Official Journals By StatPerson Publication
|
Table of Content - Volume 7 Issue 2 - August 2018
A comparative, prospective study of proximal femoral nail and dynamic hip screw in the treatment of stable intertrochanteric fractures in adult Indian patients
Anil Kumar DN1*, Gowda B2
1Assistant Professor and 2Professor and HOD, Department of Orthopaedics, Raichur Institute of Medical Sciences, Raichur 584101 INDIA. Email: anildn@gmail.com
Abstract Background: Conservative treatment for intertrochanteric fractures (ITF) have shown higher mortality and have largely been abandoned. Rigid internal fixation and early mobilization is the current standard treatment. Methodology: In this prospective study, we compared efficacy, rate of union, complications, operative risks and functional outcomes in ITF, treated with dynamic hip screw (DHS) and proximal femoral nail (PFN). Results: We included 30 eligible patients (females=19). Fall from the height (n=12) was most common and 53.33% had Boyd and Griffin Type II fracture. Mean radiographic exposure (70 Vs 40) and duration of surgery (100min Vs 80 mins) was greater, but blood loss was less (240mL s 320 mL) with PFN. Failure to achieve closed reduction, fracture of lateral cortex, fracture displacement by nail insertion, failure to put de-rotation screw and drill bit breakage, improper positioning of Richard screw, varus angulation were seen with PFN and DHS, respectively. Stiffness of hip and knee were seen with PFN; occurrence of shortening of >1cm, varus malunion was double with PFN. Mean duration of hospital stay and time for full weight bearing was 26 daysand 12.7 weeks (PFN-10.6weeks, DHS-14.8weeks), respectively. Restriction of hip rotation was more with DHS. Good to excellent results were seen in 81.8% and 63.33%in PFN and DHS, respectively. There were two deaths (myocardial infacrction and liver disorder) in DHS group. Conclusion: PFN is a better alternative to DHS but is technically difficult procedure requiring greater precision and expertise. Proper patient selection and good preoperative planning helps to minimize complications. Key Word: Blood loss, Dynamic Hip Screw, Intertrochanteric fracture, proximal femoral nail
INTRODUCTION Intertronchanteric fractures frequently encountered in elderly patients aged >70 years, but not infrequent in younger population. In younger population, intertrochantereic fracture occurs due to high velocity trauma, where as in elderly population, it is most often due to trivial trauma. Osteoporosis in women make them more prone for this fracture.1 Conservative methods resulted in higher mortality rates and complications such as decubitus ulcer, urinary tract infections, pneumonia, thromboembolic complications. These methods have been abandoned. Due to associated complexities with intertrochanteric fractures and increased mortality of 15-20%.1surgical management is the treatment option; open reduction and internal fixation with implants is the focus in the management. Implants for the fixation of intertrochanteric fractures can broadly be divided into -Extramedullary (ex: Dynamic hip screw) and Intramedullary (ex. Proximal Femoral Nail) devices. Latter is the latest implant for management of intertrochanteric fracture, which is a cephalomedullary device and has many potential advantages such as efficient load transfer, less transfer of the stress and hence, less chance of implant failures; maintenance of controlled impaction, limited sliding due to intramedullary location therefore, less chance of shortening and deformity are other advantages. In addition, shorter operative time, less soft tissue dissection and less blood loss make it a preferred surgical option for orthopedicians.2-5 PFN is a novel, morden, intramedullary implant based on experience with Gamma nail. The currently used Gamma nail as an intramedullary device has high learning curve with technical and mechanical failure rates of about 10%. The AO ASIF in 1996, developed the Proximal Femoral Nail with an antirotation hip pin together with a smaller distal shaft diameter which reduces stress concentration to avoid these failures. PFN has all the advantages of an intramedullary device such as decreasing the moment arm, can be inserted by closed technique which retains the fracture heamatoma, decreases blood loss, minimizes soft tissue dissection and wound infections. Technical ease that can be attained with sufficient training, association with less intra and post operative complications, early weight bearing make it a suitable choice for the treatment of intertrochanteric fractures.6 Moreover, comparative study has shown that sliding of the hip screw and shortening of proximal femur are more common with DHS. In view of these conditions, we compared the results of DHS and PFN in the treatment of intertrochanteric fractures.
MATERIALS AND METHODS This prospective study was conducted by the department of Orthopedics of a tertiary care teaching hospital after obtaining Institutional Ethics Committee’s approval. Determining and comparing efficacy, rate of union, complications, operative risks and functional outcomes in intertrochanteric fractures treated with DHS and PFN were the objectives of the study. Prospective patients were screened after obtaining written informed consent from the patients and included if they met the selection criteria. Patients with fresh intertrochanteric fracture were included while those with pathologic fractures, multiple fractures, fractures in children, old neglected fractures were excluded. After obtaining a detailed medical history, clinical, laboratory and radiological evaluation was carried out on hospitalised patients. Associated injuries were evaluated and treated simultaneously. Trochanteric fractures are classified according to Boyd and Griffinclassification.7 Medical fitness was assessed by the physicians prior to surgery. Patients were randomised into two groups as per the computer generated randomisation schedule based on their clinical status. The patients were operated on elective basis after overcoming the avoidable anaesthetic risks. Figure 1 illustrates the major procedures in the surgery. With appropriate measures femoral nail diameter, length of Richard’s screw, neck shaft angle was measured in unaffected side for femoral nail and dynamic hip screw. A standard length PFN (250mm) femoral nail was used in all our cases. The implant consisted of proximal femoral nail (PFN), self tapping 6.5mm pin, self tapping 8mm femoral neck screw, 4.9mm distal locking screw and an end cap.PFN is made up of either 316L stainless steel or titanium alloy in different sizes. We used the standard length PFN of 250mm with distal diameter of 9, 10, 11 mm. The proximal diameter of the nail was 14mm. Proximal derotation screw of 6.5mm and distal lag screw of 8mm. Distal locking was done with self tapping 4.9mm cortical screws, one in static mode and the other in dynamic mode allowing 5mm dynamization. The nail was universal with 6°of mediolateral valgus angulation and with neck shaft angle of 135°. End cap was not used. We used lag screw of 60-110mm and a side plate that allowed a purchase of at least 8 cortices with shaft of femur and 125-135° angled plate depending upon the neck shaft angle determined preoperatively. A minimum of 4 cortical screws were used to fix the side plate with the shaft.
Figure1: Major procedures in surgery Routine postoperative care was given, antibiotics and analgesics were prescribed as appropriate. Blood transfusion was given depending on the requirement. Patients were ambulated early after 24 hrs following surgery. Quadriceps static exercise and knee mobilization was started in the immediate postoperative period. Patients were taught gait training before discharge from hospital. Only in very unstable fracture pattern weight bearing was not advised. Suture removed on the 10th post operative day. All patients were followed up at an interval of 2 weeks until fracture union, at 12 weeks and at 6 months postoperatively. At each visit, patient was assessed clinically regarding hip and knee function, walking ability, fracture union, deformity and shortening. X ray of the pelvis with both hips was taken to assess fracture union and implant bone interaction.
RESULTS We included 30 eligible patients meeting selection criteria. There were 19 (63.33%) females and 11(36.66%) males. Mean age was 48.6years, with a range of 16-85 years. Patients belonging to 20-60 years comprised 60% of the study population (Table 1).
Table 1: Age distribution
Two patients were known cases of hypertension and diabetes mellitus. One patient each was diagnosed hypertensive during screening and cardiac disease (AR with MS) based on ECG and HOCARDIOGRAM. Fall from the height (n=12) was the most common cause; fall following slip and road traffic accident were the causes of injury in nine patients each. Right side was affected (n=21) compared to left (n=09). Type II fracture was most common (n=16, 53.33%) followed by type I (n=09, 30.0%) and type III (n=05, 16.67%) One patient had ipsilateral pelvic fracture which was managed by external fixation, during fixation of intertrochanteric fracture. No other patient had any other associated injuries. Patients were treated using either DHS or PFN based on the randomization schedule. Demographic characteristics of both groups are tabulated in table 2.
Table 2: Demographic characteristics of two study groups
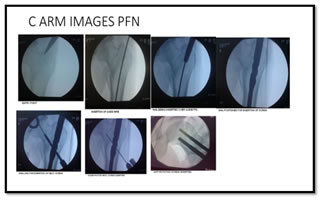
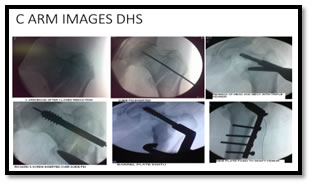
All patients were operated at an average interval of 10.9 days from the day of trauma. Fig 2 and Fig 3 illustrate the C-arm images of PFN and DHS. Figure 2: C-arm images of PFN Figure 3: C-arm images of DHS Intraoperative details are tabulated in table 3.Failure to achieve closed reduction and Improper positioning of Richard screw were the common intraoperative complication in PFN and DHS group, respectively (table 4)
Table 3: Intra-operative details
Table 4: Intra-operative complications
There was one case of post operative infection where open reduction was performed and fracture was fixed with PFN. There was no infection among the DHS patients. Table 5 lists the delayed complications that occurred in our patients.
Table 5: Delayed complications PFN
 Mean hospital stay was 37.87 days, mean time for full weight bearing was 12.7 weeks (table 6). Table 6:
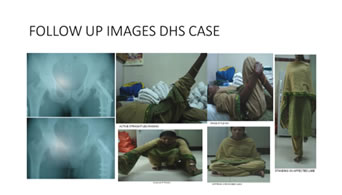
Follow up Five patients were lost for further follow up (3 cases of DHS and 2 PFN) and there were two death in the study due to associated medical problems (myocardial infacrction and liver disorder) in DHS group. Anatomical results were assessed by shortening, hip and knee range of movements and varus deformity. Functional and Anatomical results (table 7) were assessed by taking the remaining 23 cases (PFN-11, DHS-12) into consideration.
Table 7: Anatomical and functional outcome
DISCUSSION Selection of a technique in fracture correction depends on the biomechnics of the fracture, which in turn defines the failure rate and PFN offers biomechanical advantage (better stability and weight bearing) in the intertrochanteric fractures over other available techniques.8-9 Usage of PFN antirotation internal fixation for intertrochanteric fracture is witnessing increased acceptance globally due to its associated advantages such as smaller incision, less time for surgery, less intraoperative blod loss, less volume of drainage, less complicaitons, lesser rate of postoperative fixation failures compared to DHS.10-16 Comparative studies with DHS have proven the efficacy of PFN, supported and recommended its use in intertrochanteric fractures.17-24 Its applicatin for the management of osteoporotic fractures is found to yield better outcomes than DHS.25 Our patients were younger with a mean age of 48.6 years. Men were more affected. Type II was seen in nearly half of the study population (53.33%). Study by Yu W et al17 has shown in their study with longer follow up of 4 years that orthopedic complications are more with DHS than with PFN. In contrast, Calderón A et al26 report better shortcome outcomes with PFN; after that, these benefits are not seen, and are comparable with DHS. Outcomes in pertrochanteric fractures treated with DHS and PFN, clearly demonstrated that PFN allowed faster restoration of post operative walking ability when compared with DHS.27 Recovery was faster and better with PFN compared to DHS allowing early mobilizaiton.21,28 Our reports support these observations; only one patient in PFN remained non-ambulatory. Good functional and anatomical outcomes were seen even during the followup period. Longer surgery time has been reported with DHS.18,22,24,26Jonnes C et al22 reported time of 105min (91 mon for PFN) and blood loss of 159 mL (73 mL with PFN) with DHS. Average time for surgery was less for PFN (51.5±4.4min) compared to DHS (68.8±5.9min); more blood loss was reported with DHS (269.3±40ml) compared to PFN (179±12.9 ml).29 Our study to report less blood loss with PFN, but more operation time (100min Vs 80 min) and more radiological exposure (70 Vs 40) with PFN. Knobe M et al30 report no difference in surgery time but as seen in our study, with radiographic exposure was more in PFN group. However, few studies have reported no significant differences between the two groups.31-32 Bhatti A et al33 reported duration of stay for PFN and DHS in their study was 14 and 22 days, blood loss was 275 and 475ml, persistent hip pain was seen in 3% and 9% respectively. This correlated with our study where the duration of hospital stay was 26 days in both cases, average blood loss was 240 and 320 ml, persistent hip pain was seen in 1/11 and 2/12 cases of PFN and DHS respectively. Nuber S et al24 report a shorter stay with PFN (18.6 days) Use of PFN is not without disadvantages; Imren Y et al8 report increased failure load with this procedure. Evidence indicates that peri-implant fractures though rare but unignorable complication associated with PFN, particularly in females.34 Patient’s age may have a role in the development of this complication as the mean age of participants of the reported study was higher (84.8 years). We observed Failure to achieve closed reduction (23.33%), fracture of lateral cortex (9.99%), fracture displacement by nail insertion (9.99%) and failure to put derotation screw (13.33%) with PFN while DHS was associated with Drill bit breakage (3.33%), improper positioning of Richard(16.66%), and varus angulation (9.99%). There was knee and hip joint stiffness in one patient each in PFN group, and none in DHS group. Shortening of >1cm and Varus malunion were seen in both groups (2 patients –PFN Vs 1 patient –DHS, each). There was no non-union and implant failure in our patients. Zhao C et al29 report that none of their patients had varus collapse with PFN while one had with DHS; lateral hip pain was reported in six patients with PFN. Knobe M et al [30] report complications resulting in re-surgery was more with DHS (25%) compared to PFN; this study also reported high rate of lag screw sliding with DHS. Superficial post operative wound infection is the most commonly reported.[6] Rate of post operative complications have been reported to be similar with PFN and DHS.28 We too noted superficial infection in one patient treated with PFN and was treated with appropriate antibiotic as per the reports of culture and sensitivity. There was no infection in the DHS group. Windolf J et al35 too report the occurrence of local complications requiring revision surgery (4.9%). This study detailed the technical factors responsible for failure and emphasized the precise technical performance; poor reduction and wrong selection of screws were the main factors for the failure, requiring technical precision. Data on procedure related morbidity is limited. Mehboob reports a low intra and post operative morbidity with PFN.36 In our study we had two death due to medical reasons in DHS group. There was no procedure related death. In young patients it was due to high velocity trauma. Fall from height being the common mechanism of injury; slip and fall was common mechanism in elderly. PFN has the advantage of controlled collapse at fracture site, is biomechanically sound and can be done by closed means. In addition, PFN maintains neck length by preventing excess collapse at fracture site. Entry point determination is crucial for PFN, particularly in elderly with osteoporotic bones as wrong entry point may result in iatrogenic comminution of lateral cortex. PFN one implant with many advantages make it surgeon’s choice for intertronchanteric fractures particularly in those with complex fractures.37 Our sample size was small to derive statistical significance and to support or unsupport the use of any of these techniques. We did not objectively test surgeon’s competency in the procedure.
CONCLUSION PFN is a better alternative to DHS in management of intertrochanteric fractures but is technically difficult procedure and requires more expertise compared to DHS. Most of the complications in both PFN and DHS can be avoided with proper patient selection and good preoperative planning.
ACKNOWLEDGEMENT Authors thank the support of the management of the hospital and staff of the department during the conduct of the study. Authors acknowledge the cooperation of patients without which it would have been impossible for them to conduct the study. Authors thank Dr M S Latha for editing support and proof reading.
REFERENCES
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home