Official Journals By StatPerson Publication
|
Table of Content - Volume 8 Issue 1 - October 2018
Study of bone mineral density to predict osteoporosis in Indian population
C Ravi1*, Kalwa Dinesh2
1Associate Professor, Department of Orthopedics, Mahavir institute of Medical Sciences, Vikarabad, Telangana, INDIA. 2Registrar, Apollo DRDO, Hyderabad, INDIA. Email: ravihyd9@yahoo.com
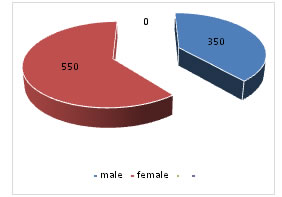
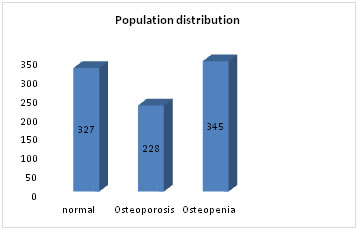
Abstract Background: Osteoporosis is the most frequent problems leading to or aggravating orthopaedic problems. Calcaneal quantitative ultrasound is frequently used method with ease of access and usage that can provide information about osteoporosis. The aims of this study are to identify efficacy of detecting underdiagnosed osteoporosisand finding out prevalence of osteoporosis. Despite osteoporosis related fractures be a major health issue, osteoporosis remains underdiagnosed. Objective: To determine the prevalence of osteoporosis by bone mineral density in general population. Subjects: Patients who visited to outpatient departments in Hyderabad and vikarabad have been included in the study after taking informed consent. Methods: This study was conducted in patients attending the outpatient departments of hyderabad and vikarabad during 2016to 2018.The assessment of osteoporosis diagnostic accuracy was performed for calcaneal quantitative ultrasound. Results: We enrolled 900patients out of which 350 are male patients, 550 are female patientsand almost 25%(228) of them had osteoporosis, and osteopenia in 38% (345) with most number of patients with osteopenia and osteoporosis were present in 51-60years age group. Conclusions: Use of calcaneal quantitative ultrasound for screening is a reasonable alternative of dual-energy X-ray absorptiometry. since many studies confirm that none strategy is clearly superior, but various available tools must be always completed with X-ray. Key Words: Osteoporosis; Calcaneal ultrasound, dual-energy X-ray absorptiometry.
INTRODUCTION Osteoporosis is a skeletal disorder characterized by compromised bone strength, which predisposes an affected individual to bone fracture1. Osteoporosis leading to fractures after minimal traumais a considerable problem in health care because of its potentially severe consequences for both the patient and the health care system if a fracture occurs, particularly in elderly patients with co-morbidities. Estimates of the prevalence of osteoporosis vary with the specific definition chosen, but the World Health organization has estimated that 30% of all women aged over 50 (postmenopausal) have osteoporosis according to a definition of bone mineral density being more than 2.5 standard deviations below the mean for young healthy adult women at any site.3 Hip fractures are the most serious result of osteoporosis, and incidence is increasing more than would be expected from demographic changes in age and sex ratio. It is important to find ways of preventing osteoporotic fractures. Measuring bone mineral density has been used as for early identification of individuals at high risk of a fracture, although it is only one of the risk factors for fracture. The World Health Organization (WHO) has established criteria for the diagnosis of osteoporosis, criteria that rely on a patient’s T-score, gleaned from DXA based BMD measurement at the hip or spine.3The standard deviation (SD) was expressed as T‑score. It was calculated as a difference between the measured bone mineral density (BMD) of the patients and the expected bone density value in a normal young person (YN) divided by the population standard deviation (SD)20 T-score=BMD-YN/SD21 A patient’s bone mineral density (BMD), measured by DXA, is expressed in g/cm2; however, by convention, the score then is converted to a T-score, which represents the number of standard deviations (SDs), plus or minus, from a reference value2 Calcaneal ultrasound measurement (quantitative ultrasound, QUS) has been shown to predict fractures in elderly women. However, only a few studies have examined its ability to predict perimenopausal and early postmenopausal fractures4. According to the World Health Organization (WHO) criteria the diagnosis of osteoporosis is based on bone mineral density (BMD) 2.5 standard deviation (SD) or more below the young adult mean (a T-score < 2.5 SD).3 A T-score within the normal range is −1.0 SD or above, while a T-score between −1.0 and −2.5 SD characterizes low bone mass, referred to as osteopenia. The pathogenesis of bone reabsorption is multifactorial. There are general factors that predispose to osteoporosis-such as age, gender, malnutrition, sedentary lifestyle, alcohol, hypogonadism, glucocorticoid, and obesity etc. Studies have shown that patients with HIV-infection have an increased risk for fracture compared to non-HIV infected patients. Patients have an increased risk of fractures due to osteoporosis. Considering that bone strength reflects integration of bone density and bone quality, these findings suggest that bone quality may be as important as bone density. DXA provides information on mineralization status but not on bone quality. Quantitative ultrasound (QUS) method can integrate this information. Laboratory investigations have indeed demonstrated that QUS measurements of excised bone specimens are influenced by material properties and structural bone characteristics. In addition, ultrasound velocity has been used extensively to characterize the elastic properties of trabecular and cortical bone.5 The aim of this study was to investigate the population at risk of osteoporosis, according with theguidelines for osteoporosis, measuring the BMD by calcaneal quantitative ultrasound (QUS). MATERIALS AND METHODS Methods: This cross-sectional study was conducted at the out patient departments of Hyderabad and Vikarabad during 2016and 2017.Inclusion Criteria: Patients aged above 40 years. Both male and female are included Exclusion Criteria: Previous osteoporosis diagnosis, previous fractures, previous treatment for osteoporosis. The ultrasound scanning of calcaneus of the left foot was performed with Hologic Sahara device. QUS is used to obtain an estimate of the heel BMD in g/cm2.
RESULTS We found no association between the relative risk for decrease in bone density of 1 SD and the length of follow up. Relative risk of fracture for 1 SD decrease in bone density compared with relative risks in women for stroke and coronary heart disease. Table shows age distribution
Table 1:
Figure 1: Representing sex distribution
Figure 2: . DISCUSSION The study population consisted of 900 patients aged 51-60 years, most of them were female. The number of patients classified as “osteoporotic” varied according to the method of measurement used and site evaluated. Almost 25% of patients were diagnosed as osteoporotic. In contrast, no statistically significant differences were found for the following variables: gender, BMI, cigarette smoking, diabetes mellitus, hypophosphatemia, or hyperparathyroidism. Interestingly, among patients with normal bone measurements (T-score > −1.0 SD), osteoporotic vertebral fractures were found. Odds ratio expresses the risk of VF in patients with normal BMD, osteopenia or osteoporosis, according to femoral, lumbar, and calcaneal T-score. Ability of Bone Density Measurements To Predict Fractures whether bone density has theability to predict fractures at all ages. In a paper published by Nevitt 13et al showed that bone mineral density could predict fractures equally well over a three year period up to the age of 80: “Thus it seems that an old age bone mineral density can predict fracture, at least for a 3-year-period. There are few studies in men, but the predictive ability of bone density measurements seems to be similar for men and women. Use of Screening: Bone density measurements can predict risk of fracture. Although, there are no obvious cut off values for screening. Law14 et al made a similar analysis of case-control studies of hip fracture and found alower predictive ability for measurements of bone density (odds ratios of 1.35 for all measurement sites and 1.7 for measurement at the femoral neck). They calculated a detection rate of 30% and a false positive rate of 15% for measuring bone density at the femoral neck as a screening tool, based on a cut off 1 SD below the mean density of the controls. Even though bone density can predict fractures in a similar way as blood pressure for stroke, we cannot recommend a screening programme for osteoporosis by measuring bone density15. There is a overlap in the bone densities of patients who develop a fracture and who dont. Thus, bone mineral density can identify people who are at increased risk of developing a fracture, but cannot identify individuals who are for sure going to develop a fracture. Osteoporosis is a complex, multifactorial chronic disease that may progress silently for decades until characteristic fractures result late in life. Because there are no symptoms until fractures occur, relatively few people are diagnosed in time for effective therapy to be administered.16 In young adults, the two processes are closely coupled: Bone resorption is matched by bone formation, and bone mass increases or at least remains constant. With aging, however, bone formation does not keep pace with resorption, and bone mass is gradually lost throughout the skeleton.16 The biomechanical effects of age-related bone loss are partially compensated for by modeling of the shafts of long bones (through endosteal resorption and periosteal apposition) to increase the diameter and, thus, increase resistance to bending and torsion. However, this process is less marked at the ends of limb bones and in the vertebrae, where fractures typically associated with osteoporosis occur.17 The application of FRAX score is very useful for the assessment of fracture risk, because this tool gives the 10-year probability of a major osteoporotic fracture and it can guide decisions about who to screen.5
Table 1:
*Rheumatoid arthritis type I diabetes, hypertbroidum hypogedism, gastro-intestinal disease, chronic liver disease, pulmonary disease, organ transplantation.
WHO defines osteoporosis based upon DXA measurements.1 In fact, this method remains the most widely used for measuring BMD and T-score based on DXA measurements are the only validated for osteoporosis/osteopenia diagnosis. DXA provides accurate measurements at clinically relevant sites, i.e. those with major clinical consequences in case of a fracture; on the other hand, the major disadvantages of DXA are non-portability (large machine), relatively expensive compared to other technologies (especially if performed in low-income countries), and the use low-dose radiation.6,7 Alternative techniques for evaluation of bone status at peripheral sites have been developed. Among them quantitative ultrasound measurement of the heel is considered one of the best alternative method currently available for the assessment of fracture risk.8,9 An advantage of this technique is the possibility of detecting structural bone characteristics (elastic properties, trabecular orientation) thus enabling a better quantification of bone quality. It is portable, cheaper, and easier to perform in comparison with DXA. The limitation of our study was the small size of the patients included. Further studies are needed to analyze the potential of this technique. For patients with limited access to DXA or those who prefer not to travel for DXA screening, using QUS for screening is a reasonable alternative. Screening should always be followed by X-ray. Treatment of postmenopausal osteoporosis with parathyroid hormone (1-34) decreases the risk of vertebral and nonvertebral fractures; increases vertebral, femoral, and total-body bone mineral density; and is well tolerated.18 The overall relation with BMD and fracture risk was similar in men and women. Specifically, fractures of the hip and wrist were strongly associated with low BMD, in both men and women, while for upper humerus fractures, this was only significant in women.19 There are four different ways in which a BMD assessment technology can be used. It should i) help in the diagnosis of osteoporosis, ii) be able to detect changes in BMD with time or after any therapeutic intervention, iii) be able to predict occurrence of fragility fractures in a patient, and iv) be able to discriminate between patients with and without previous fragility fractures.22
REFERENCES
|
|
 Home
Home