Official Journals By StatPerson Publication
|
Table of Content - Volume 7 Issue 3 - September 2018
Study of proximal femoral nail v/s dynamic hip screw in inter-trochantric fractures treated at Pravara Rural Hospital, Loni, Maharashtra, India
Dinesh Dhaytadak1, Sanjay Mulay2*
1Sr. Resident, Department of Orthopaedics, Rural Medical College, Loni, Dist Ahmadnagar, Maharashtra, INDIA. 2Professor, Department of Orthopaedics, Bharati Vidyapeeth Medical College, Pune, Maharashtra, INDIA. Email: sanjaymulay59@gmail.com
Abstract Background: This is the commonest injury seen in patients above 50 yrs of age, with more incidences in women. Multiple factors like aging, osteoporosis, anatomy of inter trochatric region, predispose to this type of injury. Many techniques were tried since 19th century, but only Dynamic Hip Screw (DHS) and Proximal Femoral Nail (PFN) have survived over so many years, and have been accepted by the surgeons and still today, these 2 modalities remain to be the treatment of choice in inter-trochantric fractures. Methods: A comparative study was carried out in sample size of 50 patients, wherein 25 patients were treated with DHS and other 25 treated with PFN during the period of September 2015 to September 2017 in Department of Orthopaedics, Rural Medical College, Loni, Maharashtra. Isolated intertochantric fractures with recent history, both stable and unstable were included in this study, while pathological fractures, paediatric fractures, polytrauma were excluded from this study. Results: Both the techniques were compared on various parameters like pain, fracture union, implant cut out, failure of implants, operative blood loss, duration of surgery, high risk cases, early weight bearing. On all these counts, this study revealed that although the difference was marginal, PFN was better technique over DHS especially in unstable fractures. Healing of fracture and weight bearing was found to be earlier with PFN than with DHS. Since the fracture hematoma is not opened in PFN, it allows biological healing of fracture. Conclusion: It was found that PFN is stronger construct to withstand cyclical loading and unloading in trochantric region. PFN was found to be better in high risk cases. Key Words: Dynamic Hip Screw (DHS), Proximal Femoral Nail (PFN), Inter-trochantric fractures.
Inter trochanteric fractures are those occurring in the region extending from the extracapsular basilar neck region to the region along the lesser trochanter. Due to an increasing life span and sedentary lifestyle, the incidence of these fractures is increasing. Also the osteoporosis in geriatric age group has contributed to higher incidence of this injury. With low energy falls like miss-step can also cause this injury. Approximately in 90% of the community which is more than 50 years of age, with a higher proportion in women, the inter-trochantric fractures are seen. High velocity trauma resulting in inter-trochanteric fractures are relatively rare and are more common in men less than 40 years of age.1 Cummings SR et al2 noted that neither age related osteoporosis, nor the increasing incidence of falls with age sufficiently explains the exponential increase in the incidence of hip fracture with aging. Their hypothesis was that four conditions correlated for a fall to cause a hip fracture a) Direct impact on hip, b) Failure of protective responses, c) Local soft tissues cannot absorb the energy to prevent impact, and d) Residual energy of the fall exceeds the strength of proximal femur. This concept applies primarily to strategies to prevent hip fractures. The inter trochantric fractures are basically divided into 2 types, stable and unstable fractures. This is decided by the degree of comminution especially in posterior and medial aspect of trochanteric region, displacement with altered neck-shaft angle (coxa vara), and the rotational displacement. In order to analyze these things, the detailed study of the fracture geometry was essential. Many techniques were tried from intramedullary devices to nail plate assembly over years. But, with improved knowledge of biomechanics and the transfer of forces during weight bearing, the evolution in implant design took place, and in 1956, the first commercially available sliding compression hip screw was made available in United States in cooperation with K. Clawson of Seattle and McKenzie of Scotland manufactured by Richards Manufacturing Company of Memphis, Tennesse.3 The DHS is a unique implant which facilitates application of compression across the fracture line at the time of surgery; it also acts as a rail on which controlled collapse occurs at the fracture site. Weight bearing causes the femoral head to become impacted on the femoral neck producing dynamic compression of the fracture. The shaft of the lag screw slides down the barrel maintaining reduction of the fracture as compression occurs.4-7 The AO ASIF,8 developed the proximal femoral nail (PFN) with an anti rotation hip pin together with a smaller distal shaft diameter which reduces stress concentration to avoid failures. The mechanism of action of PFN is similar to that of DHS i.e. controlled collapse at the fracture site on weight bearing leading to compression at the fracture. Here the intra-medullary nail replaces the side plate of the DHS. The distal screws lock the nail and help in control of rotation and telescoping of the fracture fragments. A PFN has a mechanical advantage over the DHS of reducing the distance between the weight bearing axis and the implant. The lag screw withstands the bending movement which is transferred to the intramedullary nail and counterbalanced by its locking mechanism with the femoral cortex in the medullary canal. Almost the entire load is transferred to the nail and negligible portion to the femoral cortex while on the other hand; the DHS transfers a large proportion of its load to the medial femoral cortex.9-11 The tip-apex distance is another factor which plays an important role in biomechanics of DHS. It is the sum of the distances from the apex of the femoral head to the tip of the lag screw on anteroposterior and lateral radiographs. If it is less than 25 mm, then there are very less chances of failure by cutting out of the lag screw.12
MATERIAL AND METHODS Study design and Sudy period: A prospective study carried out between September 2015 to September 2017 in Department of Orthopaedics, Pravara Rural Hospital of Rural Medical College, Loni, District- Ahmednagar, Maharashtra, India Study Tool: The DHS implant consists of a lag screw, a compression screw and a barrel attached to a side plate. Compression Screw used allows compression of 36 mm at the fracture site. Barrel side plate are available in angles of 125,130, 135, 140 degrees and from 4 -12 holes. 135 and 140 degree plate is more often used. 4.5mm cortical screws are used to fix the side plate with shaft. The implant consists of a Proximal Femoral Nail, a self tapping derotation 6.5mm screw, a self tapping 8mm femoral neck lag screw, 4.9mm distal locking screws and an end cap. PFN is made up of either 316L stainless steel or titanium alloy. PFN Length: Standard PFN: 250 mm. Long: 340, 360, 380, 400, 420 mm Diameter: 9, 10, 11, 12 mm, Neck shaft angle range: 130°, 135° The nail is having 14 mm proximal diameter. This increases the stability of the implant. There is 6° mediolateral valgus angle which prevents varus collapse of fracture, even when there is medial comminution. The distal diameter is tapered to 9-12 mm, which also has groove to prevent stress concentration at the end of the nail and avoids fracture of the shaft distal to the nail. Proximally it has two holes, for insertion of 8mm neck screw which acts as a sliding screw and the proximal one is for 6.5mm hip screw which helps to prevent the rotation. Distally the nail has two holes for insertion of 4.9mm locking screws. Sample Size: Total 50 patients (25 - DHS and 25 – PFN) Inclusion Criteria
Exclusion Criteria
RESULTS The study comprised of 50 patients as per the inclusion criteria and two groups were made, one operated with DHS while other operated with PFN with 25 patients in each group. Of the 50 patients there were 20 females and 30 males. The youngest patient in our series was 20 years and the oldest was 89 years. The average age of the patient for DHS was 62 years and for PFN was 60 years. The average surgical time for DHS was 94.44 minutes (range 50-150 min) and for PFN was 64.52 min (range 40-125 min). Surgical time needed for PFN was less than for DHS (p=0.001). The average intra operative blood loss for DHS was 227.96 ml (range 120-640 ml) and 9 patients needed blood transfusion. The average intra operative blood loss for PFN was 87.28 ml (range 40-125 ml) and only 2 patients needed blood transfusion. Blood loss in PFN surgery was less as compared to DHS surgery (p= 0.001). Out of the 50 patients, 2 expired during follow up due to unrelated causes (both due to myocardial infarction) and 4 patients were lost in follow up. The remaining 44 patients were followed up for an average of 12 months. Table 1: Distribution according mode of injury (n=50)
As Table 1 showing distribution of the cases with fall from height, Road traffic accidents, and slip and fall. The numbers of cases are more in category of slip and fall, than other modes of injuries.
Table 2: Distribution according to co-morbidities
It was seen from Table 2 that the associated medical co-morbidities, which have direct impact on surgical outcome. These fractures are seen after 5th/6th decades. Hence medical co-moorbidites like Bronchial Asthama (BA), Hypertension (HTN), Diabetes mellitus (DM), chronic renal failure, are seen.
Table 3: Distribution according to Follow up (Harri’s Hip Score at 3 Months)
It was observed from Table 3 that Harris hip score used in this study has following parameters. At the end of 3 months, in DHS group, 2 patients were graded as excellent, 9 patients as good, 4 patients as fair, 5 patients as poor, 1 with failed result, 3 patients were lost in follow up and one patient died. In the PFN group, 3 patients were graded excellent, 9 patients as good, 8 patients as fair, 2 patients as poor, one was lost in follow up and one patient died.
Table 4: Distribution according to Follow up (Harri’s Hip Score at 1 Year)
It was seen from Table 4 that at 1 year follow up, in DHS group, 6 patients were graded as excellent, 6 patients as good, 6 as fair, 2 as poor and 1 as failed. 3 patients were lost in follow up and one patient had died. At 1 year follow up in PFN group, 5 patients were graded as excellent, 9 patients as good, 8 as fair and 1 as poor. 1 patient was lost in follow up and one patient had died. Aaverage Harris Hip Score for PFN was much better than DHS in the early follow up but later on the difference reduced between the two modalities of treatment. Thus PFN provides an early mobilization and rehabilitation of the patients as compared to DHS. The functional outcome (Harris Hip Score) was better in PFN group than DHS group for unstable fractures but was not significant.
Table 5: Distribution according to Gait after one year
It was seen from Table 5 that the average rate of fracture union in PFN group was 10.52 weeks (range 6 to 36 weeks) and in DHS group was 13.84 weeks (range 6 to 24 weeks). 1 patient of DHS group developed a superficial infection which settled down with 2 weeks of intravenous antibiotics. Another patient developed a deep infection which required a debridement procedure at 2 weeks followed by a 2 weeks course of intravenous antibiotics after which the infection subsided. 1 patient in the DHS group developed excessive shortening (>2.5 cm) during the follow up due to increased collapse at the fracture site. 1 patient in the DHS group developed a bed sore; the patient was household ambulatory pre operatively and was bed ridden post operatively for some time due to medical reasons. 1 patient in DHS group had an implant failure due to the cut out of the DHS screw, the patient was later on treated by implant removal and hemiarthroplasty. 1 patient in PFN the group developed non union which was treated by bone grafting at 6 months post surgery and later followed up with signs of fracture union.
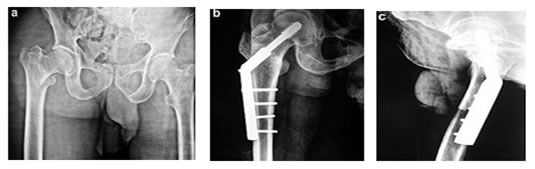
Figure 1: DHS (Dynamic Hip Screw)
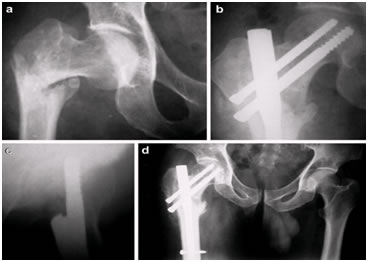
Figure 2: PFN (Proximal Femoral Nail)
DISCUSSION The treatment of intertrochanteric fracture is still associated with some failures. High stress concentration subjected to multiple deforming forces and high incidence of complications reported after surgical treatment, compels the surgeon to give a second thought regarding selection of proper implant. Many designs have come and got discarded. It is only DHS and now PFN has survived so far. Bridle SH et al12 and Leung KS et al13 compared the results of Gamma nail with a sliding hip screw in a prospective randomized controlled trial and observed that Gamma nail required lesser time with lesser intraoperative blood loss than sliding hip screw. There was no significant difference in the final clinical outcome. They also stated that patients of Gamma nailing could achieve full weight bearing in a significantly shorter time. In our study we also noted that the time required for surgery and the intraoperative blood loss was less in P.F.N. as compared to D.H.S. and the patients mobilization was quicker in P.F.N. than in D.H.S. group. Menezes DF et al14 conducted a study on 155 cases of intertrochanteric fractures treated with P.F.N., and found 2% failure of fixation. However no such failure of fixation was noted in our study. Another study by Pajarmen J et al15 showed that the blood loss in D.H.S. group was more than in P.F.N group though the surgical time required for D.H.S. was less as compared to P.F.N. Also the P.F.N. accounted for a significantly better mobilization as compared to D.H.S. in the early stages of post operative follow up. In our study the time required for P.F.N. was significantly less than for D.H.S. but the blood loss and mobilization parameters correlated with the above mentioned study. Thus in stable fractures the functional outcome for both the modalities of treatment was similar. But in unstable fractures, the functional outcome was better for PFN than for DHS however, (p >0.05). At 1 year follow up, 9 patients had no pain, 5 had minimal pain, 6 had moderate pain and only 1 patient had severe pain post operatively in the DHS group, while 12 patients had no pain, 8 had minimal pain and 3 had moderate pain post operatively in the PFN group. Thus, though the number of patients with none or minimal post operative pain was more in the PFN group (20) than the DHS group (14), the difference was not statistically significant (p>0.05). Also at 1 year follow up, 10 patients had a normal gait, 3 patients had a limp, 3 patients used a stick for walking, 4 patients used a walker and one patient used a wheel chair in the DHS group while 12 patients had a normal gait, 5 patients had a limp, 4 patients used a stick while walking and 2 patients used a walker for walking in the PFN group. There was no significant difference between the number of patients with a normal gait (10 and 12 respectively) in the DHS and the PFN group (p >0.05).
CONCLUSION The functional outcome of both DHS and PFN are mentioned earlier which reveal that PFN is better in unstable fractures, is stronger construct to withstand cyclical loading and unloading, and provides medial buttress effect to prevent excessive collapse and shortening of neck. It is useful in high risk cases with less surgical exposure and less blood loss, polytrauma and with other medical co-morbities. Moreover in PFN fracture hematoma is preserved. DHS has more exposure, more soft tissue dissection, more surgical time and more blood loss. Failure of fixation is seen in both techniques due osteoporosis and poor purchase of implant.
REFERENCES
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home