Official Journals By StatPerson Publication
|
Table of Content - Volume 6 Issue 1 - April 2018
Results of radical posteromedial release (RPMR) in neglected CTEV: A prospective clinical study
V R Rokade*, Anant Chowgule**, Pankaj Lawate***
*Associate Professor, **Assistant Professor, ***Sr. Resident, Department of Orthopedics, Government Medical College Miraj, Maharashtra, INDIA. Email: drvikas852@gmail.com
Abstract Objective: The aims of treatment are to give supple, flexible, pliable and cosmetically acceptable plantigrade foot in patients of neglected ctev with minimum complications by RPMR. The objectives are to find the correlation between clinical results and with radiological findings. Methods: It is prospective study of treatment of CTEV. Total 30 patients of neglected ctev were studied. These patients were operated by Radical posteromedial release (RPMR). All relevant pre and perioperative information and complications were recorded. Also assessment of functional outcome was made. Results: In present series satisfactory results (excellent and good) were noted in 35 feet (74.46%) and unsatisfactory results (fair and poor) in 12 feet (25.54%). Conclusion: Radical posteromedial release (RPMR) is very helpful in treating neglected congenital talipus equionovarus ( CTEV ) patients. Key Words: CTEV, RPMR.
INTRODUCTION Talipes equinovarus is the commonest deformity of the foot. Clubfoot is one of the most common congenital deformities affecting about 1 infant in every 1000 births. Worldwide approximately 1,00,000 new cases of clubfoot occur each year which if uncorrected leaves infant to face a life of disability 1. Because of awareness number of patients treated with ponsetty cast one of the conservative modality are increased but still in rural areas patients who are having neglected ctev present late to us. Those patients majority above one or two years are treated with radical posteromedial release 2.
MATERIALS AND METHODS At Govt Medical College Hospital Miraj and Padm. Vasantdada. Patil Govt. Hospital Sangli patient who underwent radical posteromedial release (RPMR) from January 2014 to December 2016 were evaluated. All the patients in this study are with idiopathic neglected CTEV. All these patients were managed by RPMR with two incisions. The extent of soft tissue release depends on severity. Lateral release done in very severe cases.30 patients were operated by McKay’s13 procedure with modified Carrols6,15 incision. When patient was admitted, detailed history was taken and type of deformity noted. The deformity is graded as mild, moderate and severe. Grade I : Mild – Malposition is less marked, the rigidity, especially that of the equinus gives way easily and the foot can be brought into normal position without force. Grade II Moderate – Distinct malposition, less rigid than the former and can be molded at least partially close to normal. Grade III Severe Clubfoot: Extreme malposition which because of its rigidity cannot be brought even close to normal position. Physical examination was done to note severity of deformity and graded accordingly. All feet operated in this study had moderate to severe type of deformity. After surgery on a follow up examination all feet were evaluated clinically and radiologically in detail as outlined by Dan Atar et. al1. The rating system combined objective clinical assessment and subjective and radiographic criteria. A total score of 100 points indicated a normal foot. This included a maximum score of 15 points each for ankle range of motion and function, 10 points each for subtalar motion, position of heel while standing, gait, appearance of the forefoot, pain and radiographic criteria and five points each for the type of shoes worn and flexor tendon function. A score of 85 to100 points was classified as excellent, 70 to 84 points good, 60 to 69 points fair and less than 59 points poor. Functional rating system for clubfoot surgery is given below (Dan Atar et.al1.)
Table 1: T.C. Index is the sum of the talocalcaneal angles measured on lateral and anteroposterior radiographs.
At the time of follow-up, radiographic examination in detail and following angles were measured- AP Talocalcaneal angle, Lateral talocalcaneal angle, Talo First Metatarsal angle Tibio-calcaneal angle Operative Technique Radical Posteromedial Release: Total 30 patients (50 feets) were treated by radical posteromedial release5. Patients planned for surgery were admitted two days before the day of operation. All necessary investigations Hb, CBC, urine examination were done. Surgical fitness from the paediatrician is taken. Preoperative anaesthetic check up was done and as suggested by the anaesthesiologists, Inj.Atropine 0.3mg( i.m.) administered 30 minutes before surgery. All procedure is done under general anaesthesia. A pnumatic tourniquet is applied to the midthigh region. Foot and leg is first cleaned with 2% savlon, starting from the tip of the toes to the knee and then iodine was painted all over the foot and leg. The part was covered with sterile drapes. Tourniquet inflated. Tourniquet time was noted by anaesthesiologists. Position: Supine position given with sandbag kept under opposite hip. So that posteromedial part of leg and foot will come into operative field. Incision: Modified Caroll’s incision6 is taken. Posterior Incision: While assistant holds the foot in dorsiflexion the post. incision taken slightly lateral to the tendoachilles from it’s insertion to 5-6 cm.above. Sural nerve is identified and protected. Incision deepened till the glistening sheath of tendoachilles is seen. The sheath of T.A. is released. The ‘z’ plasty of the tendoachilles is done. Plantaris tendon is identified and cut. The neurovascular bundle is located medially and was identified by the bluish discolouration of the posterior tibial vein. It was retracted with a wet tape gauze passed around it. The superior peroneal retinaculum is cut and ankle joint is identified by passive upward and downwards movements of the ankle joint. First a small incision is made and then the capsulotomy is completed. Posterior talofibular ligament is cut by extending the capsular incision laterally to the fibular side. The posterior talocalcaneal and calcaneofibular ligament which is the main tether on lateral side are released. Then sheath of the peroneal tendon was cut alongwith the tibiofibular syndesmosis. Medial Incision: A gently curved incision is taken from the base of the first metatarsal curving below the medial malleolus towards the tendo Achilles, two fingerbreadths anterior to it. The subcutaneous tissue dissected and the neurovascular bundle (med. and lat. plantar nerves and associated vascular components) was protected. The tibialis posterior (T.P.) tendon is identified. The sheath of tibialis posterior entered just post. to and above the medial malleolus. The tendon traced downward up to talonavicular joint and then ‘z’ plasty of T.P. is done. The talonavicular joint is opened by pulling on the remaining tibialis posterior tendon and then the capsule of talonavicular joint released all the way around med., inf., sup. and lat.aspect. The superficial deltoid, dorsal talonavicular ligament, plantar calcaneonavicular ligament (spring ligament) cut close to navicular. The Master knot of Henry is identified and released. The tendons of flexor digitorum longus (F.D.L.), and flexor hallucis longus (F.H.L.) are freed, and traced proximally until talocalcaneal joint is entered. “Z” plasty of FHL and FDL is done. The medial capsule of the talocalcaneal joint is released along with superficial deltoid ligament. The interosseous talocalcaneal ligament is kept intact. Both ends of bifurcated Y ligament are cut. Then the naviculo-cuniform joint is released. The abnormal origin of abductor hallucis is also released. The cut ends of T.P., FDL, FHL are sutured to each other with 3-0 ethilon suture. Through normal saline and betadine wash is given. Steindlers procedure- Stab incision is taken below and posterior to medial malleolus through which plantar fascia is cut and the origin of quadratus plantae is stripped in cases of severe cavus deformity. Internal fixation: After reduction of navicular on talus, the talonavicular joint is fixed with ‘K’ wire. Anather ‘K’ wire is passed from plantar aspect of calcaneus into the talar body after reducing calcaneus under talus. Tourniquet is released and vascularity is checked. Then subcutaneous sutures are taken with 3-0 vikryl. The skin is closed with 3-0 ethilon. Wound is dressed with betadine gauze. Above knee C.T.E.V. cast is given in corrected position and splitted longitudinally. Postoperative Management: The operated extremity is kept elevated over the pillow. Injectable antibiotics-Inj. Cefotaxime and inj. Gentamycin are given intravenously according to the body weight for three days and afterwards switched over oral antibiotics in syrup form for next four days. If the deformity is bilateral other side is operated after two to three days. On fifth postoperative day if the swelling is reduced, distal neurovascular status is checked, the cast is reinforced and patient is discharged. On the first follow-up, after one month the cast is removed, the sutures and “K’’ wires are removed radiographs are taken and the correction is assessed. Again above knee C.T.E.V. cast is given for three weeks. On the second follow-up below knee C.T.E.V. cast is given after taking shoe measure. After three weeks cast is removed and C.T.E.V. shoes are given. The shoes are continued till five years. Radiographic assessment done on each follow up after three months in first year and at six months afterwards. OBSERVATIONS In the present series, there were 25 males and 5 females making the ratio of 5:1.
Table 2: Distribution of cases as regards the gender and incidence of involvement of extremities
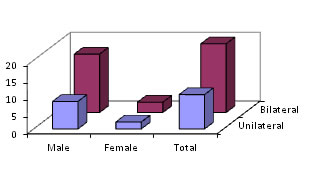
From above data, it is obvious that bilateral cases are 83.33% and unilateral are 16.66%. Graph showing distribution of cases as regards the gender and incidence of involvement of extremities Figure 1:
Table 3: Type of deformity and number of feet
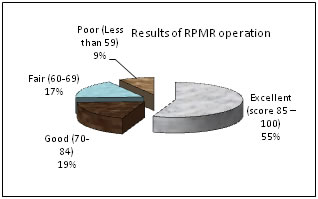
47 feet (30 patients) were operated by this method and results were studied as per the score chart (Dan Atar et. al.) It is clear that satisfactory results (excellent and good) were noted in 35 feet and unsatisfactory results (fair and poor) in 12 feet (25.54%)
Table 4: Results of RPMR operation
Figure 2: Table 4: Type of deformity and clinical results
Nine feet belonging to moderate deformity obtained unsatisfactory results. Most of the moderate type (21 feet) obtained satisfactory results. While 3 feet in severe grade had a failure.
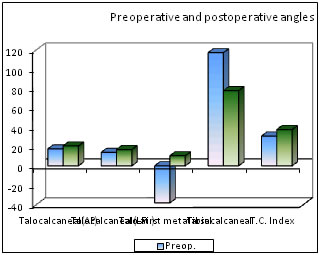
Table 5: Preoperative and postoperative angles
Figure 3: Table 6: Clinical results and ranges of parameters
Comparison of clinical results as (Excellent, Good, Fair, Poor) with respect to talocalcaneal angles in anteroposterior, lateral films and with T.C.index (sum of talocalcaneal angles in AP and Lat. view) was done.
Table 7: Postoperative complications
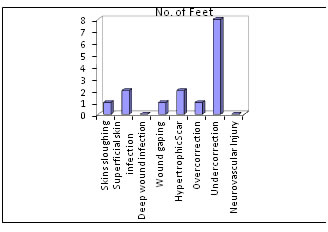
Undercorrection is observed in majority of cases (17.02%) as evidenced by residual forefoot adduction, equinus at ankle, heel varus while other complications are small in number. Neurovasular injury or deep wound infection is not noted in any case.
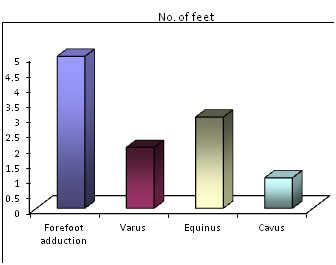
Figure 4: Table 8: Residual deformities
It is obvious that forefoot adduction is the most common residual deformity.
Figure 5: DISSCUSSION Clubfoot is still a major problem to all of us. Various theories regarding its etiology fall short on some vital point, its pathology is not clear. With Ponsetty’s cast treatment the requirement of major surgical procedures is reduced. But due to lack of awareness in rural areas cases of neglected ctev are still there. The aim of present study was to study the results of Radical Posteromedial Release (R.P.M.R.) operation in details3,4. To find residual deformities and their correlation with radiological findings, to study various deciduas such as calf atrophy which are accompaniments of clubfoot surgery in each case and finally to analyse the surgical results7. In the present series, 30 clubfoot patients were studied, 25 males and 5 female showing M : F = 5 : 1 with 83.33 % male and 16.67 % females. Turco13 in his series of 468 patients found 334 (71.36 % ) males and 134 (28.63 % ) female having a ratio of 2.5 male to 1 female. Debrunner gives 58.6 % boys and 41.4 % girls. Max bohm gave the sex ratio 4: 1. Ponsetti found six male to one female. Kite in his series of 1509 patients found 70.58 % males and 29.42 % female. Thus the literature varies as to the percentage of boys to girls in clubfeet. Thus, the finding of 5 : 1 affection more in boys than girls coincides with the series in literature. In the present series 20 patients were bilateral (66.67%) and 10 patients were unilateral 33.33 %.Turco13 in his series found 56.76% bilateral cases. Chung reported bilaterality in 55.75 % cases. Kite found in his series 49.37 % bilateral cases. Ponsetti11 found 40% bilateral cases. Preponderance of bilateral cases coincides well with other series in the literature. In the unilateral cases, more involvement is on the right side.
RESULTS In the present study we found 74.46% satisfactory results, unsatisfactory results were noted in 25.54% feet, comparison of the results of clubfoot surgery from different centers is difficult because the preoperative severity of the feet in different studies may be different and no standard means exists for evaluating the residual deformity present after clubfoot surgery. One advantage in using the functional rating scale of Dan Atar et.al.1 is that it allows direct comparison with their results.
Table 9:
Results of our series coincides with the results of comparative study of Dan Atar et. al.1 Our series had good percentages of satisfactory results. This can be explained on the fact that making awareness of parents for the physiotherapy instructions and used orthosis, once they go home. Postoperative Complications
The most common residual deformity noted was forefoot adduction (19.14%), next was varus 4 feet (8.52%), equinus in 2 feet (4.26%),and cavus in 3feet (6.38%). Varus ranging from 3-10 degrees. In residual equinus, pitch of ankle was ranging from 0.5 to 1cm.
REFERENCES
|
|
 Home
Home