Plating of fibula in the management of distal metaphyseal tibial and fibular fractures - A prospective study
Srinivas Y1, Srikanth G2*, Vikramsimha Reddy3, M E Luther4
1Associate Professor, 2Sr. Resident, 3Jr. Resident, 4Professor and HOD, Department of Orthopaedics, Kamineni Institute of Medical Sciences, Sreepuram, Narketpally, Nalgonda (Dist)-Telangana.508254, INDIA. Email: srikanthgourla05@gmail.com
Abstract The tibia is exposed to frequent injury. Distal tibial metaphyseal fractures are often the result of high-energy trauma, usually associated with distal fibular fractures. The presence of the ankle joint allows rotatory deformity after fracture, and care should be taken during reduction to correct such deformity. Fixation of fibular fractures in distal tibial metaphyseal fractures is controversial, although fixation of the fibular fracture by a plate and screws partially stabilizes comminuted fractures of the distal tibial shaft or metaphysis and considered in distal tibial fractures treated with intramedullary fixation to prevent valgus deformity even there is increased potential for delaying the tibial fracture healing. Objectives: The purpose of this study was to compare the functional and radiological outcome of fractures of distal third tibia and fibula treated by interlocking nail of tibia with fibular plating and without fibular plating. Material and Methods: A total of 24 patients who had fractures of lower third tibia and fibula are included in this study. 24 patients were divided into two groups A and B (12 patients in each group) based on fibular fixation. Results: Functional results were evaluated based on classification system for result of treatment by Johner and Wruhs criteria. Functional Outcome according to Johner and Wruhs criteria based on clinical rotational alignment, radiological valgus angulation and ankle range of movements, in group A 7 patients (58%) had good results and 5 patients (42%) had fair results. In group B 8 patients (67%) had good results and 4 patients (33%) had fair results (p=1.00 statistically not significant). Conclusion: Based on the results of the study, it was confirmed that fixation of fibula first, along with interlocking nailing of the tibia maintains limb length and decreases the malalignment and malrotation of the tibia in distal third fractures of tibia and fibula as compared with only interlocking nailing of tibia in distal third fractures of tibia and fibula. Key Words: Distal tibia fractures, Intramedullary nailing, Fibula plating.
Distal tibial fractures represent less than 7% of tibial fractures. Metaphyseal fractures of distal tibia comprises 15% of all fractures of distal third of the tibia. Often caused by high-energy axial compression, low energy rotational forces. High energy injuries involve ipsilateral fibular fractures in 80% of cases1.These fractures are unique as distal tibia is relatively a less vascular bone. Severe soft tissue injury and bony comminution are common in these injuries2. These fractures can be treated conservatively or surgically by using external fixator, dynamic compression plates (DCP), limited contact-dynamic compression plates (LC-DCP) or locking compression plates (LCP) or intramedullary nails2,3. Cast treatment cause prolonged immobilization with loss of reduction and decreased ankle movements. External fixator complications are stiff ankle, pin tract infections, septic arthritis, malalignment, loss of reduction and delayed union. Traditional open reduction and internal fixation with plate and screws requires extensive exposure with possible devascularization of the bone, wound dehiscence and infection. The subcutaneous location of plates may lead to symptomatic hardware requiring its removal. Recent techniques of minimally invasive osteosynthesis using locked plate and screws show good fracture healing and minimal complications. Locking intramedullary nailing is widely used in the treatment of displaced tibia and fibula fractures including those with soft tissue and open injuries2,3,4. Intramedullary interlocking nailing is minimally invasive and spares extra-osseous blood supply, and load sharing in nature. Their role in the treatment of distal third shaft and metaphysis is controversial due to difficulties in fracture reduction, iatrogenic fracture and inadequate fixation leading to malalignment. The distal widening of medullary canal prevents tight endosteal fit of the nail and compromises the reduction leading to rotational and angulatory deformity. When associated with distal metaphyseal fibular fractures, the fixation of fibular fracture has been suggested to decrease the incidence of angulations (varus/valgus), malrotation of tibial fracture and improves stability of fixation. Any malunion can disrupt the biomechanics of the ankle and foot joints leading to early arthritis of these joints. So there exists a debate whether or not fibular fixation in distal third tibia fractures is required as an adjuvant to intramedullary nailing of tibia. Hence it is hypothesized that fixation of fibula decreases malalignment, malrotation and increases the stability of fixation in combined distal tibia fibula fractures. In this study an attempt has been made to analyze the results of treating such fractures by interlocking intramedullary nailing of tibia with or without fibular fixation.
MATERIALS AND METHODS This was a prospective randomized study done from October 2014 to September 2016 at Kamineni institute of Medical Sciences, Narketpally. Patients with fractures of lower metaphysis of tibia and fibula were taken for this study after obtaining their informed valid written consent. Patients age above 19 years, closed fractures of distal third tibia and fibula (AO A1, A2, A3), Gustilo-Anderson type I open fractures of distal third tibia and fibula are included in this study. Patients below 19 years, pathological fractures, Gustilo-Anderson type II and III open fractures of distal third tibia and fibula, associated neurovascular injury, patients with intra-articular fractures and segmental fractures of fibula were excluded.24 patients with fractures of lower third tibia and fibula are included in this study to compare the functional and radiological outcome of fractures of distal metaphysis of tibia and fibula treated by interlocking nail of tibia with or without fibular plating. 24 patients are divided into groups A and B (12 patients in each group) based on fibular fixation. Group A: patients treated with intramedullary interlocking nailing tibia without fibular fixation. Group B:patients treated with intramedullary interlocking nailing tibia with plating of fibula with 3.5mm one third tubular plate and screws, study done by simple randomization method, on admission first patient was grouped into group A and second patient into group B, alternatively all are divided into two groups (12 patients in each group). A careful history was elicited from the patient and clinically examined for general condition and local injury for swelling, deformity and loss of function. Palpation revealed tenderness, crepitus and abnormal mobility at the fracture site. Distal neurovascular status of involved limb was checked. Antero-posterior and lateral radiographs of the affected leg along with knee and ankle were taken and confirmed. The limb was then immobilized in an above knee POP slab till swelling subside and necessary investigations and pre anaesthetic check up was done and consent was taken and definitive fixation was done for fracture tibia by closed reduction and internal fixation with interlocking nail and fracture fibula by open reduction and internal fixation with one third tubular plate and 3.5mm cortical screws.
RESULTS Functional results were evaluated based on classification system for result of treatment by Johner and Wruhs criteria. All Patients were followed up at regular interval i.e.4 weeks, 8 weeks, 12 weeks, and 24 weeks. Final assessment was done at the end of 36 weeks (9months).In the present study age of the patients ranged from 20-67 years with an average of 43.37 years. 21 (87%) patients were males and 03 (13%) patients were females showing male preponderance.19 (79%) of patients sustained injury following road traffic accidents and 05 (21%) patients sustained injury due to fall. The fracture pattern was classified based on A.O classification (43) for fractures of distal tibia and fibula (43), of the 24 cases studied, 21 (88%) cases were Al, 2 (8%) were A2 and 1 (4%) were A3. A1 fractures were more common. All fractures in this study were closed fractures. The mean time of union in patients in group A patients was 5.08months and in group B was 5 months (p=0.023 statistically significant).The average external rotation deformity in patients of group A was 8.660 and for in group B was 8.000. In group A 58% of the patients had good results and 42% patients had fair results. All patients in group B had good results (p=0.014 statistically significant).The average valgus deformity of the tibia in group A was 7.250and in group B was 5.660. All the patients in group A had fair results. In group B 50% of patients had good results and 50% of patients had fair results (p=0.042 statistically significant).Ankle range of movements in group A, 67% of patients had good results and 33% had fair results. In group B, 67% of the patients had good results and 67% had fair results (p=1.00 statistically not significant).Functional Outcome according to Johner and Wruhs criteria based on clinical rotational alignment, radiological valgus angulation and ankle range of movements, in group A 7 patients (58%) had good results and 5 patients (42%) had fair results. In group B 8 patients (67%) had good results and 4 patients (33%) had fair results (p=1.00 statistically not significant).
Figure 1:
DISCUSSION The distal part of fibula plays an important role in the biomechanics of the ankle. Locked intramedullary interlocking nail concerns include the insufficient stability of fracture fixation, risk of propagation into the ankle joint, and delayed / nonunion with break of nail and locking screws. The present study examined the necessity of fibular fracture fixation to help in prevention of ankle malalignment (varus/valgus and rotational) after intramedullary interlocking nail of distal tibia fractures3. In this study the average age of patients with such injuries was found to be 43.3 years (20-67). The average age of patients in present study is comparable with the studies of M. Berlusconi et al (2014)5. Present study showed male preponderance as reported by R.Buzzi et al (2009)2. In the present study road traffic accidents was most common mode of injury and intra-articular fractures are excluded, only extra articular fractures are included (type A). Type A1 fracture pattern was most common which is comparable with studies of M. Ehlinger et al (2009)6. The average time of union in group A patients was 5.08 months and in group B was 5 months (p=0.023). Fracture union was achieved in all patients in both groups. Present study was comparable with Prasad.M et al (2013)7. There are no nonunion or delayed union in this study probably as all patients had closed fractures, the average valgus angulation was less (i.e. 5.660), when compared to group B (7.250). In group A all the patients had fair results and in group B 6 patients had good results and 6 patients had fair results. Fibula fixation establishes the length of the lateral column. If fibula fixation is done prior to nailing of tibia, it helps to restore the alignment of proximal and distal tibial fragments. This may be the reason for less valgus angulation in cases where the fibula was fixed (statistically significant p = 0.042).The average external rotation at ankle was less i.e. 8.000 in group B as compared to 8.660 in group A (p = 0.014). In group A 7 patients had good results and 5 patients had fair results and in group B all the patients had good results. Range of movements at the ankle was statistically not significant (p = 1.00) between the two groups i.e. in group A, 67% of patients had good results and 33% had fair results. In group B, 67% of the patients had good results and 33% had fair results. B.C Taylor et al (2015)8 reported valgus/varus malalignment in 28 patients out of 83 inpatients without fibular fixation group and 6 out of 15 patients in fibular fixation group but in present study all the patients, whether fibula was fixed or not, there was valgus angulation at the fracture site. The probable reasons were the relatively wider diameter of the distal fragment decreases the amount of fixation with less contact surface between the nail and bone; this can result in the distal fragment going for valgus/varus angulation3,7. T. Schepers et al (2011)9 in their study included 205 patients with distal fibular fractures in which 165 patients received 1/3 tubular plates and 40 patients were treated with locking plates. Wound complication rate was 5.5% in conventional plating group (1/3 tubular plate) and 17.5% in locking plate group. In the present study the entire fibula fractures in group B received 1/3 tubular plates and there are no wound complications noted. Present study showed reduction of valgus angulation in fractures treated with fibular plating compared to tibial nailing alone. In the present study fibula was fixed first in group B which maintained the length of the leg and reduces rotational and valgus malalignment when compared to tibial nailing alone. Guilherme Boni (2015)10 stated that in distal third tibial shaft fractures undergoing intramedullary nail fixation, adjunct fibula fixation may allow for achieving and maintaining fracture reduction of the tibia and improvement seen in clinical outcomes. Shan Wei Yang et al (2005)11 had done plating for all associated fibular fractures and noted no rotational deformity postoperatively. Therefore, they support performing fibular plating first before the treatment of distal tibial fractures.
Table 1: Comparison of Functional Outcome between both groups under study according to Johner and Wruhs criteria based on clinical rotational alignment, radiological valgus angulation and ankle range of movements (n=24)
CONCLUSION
REFERENCES
|
|
 Home
Home
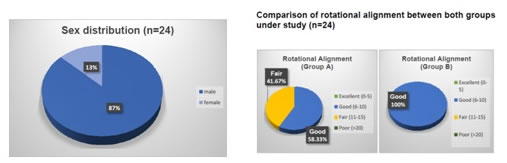 Figure 2:
Figure 2: