Official Journals By StatPerson Publication
|
Table of Content - Volume 7 Issue 2 - August 2018
Failed hip surgeries managed with replacement arthroplasty: A retrospective study of 25 cases
Harsh Raj1, Parag M Tank2*, Vijay J Patel3, Bhargav G Parmar4, Dipak S Parmar5
1Sr. Resident, Department of Orthopaedics, GCS Medical College, Ahmedabad, Gujrat, INDIA. 2Assistant Professor, 3,4PG Resident, Department of Orthopaedics, Smt NHL Municipal Medical College, Ahmedabad, Gujrat, INDIA. 5associate Professor, Shri MP Shah Government Medical College, Jamnagar, Gujrat, INDIA. Email: paragtank1@gmail.com
Abstract Background: Hip fractures account to succumb devastating lifestyle and early mortality in older comorbid patients. Fractures of the hip region need anatomical fixation and osteosynthesis. But implant failures are associated with deformed hip function, biomechanical imbalance of the lumbopelvic synchrony and painful gait. Method: 25 patients operated for hip fractures previously were included in the study. 18 male and 7 female patients between age 30-70 years were the subjects. 18 patients were previously operated fracture neck femur, 5 patients were fracture intertrochanteric and 1 patient had fracture acetabulum. All patients were undergone implant removal and hemiarthroplasty in 6 patients while total hip prosthesis in 19 patients. Assessment were done with Harris hip score at 6 months and 1 year followup. Result: 31% of patients with Ficat Arlet stage II changes were undergone hemiarthroplasty while rest of the patients with grade III-IV changes had operated with total hip replacement. 24% of patients had mild pain at one year followup. 64% of patients had no limitation of walking distance. 92% of patients had no restrictions in daily living activities. Final excellent score was observed in 78% of cases at final follow up. Conclusion: hip arthroplasty following failed hip surgery is a major rescue from morbidity related to complications of immobilisation and altered gait with deranged hip biomechanics. Removal of old implants with reconstruction of hip joint with arthroplasty is an art and require expertise. Key Words: Failed hip, hip arthroplasty, ficat arlet stage, harris hip score.
It is still controversial to recognise the ideal management plan and implant of choice for elderly hip fractures. As with the frequent occurrence of intertrochanteric fractures than neck of femur fractures in old age people, low socioeconomic status, unhealthy diet, already existing osteoporosis and comminuted fractures jeopardise the healing rate and fail primary surgery.1 With the advent of technological leap, reliable and trustworthy instrumented techniques designed to total hip arthroplasties render accepted outcomes of health related quality of life.2 Preoperative education and counselling have improved the scenario of current widespread acquaintance of hip arthroplasty by both primary as well as secondary or revision subjects.3 Osteosynthesis in fracture in and around hip joint is the mainstay of treatment possibly in all age group. Following failure of primary fixation owing to magnitude of injury to vulnerable porotic bone, unstable fracture pattern, wrong implant selection and method, hip replacement is a expected and adequate salvage procedure regardless of operative challenge.4 Screws, sliding hip screws, dynamic hip screws and lately proximal femoral nails of all generations have propensity to cut out, penetrate or breakage of itself tend to failure of fixation with complications. With an attempt to revise in younger age group again with same or different implant due consideration of femoral head salvage but in older age group hip replacement has promising results with early ambulation.5 We studied clinical and functional outcome of patients with previously treated with different implants for fracture neck of femur, intertrochanteric fractures and acetabular surgeries revised for failure of various reasons with hip arthroplasty for short term followup.
MATERIALS AND METHOD We studied retrospectively 25 patients of previously failed hip surgeries operated at our institute and other setup before January 2012. 6 patients were undergone hip hemi arthroplasty and 19 patients were undergone total hip surgery. All patients demographic data with etiology of failed primary surgery, comorbidities are recorded. Thorough history with clinical examinations are undertaken. All patients are counselled for hip arthroplasty with due understanding of indication, nature of daily function performed after surgery and problems related with hip arthroplasty. Following instituitional ethical board review patients are included in the study. Preoperative anaesthetic and surgical consents are taken. All patients are given spinal anaesthesia. Inclusion Criteria
Exclusion Criteria
All surgeries are done with operating surgeons who are authors of the study. patients are positioned floppy lateral position. Same previous incisions are demarcated and utilised in southern postrior approach of the affected hip. Hypertrophied Scar tissue of the previous incisions are excised. Intact cancellous screws are removed from lateral aspect of proximal femur easily while broken screws are removed with excision and morcelisation of head. Sliding hip screws are removed with difficulty leaving bony defects on posterolateral aspect of proximal femur. Proximal femoral nails are removed but proximal broken screws are removed same as cancellous screws. Acetabular plates are removed in one case. No trochanteric osteotomy done in any of the cases. Head delivered with deliberate care and preserve in all cases for bone grafting at acetabular defects. Proximal femur broached meticulously and young patients undergone uncemented total hip components while older patients had operated with hybrid if no bone loss and both cemented with bone grafts if acetabular bone loss visualised. six patients with comparatively good acetabulum are implanted with modular bipolar hemiarthroplasty. Greater trochanter encirclage wiring for trochanteric reconstruction are performed in cases of stuck old implants which jeopardise the weak horizontal offset and fulcrum imbalance. Acetabulum are inspected in every cases for bone loss, marginal erosions, labral pathology and osteophytes. Some acetabular bone defects are observed inn cases where previous implants were penetrated the femoral head and scratched the articular cartilage of pulvinar or medial weight bearing dome roof arc. Cancellous bone grafts from posterior superior iliac region harvested and weight bearing dome reconsruction done followed by reaming of the cavity initiated. Edges of the labrocapsular margins were freshened and fibrosed, devitalised tissues excised. Total hip prosthesis are usually CoCr alloy without dual mobility cup and highly cross linked polyethylene liner are used. Cup of respective sizes were implanted depending upon the head size of the patient. In case deformed head or if head was not available on table for measurement true size caliberation of the opposite hips were also taken preoperatively. In all cases femur first implantations were instituted as femoral bone loss were more due to previous implants. Along with adequate version of the acetabulum and femur following on table reduction of the hip joint length of the limb checked compared to other normal limb. Wound closed in layers keeping negative suction drainage. Skin closed with stapler. Surgiwear dressing applied. Limbs are kept apart in the postoperative period. Postoperatively patients were given blood transfusion if required. Dressings were changed on second day with removal of suction drain. Diabetic patients were switched over insulin sliding scale regimen. Broad spectrum antibiotics were administered. Patients were allowed to stand on third to seventh day as physiotherapy protocol with quadriceps and hamstrings exercises. No patients were given oral or subcutaneous anticoagulants except one preexisting ischaemic heart disease patient who was allowed to continue aspirin as preoperative regime. X-rays were taken on third day. Regular rehabilitation protocol followed and patients were called for visit at 2 weeks, 4 weeks, 6 weeks, 8 weeks, 12 weeks, 6 months and at one year. Harris hip score were taken after 6 months and at end of a year. Patients were followed up for 5 years. Each time clinical and radiological examination and scores were recorded and compared with subsequent visits. RESULTS Table 1: Data evaluation for our study
Table 2: Harris hip score evaluation
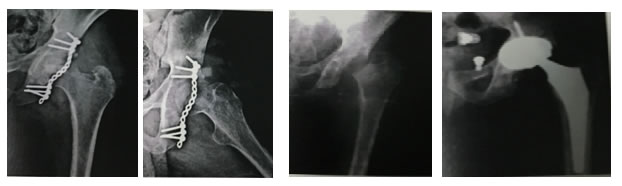
Figure 1.1 Figure 1.2 Figure 1.3 Figure 1.4 Figure 1.1: Primary surgery for acetabulum fracture; Figure 1.2: Implant removal surgery after index surgery; Figure 1.3: Secondary surgery with THR; Figure 1.4: Rom at hip at final follow up
We observed 25 patients of failed primary surgery of hip from January 2012 to June 2015. 18 male patients (72%) and 7 female patients (28%) of previous surgery on hip included. Age of the patients were from 30years to 70 years with mean age 51.56 years observed. 15 patients (60%) were operated for final surgery on left side while 10 patients (40%) of previous hip surgery were affected on right limb. 18 patients (72%) of previously operated for neck of femur fracture, 5 patients (20%) of failed intertrochanteric fracture surgery and 2 patients(8%) with previous acetabular fracture surgery were observed. 18 patients(94%) of previously operated for neck of femur fractures were operated with cannulated cancellous screws, while 1 patient(5.2%) was operated with sliding hip screw. 3 patients (75%) of fracture intertrochanteric region was operated with proximal femoral nail and 1 patient (25%) was operated with sliding hip screw with derotation screw. Two patients were operated with plate and screws for posterior wall acetabulum fractures. 6 patients (31%) of previously operated fracture neck of femur were revised with second surgery with modular bipolar hemiarthroplasty. One patient had cancellous screw cutout with grade IIIA avascular necrosis of femoral head observed. Five patients with grade IV AVN changes with one patient operated with sliding hip screw had screw penetration in acetabulum with pain and positive trendlenburg test. One patient with non-union and breakage of cancellous screw with grade IV avascular changes was revised with total hip prosthesis. 12 patients (92.3%) had grade IV avasular canges in hip operated previously with cancellous screws were finally operated with total hip implant. 3 patients (75%) operated before with proximal femoral nail for intertrochanteric fractures had proximal screw cutout in one patients while two patients had proximal screw acetabular penetration with grade IV avascular changes while one patient operated with sliding screw had varus collapse with neck shorten and absorbed operated finally with total hip prosthesis. 2 patients operated previously for posterior fracture acetabulum wall had grade IV avascular changes operated with total hip prosthesis with bone graft harvested from posterior iliac bone. We reported 2 cases of bipolar and 1 case operated with total hip prosthesis had infection which were managed with vigorous antibiotic prophylaxis for 3 weeks. We had one case each with bipolar and total hip prosthesis encountered with dislocation postopratively which were managed with close reduction. Sciatic nerve palsy was observed in one patient of acetabulum fracture operated with much difficulty for total hip replacement with bone graft which showed partial regeneration of tibial and peroneal fibres at two year of followup of clinical and nerve conduction study. We observed 76% of patients had no pain in either of the previous surgery operated with arthroplasty while 24% of patients had mild pain at one year followup. 64% of patients had no limitation of walking distance at final followup while 24% of cases had decreased walking distance. 12% of cases had significant limitation of walking distance especially comorbidities and complication like infection. 92% of patients had no difficulty in executing activities of daily living while 12% of cases had some difficulty in daily activities. Harris hip score was excellent in 78.94% cases of previously fracture neck of femur while 75% of fracture IT treated with arthroplasty. 21.05% of fracture neck of femur and 25% of fracture IT had good result. No patients in our series was revised for hip replacement in 2 year of final follow up.
DISCUSSION Following primary surgery the next surgery remain always difficult in all age groups and all fractures for patients as well as for expert surgeon. Proximal femur and hip joint have tremendous biomechanical and locomotor implications in trunk balance and gait functions. In second surgery of hip utmost care must be taken while removing old implants especially broken and sunk inside bone. In order to avoid further bone damage and loss preoperative planning of autograft or allograft should be considered for reconstruction of the acetabulum.6 Intertrochanteric fractures have considerable more bone loss after primary fixation failure due to medialisation of femoral shaft and severe collapse of proximal fragment with greater trochanter increased horizontal offset. Simultaneous wasting of gluteus muscles with abduction weakness yield rehabilitation following hip arthroplasty longer and difficult. Risk of osteosynthesis for neck of femur bound to fail particularly in old age. But primary hip arthroplasty and following failure of osteosynthesis hip arthroplasty have similar results. Internal fixation for neck of femur should be the primary procedure.7 Nilsson et al8 reported 11% dislocation rate in secondary arthroplasty following primary failed osteosynthesis for neck of femur fracture and advocated elective secondary hip arthroplasty should be instituted early for successful outcome. As far as possible in salvage hip arthroplasty following initial failed hip surgery is to maximally preserve functional consistency of abductor mechanism during surgery and reconstruction if required. Vigorous weight bearing rehabilitation programme should be started within a short period amount to contribute to excellent result.9 However majority of the cases of fracture neck femur especially young age group are treated primarily by osteosynthesis as the basic concept is to preserve the native biomechanics of the joint, they must be counselled about failure of this method and need hip arthroplasty as second revision surgery. Moreover patients are counselled the inadequate and inferior performance at the end of revision rather than primary arthroplasty.10 In older age group with multiple comorbidities early and rapid mobilisation of the extremities as well as weight bearing walking should be initiated to curb the secondary complications of immobilisation and to increase longevity of life. With calcar replacing implants and long stem implants it is possible to primarily replace the hip in comminuted intertrochanteric fractures keeping in mind major surgery and cement related problems in already compromised cardiorespiratory compensation in old age.11 Proper placement of total hip component considering the bone loss and adductor fulcrum preservation the chances of dislocation following total hip arthroplasty are lesser to hemiarthroplasty. 12 In the outset of femoral fracture non-union treated with implants which fail subsequently total hip arthroplasty confer promising and satisfactory outcome. The problems related to revision arthroplasty like dislocation and aseptic loosening are almost always part and parcel of this method which is unavoidable.13 Better understanding and improved state of the art techniques of hemi and total hip arthroplasty share a confident task between superior success and lesser failure. Novel research for better and better designs of implants of joints also show possibility of longer life of the joint and press fit configurations of the same too render satisfactory outcome in already failed bones. Nevertheless, age and bone quality following multiple surgery would decrease chances of gaining extraordinary result to the bottom. Still expertise of the surgeons and researchers are boon to the disease conquering the unfavourable failure of the natural mechanics.
CONCLUSION There is high rate of failure of primary fracture neck of femur in young age which necessitate early definitive intervention. Secondary hip arthroplasty in these age offer vaid results. Failed implants in intertrochanteric fracture of the proximal femur can be revised with hemi or total hip arthroplasty with excellent to good outcomes. Fracture acetabulum is always not left without arthritis and femoral head avascular necrosis which demand total hip prosthesis a revolution of technology and moreover render functional painfree activity of daily living in patients.
REFERENCES
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home