Official Journals By StatPerson Publication
|
Table of Content - Volume 6 Issue 1 - April 2018
Functional outcome of complex proximal femur fractures treated with proximal femoral locking plate
L Y Sathyanarayana1, R V Adhiyaman2*
1Assistant Professor, 2Sr. Resident, Department of Orthopaedics, Shri Sathya Sai Medical Collage and Research Institute, Ammapettai, Sembakkam Post 603108, Chengalpattu Taluk, Kancheepuram Distric, Tamil Nadu, INDIA. Email: sathyanarayana2231@gmail.com
Abstract Background: Subtrochanteric femur fractures are the most devastating injuries and are one of the leading causes of hospital admissions. Proximal femur locking compression plate (PF-LCP) represents a feasible alternative for the treatment of unstable subtrochanteric fractures. Aim: To study the functional outcome of complex proximal femur fractures treated with proximal femoral locking plate. Material and Methods: This study was conducted on 20 admitted adult patients with complex proximal femur fractures with communition and osteoporosis. The fractures were classified by Boyd and Griffin classification along with Seinshemier’s classification. The functional outcome was evaluated by Harris hip score. Results: The mean time for full weight bearing was 16 weeks and 90% of cases showed bony union at 6 months follow up. Good to excellent results were seen in 95% of cases (functional outcome). Conclusion: Proximal femoral LCP is a satisfactory method of treatment in subtrochanteric femur fractures with comminution and osteoporosis. Key Words: Subtrochanteric femur fractures, fracture fixation, Proximal femur locking compression plate, functional outcome.
INTRODUCTION Subtrochanteric fractures are femoral fractures where the fractures occur below the lesser trochanter to 5 cm distally in the shaft of femur.1 They have a tremendous impact on both the health care system and society in general. These fractures are noted for their higher incidence of unsatisfactory results after operative treatment. Proximal femur fractures comprise, fractures of intertrochanteric and subtrochanteric region. In case of subtrochanteric fractures the incidence of limb shortening, medialization of distal fragment and implant cut outs is high. This led to the development of newer methods like intramedullary devices and proximal femoral locking compression plate (PF-LCP). PF-LCP represents a feasible alternative for the treatment of unstable subtrochanteric fractures. It provides the surgeon with the flexibility to achieve plate to bone apposition as well as axial compression or angular stability.2,3 Subtrochanteric fractures are complicated by delayed or non union. In view of these considerations, the present study was undertaken to study the functional outcome of complex proximal femur fractures treated with proximal femoral locking plate.
MATERIAL AND METHODS This study was conducted on 20 admitted adult patients with complex proximal femur fractures with communition and osteoporosis were selected according to inclusion criteria. The fractures were classified according to Boyd and Griffin’s classification4 and Seinsheimer’s classification.5 The cases were followed at regular intervals. This study was conducted with due emphasis for clinical observation and analysis of results after surgical management of complex proximal femur fractures with proximal femoral LCP. Inclusion Criteria
Exclusion Criteria
At the arrival of the patient with suspected proximal femur fracture, patients were resuscitated depending on their general condition. Fracture was stabilized using Thomas splint, alternatively with skin traction. Routine laboratory investigations were done including echocardiogram. X-rays of pelvis with both hips-AP view, hip with femur full length of involved side-AP and lateral views and Chest –PA view. Preoperative planning
Operative Procedure: After induction of anaesthesia, patient was placed in the supine position on the fracture table with adduction of the affected limb by 10-15 degrees and closed reduction of the fracture was done with traction and rotation. The tip of the greater trochanter was located by palpation or occasionally by using image intensifier in obese patients. A 6-8 cms vertical incision was taken from the tip of trochanter in distal direction along the shaft of femur. Fascia lata was opened in line with the incision and gluteus medius and vastus lateralis muscles were split in line with the fibers and tip of the trochanter and proximal femur exposed. Prior to placing the plate on the bone, thread the wire guides into the plate holes for each of the three proximal locking screws. Use the wire guide 7.3 in the two proximal screw holes, and a wire guide 5.0 in the third locking screw hole. The wire guides can also be used as a manipulation aid for positioning the plate on the proximal femur. Using fluoroscopic image control (AP and lateral), guide wire was inserted through the wire guide in each of the three proximal locking holes. The proximal wire was ideally placed slightly posterior to central in the lateral view. Accurate positioning of the proximal guide wire (and ultimately the locking screw) assures frontal plane alignment. Patients were encouraged to sit in the bed next day and were taught quadriceps strengthening exercises and knee mobilization. In patients with stable fixation toe touch weight bearing with walker or axillary crutches was encouraged as per pain tolerance of the patient. Sutures were removed on day 11 or 12. Patients were discharged from the hospital at 2 weeks with partial weight bearing with help of walking aids. Follow up: All patients were followed up at 2 weeks, 6weeks, 12 weeks, 6, 9 and 12 months. At every visit patient was assessed clinically regarding hip and knee function, walking ability, shortening and fixation defects. X-ray of the involved hip with femur was done to assess fracture union and implant bone interaction. The functional outcome of the patient is assessed by Harris hip score whose components are as follows. RESULTS In this study of 20 patients with complex proximal femur fractures,12 were male and 8 were female with mean age being 60 years. 75% of the cases in the study were due to road traffic accidents and 25% cases were due to low energy trauma from trivial fall. Both right and left side were equally affected. Communited subtrochantric fracture constituted 15 cases and subtrochanteric fracture with proximal femur extension in 5 cases. Mean duration of hospital stay was 10 days. Mean time for full weight bearing was 16 weeks and 90% of cases showed bony union at 6 months follow up. Good to excellent results were seen in 95% of cases (functional outcome).
Table 1: Functional results of subtrochanteric fractures
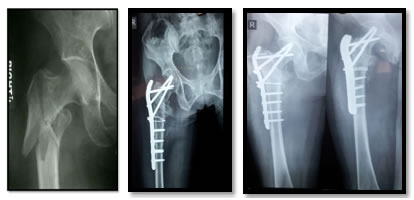
Figure 1: Pre op x-ray Figure 2: 3months post op Figure 3: 6 months post-op
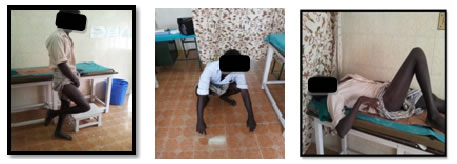
Figure 4: Knee flexion Figure 5: Squatting Position Figure 6: Hip Flexion
Figure 7: Preop x-ray Figure 8: 3 months post op Figure 9: 6 Months post-op
Figure 10: Squatting Figure 11: Sitting position DISCUSSION Early operative treatment of subtrochanteric fractures reduces both mortality and morbidity giving best chance of early independency and reducing the risks of prolonged bed rest. In the management of subtrochanteric fractures of femur, it is utmost importance to re-establish bone to bone contact of the posteromedial cortex. Sliding nail plate systems have given good results for both stable and unstable subtrochanteric fractures with reported complication rates of 3% to 15%.6 The Cephalomedullary nails like Gamma nail, Proximal Femoral Nail attempts to combine the advantages of a sliding lag screw with those of intramedullary fixation while decreasing the moment arm as compared with that for a sliding nail plate system. In the early 2000, the new locking compression plate was introduced, which allows angular-stable plating for the treatment of subtrochanteric and osteoporotic fractures, shown to be clinically effective with low complication rates.7 The Proximal femoral LCP is a precontoured specially designed for the right and left femur to accommodate average femoral neck anteversion. The convergent angle design of 95, 120, 135 and the locking interface of the proximal 7.3 mm (first and second), 5.0 mm (third) cannulated locking screws should alleviate and improve proximal femoral fixation, especially in osteopenic bone. The remaining in the plate shaft are combination holes which allow the placement of either a cortical (4.5mm) or locking head screw (5.0mm). This provides the surgeon with the flexibility to achieve plate to bone apposition as well as axial compression or angular stability. In our study the Mean age at fracture was 60 years. The common mode of injury being high velocity (RTA) and fall from height accounting for 75% of the cases. There were difficulties in placing all the 3 proximal screws into the head through neck in 5 cases and also placement of the plate along the shaft in 2 cases. This is attributed to the pre-contouring of the plate and different neck shaft angle and ante-version in individual patient and also due to low to moderate built of the patients in our region. In our study, the average operation time was 1 hr and 30 mins, with average amount of blood loss being 100 ml and duration of radiation exposure being 20 mins. The average length of incision in our study was 18 cms with bigger incision needed in communited fractures with subtrochanteric extension. The length of the plate being from 4-16 holes. The greater trochanter fragment and the lateral trochanteric wall play an important role in stability after implant fixation of subtrochanteric fractures. The PFLCP can be a feasible alternative for the treatment of unstable subtrochanteric fractures because it provides proper fixation of the lateral fragments and prevents the lateral migration of proximal fragments. In our study, 90% of the cases showed bony union at 3 months follow up and 50% of cases showing bony union at 6 months follow up. One case showed infection which was managed by removal of implant and by conservative methods. Zha GC et al reported union rate of 98% and 95% at 3 months, 6 months follow up respectively.8 In a study by Govindasamy R et al, the union rate with proximal femoral fractures at the end of three months was 89%, at the end of 6 months was 94% and had 100% union at one year follow up.9 To conclude, our study showed that proximal femoral LCP is a satisfactory method of treatment in subtrochanteric femur fractures with comminution and osteoporosis which showed good to excellent results in 95% of cases (functional outcome).
REFERENCES
|
|
 Home
Home