|
Table of Content - Volume 8 Issue 2 - November 2018
Functional outcome of open fractures of tibia treated with reamed interlocking intramedullary nailing
Basavlingappa Choudhari1*, Shiva Shankar T H2, Niranjan M3, Alexander Thomas4
1Assistant Professor, Department of Orthopedics, Al-Ameen Medical College, Bijapur, Karnataka, INDIA.
2SDM Hospital, Ujire, Belthangady, DK, Karnataka, INDIA.
2HOD, Department of Orthopedics, 3Sr. Orthopaedic Consultant and CEO, Bangalore Baptist Hospital, Bangalore, INDIA.
Email: dranandmdfm@gmail.com, drbasavarajc@yahoo.in
Abstract Back ground and Objectives: Tibial diaphyseal fractures common long bone fractures encountered in clinical orthopaedic practice. Because most of the length of tibia is subcutaneous throughout, open fractures are more common in tibia than in any other major long bone. Materials and Methods: This study was performed with 25 open fractures of tibia with reamed interlocking intramedullary nailing in Bangalore Baptist Hospital after ethical clearance. All the cases were traumatic in nature and fresh fractures they were treated as early as possible after presentation and the secondary procedures of dynamization, skin grafting and musculocutaneous flaps were done wherever needed. Results: Majority of the patients were from age group 31-40 years, most of the patients were male 22 (88%) and only 3(12%) females. Most common cause of fracture was motor cycle accidents (48%). Right tibial fracture constituted majority of the patients, most of the open fractures of the tibia were Gustilo type I (56%), most of the fractures occurred at distal third tibia (40%). Most of the patients were operated 4 hours to 9 hours days after trauma (76%), mean operation time was 90 minutes. Conclusions: We can conclude that reamed interlocking intramedullary nailing with the help of image intensifier seems feasible in open diaphyseal fractures of the tibia. Early mobilization of the patient which helps in healing of the fracture and prevents joint stiffness. Minimal blood loss and minimal risk of infection. It also promotes early union as it does not disturb the anatomy and physiology of vascularity at the fracture site.
Key Words: Open fracture tibia; reaming; interlocking intramedullary nailing.
INTRODUCTION
Tibial diaphysical fractures are the commonest long bone fractures encountered in clinical orthopaedic practice. According to a study there is a bimodal distribution of tibial fractures with a preponderance in young males.1 As one third of the tibial surface is subcutaneous throughout most of its length, open fractures are most common in tibia than in any other long bone. Furthermore the blood supply of tibia is more precarious as compared with other bones of the body enclosed by heavy muscle tissue.2 Treatment of the tibial fracture requires the experience and the best of clinical judgment in order to choose the most appropriate management plan for a particular pattern of injury.3,4 There are various modalities of treatment available such as conservative gentle manipulation and use of leg cast, open reduction and internal fixation (with plates and screws), intramedullary fixation (including Ender pins, intramedullary nails and interlocking intramedullary nails with or without reaming) and external fixation techniques. Surgeon should be capable of using all these techniques and must consider advantages and disadvantages of each one and select the best possible management plan. The best treatment should be decided by- morphology of the fracture, the amount of energy imparted, the mechanical features of the bone, age and general conditions of the patient and last but not least the status of the soft tissues. As a dictum 3 goals must be met for the successful management of open fractures of tibia.1-prevention of infection, 2- achievement of bony union and 3-the restoration of function. These goals are interdependent and usually are achieved in the chronologic order given. For example- in a given case failure to prevent infection promotes delayed union or non union and delays functional recovery of the limb. Immobilization in a plaster cast which was most commonly done in the past but it does not always maintain the length of the tibia and it leaves the wound relatively inaccessible.5 According to some studies open reduction and internal fixation with plates and screws has resulted in unacceptably high rates of infection.6,7,8 This method may be used in selected injuries, associated displaced intra articular fractures. External fixation, considered the treatment of choice by many, has some disadvantages including bulky frames and frequent pin track infections, non-unionsand malunions.6,9 Though controversies exist over the best methods of stabilization of open fractures of tibia but recently interlocking intramedullary nailing is gaining much acceptance.10
MATERIALS AND METHODS
The present study was undertaken at the department Orthopedics, Bangalore Baptist Hospital after obtaining ethical clearance. Type Of Study: Prospective and retrospective study (descriptive study) Source Of Data: Data was collected from the patient presenting with open fractures of tibia (type I to type IIIB) at Bangalore Baptist Hospital. For retrospective cases the entire data since admission to regular follow-up will was obtained from the Medical Records Department (MRD),Bangalore Baptist Hospital. This study involved both male and female patients with open fractures of tibia, who presented to Bangalore Baptist Hospital; Bangalore. 25 patients who had open fractures of tibial shaft were treated with wound debridement and reamed interlocking intramedullary nailing during the period from January 2007 to December 2008. All the cases were fresh fractures and were traumatic in nature. All the patients were brought to the casualty.
Inclusion Criteria: Patients with age more than 18 years. Shaft fractures within 4cms distal to the tibial tuberosity to 4 cm proximal to the ankle joint in tibia in which the medullary canal was large enough to accept minimum 8mm nail. Open fractures type I, II, IIIA and IIIB according to Gustilo Anderson classification.
Exclusion Criteria: Fractures lying proximal to the tibial tuberosity. Pathological fractures. Intra-articular extension of fracture. Gustilo- Anderson type IIIC open fractures. Ageless than 18 years. Polytrauma patient.
RESULTS
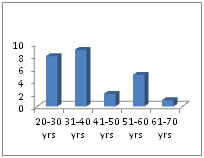 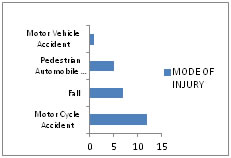 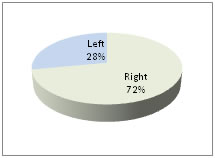
Figure 1: Age distribution Figure 2: Mode of injury Figure 3: Side Affected
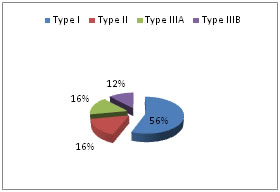 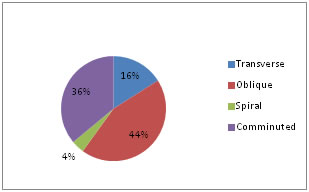
Figure 4: Fracture classification Figure 5: Pattern of Fracture
The present study 25 open fractures of the tibial shaft surgically treated with reamed interlocking intramedullary nailing from January 2007 to December 2008, at Bangalore Baptist Hospital, Bangalore were included.
- Age distribution: Majority of the patients were in the age group 31-40 years, the youngest patient was 20 years old and the oldest being 70 years. The average age of all cases in the series was 38.44 years.
- Sex distributing: Majority of the patients were males 22 (88%) and only 3(12%) were females.
- Mode of injury: The major cause of fracture in our study was motor cycle accidents, (48%) (Graph no 3).
- Side of fracture: Right tibial fracture constituted majority of the patients, 22 patients (66%) were having right tibial fractures (Graph No.4).
- Fracture classification: Majority of the open fractures of the tibia were Gustilo type I (56%) in our study, (Graph No.5), Majority of the fractures occurred at distal third tibia (40%). The predominant tibial fracture pattern was oblique (44%) (Graph no 6).
- Statistics of surgery: Most of the patients in our study were operated between 4 hours to 9 hours days after trauma (76%), 3 cases were operated less than 3 hours of trauma (12%), 3 cases were operated at 12 hours of trauma (12%), All cases were operated under spinal anesthesia. Our mean operation time was 90 minutes. ( Range 60 min. to 120 min).
- Commencement of PWB: In our study all cases were mobilized with NWB crush walking/walker on next day. For most of the patients PWB was started by 4 weeks postoperatively (40%). In 2 cases PWB was delayed for 12 weeks (8%), as these cases had more comminuted fractures with unstable fixation and grade III soft tissue injury with prolonged soft tissue healing duration.
- Commencement of FWB: In our study 17 patients were commenced to protective FWB at 12 weeks postoperatively (68%), most of the patients were commenced to protective FWB by 16 weeks postoperatively (92%)
- Secondary procedure: Dynamisation of the nails was done in three (12%) of patients. Skin grafting was done in 1 case (4%). In 1 case (4%) bone grafting was done.
- Age distribution: The average age of all cases in the series was 38.44 years. The fracture is more common in the age group of 31 – 40 years
- Sex Distribution: There were 22 male and 3female patients showing male preponderance.
- Nature of violence: Majority of the cases sustained fractures from road traffic accidents. Seven patients who sustained fracture after a fall.
Results: In several reported series as well as in our series, the open fractures of shaft of the tibia treated with reamed interlocking intramedullary nailing have given excellent results. In our series out of 25 cases, 23 (92%) fractures united within 6 months of injury, is comparable with the other series as well. Union took 26 weeks in 1 patient and one patient had nonunion with severe communication and extensive soft tissue injury. The physiological and stable fixation with reamed interlocking intramedullary nailing should lower the rates of infection and malunion and expand the use of intramedullary locked nails to the tibial fractures with severe degree of communition and soft tissue injury. (Gustilo type I to type IIIB). In our study all cases were mobilized with NWB crush walking/walker on next day. For most of the patients PWB was started by 4 weeks postoperatively (40%). In 2 cases PWB was delayed for 12 weeks (8%), as these cases had more comminuted fractures with unstable fixation and grade III soft tissue injury with prolonged soft tissue healing duration. 17 patients were commenced to protective FWB at 12 weeks postoperatively (68%), in our study most of the patients were commenced to protective FWB by 16 weeks postoperatively (92%). In the current series, there was one superficial infection (4%). This patient had Type III B open fracture with gross contamination. This patient presented late after the injury to Hospital and surgery was done 12 hours after injury (as patient presented late).The infection was controlled with course of oral antibiotics (according to culture and sensitivity).The incidence of superficial infection (4%) favorable compared with external fixation (6-14% deep infection rates) and other methods. In our series 1 patient had shortening of 5mm and one patient had less then 50 valgus union (fracture of proximal third of tibia). These findings in our study are comparable with the early results of reamed interlocked intramedullary nailing of open tibial fractures by other authors.18 In our study there was no implants failure. We recommend dynamisation of most statically locked nails at 10-12 weeks if callus is not evident to promote fracture union and to avoid fracture of the interlocking screws. In our study, 17patients had (68%) full range of knee motion, in 22 patients (88%) full range of ankle motion at 12 weeks of injury. Knee and ankle movements started immediately postoperatively, except in few cases with fracture more distally( below distal one third) and proximal one third with comminution. Our results are comparable with other series of studies. In our study two patients (8%) noticed pain at the knee joint. In our study, no patient developed fat embolism, compartment syndrome, peroneal nerve palsy and reflex sympathetic dystrophy. At the end of the study each patient was individually assessed by Johner and Wruh’s criteria for functional outcome, in which17 Patients (68%) had excellent results, 7 Patients (28%) had good results and one had (4%) had poor result. This patient with poor result had superficial infection, mild limp with knee pain, less than 80% of knee and less 50% of ankle motion and had non union. The probable cause of the poor results in this patient with above mentioned complications are This patient had Type III B fracture, with extensive soft tissue contamination. This patient presented late after the injury to Hospital and surgery was done 12 hours after injury (as patient presented late). Weight bearing was delayed as this patient had comminuted fracture. This patient had severe soft tissue injury (Type III B) and wound healing was delayed. Hence limb was immolilized in below knee slab for more than three weeks. Therefore moblization and also weight bearing was delayed.
DISCUSSION
Open tibial fractures, which usually caused by high energy trauma, have multiple problems resulting from the poor soft tissue coverage of bone and limited blood supply of the tibia, cause malunion, infection and sometimes amounting to amputation. With recent advancements in wound coverage techniques and fixation devices have considerably decreased the prevalence of these complications, but the optimum treatment of open fractures of the tibia is still evolving.11 There are 2 major factors related to the lesion that the final outcome of tibial shaft fractures- 1-Severity of the fracture, characterized according to the author3 by the degree of initial displacement, communication and soft tissue injury. 2-Damage of the tibial blood supply. Using stabilization technique that avoids additional disruption of this blood supply. Application of a plaster cast has been the most common method of treatment for open fractures of the tibia previously, but it has several disadvantages. According to Nicoll EA 3 rate of infection was 15 percent after the treatment of 140 open tibial fractures with a cast. According to Brown PW et al 5 - 27 percent of 63 open fractures of the tibial shaft had healed with more than ten millimeters of shortening; and 6.3 percent, with more than thirty millimeters of shortening. Unstable and open fracture can be managed with plaster casts incorporating transfixion pins. 12 This method has been valuable for distal tibial fractures, including those with joint extension, especially the rotation type pilon fractures. This has the disadvantage of severe pin tract infection and pivoting of the bone and angulation at the site of fracture. Plate osteosynthesis results in rigid fixation of an unstable fracture and reduces the problem of non-union. The stripping of soft tissue which is required for application of a plate, however, has led to high rate of infection in patients who have an open tibial factures. Johner R et al13 reported non-union was twice as common and rate of infection 5 times more likely when open tibial fractures were treated with plating, so use of plate remains not so attractive treatment option. External fixation techniques has several advantages in the treatment of severely communited open tibial shaft fractures (grade IIIB and C), resulting in early stabilization in patients with polytrauma, improving the survival rate of injured structures and permitting mobility to prevent general complications in these patients. To avoid some of these complications, some authors, have recommended the use of secondary intramedullary nailing after external fixation, but this procedure has an increased prevalence of deep infections after delayed conversion or previous pin tract infections. In the various intramedually devices available for treatment, the unreamed unlocked nails have produced good results in open tibial fractures but the implant did not adequately stabilized the comminuted factures or segmental fractures. Some authors believe that intramedullary nailing with reaming may be used safely for fractures with less severe wounds. Klemm KW et al 14 in his study reported that 6 infections (6.5 percent) developed after the use of interlocking intramedullary nailing with reaming in a large series of 93 grade – I open tibial fractures. Bhandari M et al shown that reamed interlocking intramedullary nailing has many advantages as compared unreamed interlocking intramedullary nailing15 The advantages of reaming include reduced incidence of delayed union, hardware failure and requirement of secondary procedures. Finkemeier et al have shown that canal reaming did not increase the risk of complications in open tibia fractures and earlier time to union without increase in complications in closed tibial fractures.16 According to Keating JF et al reamed locking intramedullary nailing is safe and effective techniques for the management of open tibial fractures.17,18 From the above discussion it is clear that, reamed interlocking intramedullary nailing combines the most desirable features of external skeletal fixation and of non – locking nailing without reaming. Alignment, Length and rotation are controlled, the soft tissues are more easily accessible and endosteal vesscular supply is regained fast. These factors should help in decreasing the rates of infection and malunions and expand the use of intramedullary nails to fractures near the metaphysis and to those with more severe communition and soft tissue injury. In current series 25 cases of open fractures of shaft of the tibial were treated by reamed interlocking intramedullary nailing over a period of two years. They were followed up for an average of 6 – 10 months. The purpose of this study was to evaluate the function outcome in these patients. These cases were of different age groups, occurred in both sexes and the fracture were of different types and at different levels.
CONCLUSION
We conclude that- Reamed interlocking intramedullary nailing with the help of image intensifier seems feasible in open diaphyseal fractures of the tibia. Early mobilization of the patient which helps in healing of the fracture and prevents joint stiffness. Minimal blood loss and minimal risk of infection. Promotes early union as it does not disturb the anatomy and physiology of vascularity at the fracture site. We are also of the opinion that ideally locking all the proximal and distal holes to avoid malunion and fatigue of locking bolts. Minimal hospital stay and early returns to activities with acceptable complications rate as compared to other modalities of treatment, overall reduced morbidity. Cost effective as per reduced need for outpatient care, earlier return to work and cessation of sick benefit compensation.
REFERENCES
-
Bucholz and Heckman’s ROCKWOOD GREENS: FRACTURES IN ADULTS, Vol 2:5th edition 2001, Lipincott Williums and Wilkins Company, USA, pages 1939 – 1994.
-
Terry Canale’s CAMPBELL’S OPERATIVE ORTHOPAEDICS Vol 3,10th edition, 2003. Mosby publishers, pages 2754 – 2782.
-
Nicoll EA, 1964: “Fractures of the tibial shaft; a survey of 705 cases” J Bone Joint surg. 16B 17338.
-
Watson – Jones: “Injuries of the leg”. Chapter – 32in Watson Jones fractures and “Joint injuries” 6th Edn, Wilson JN (Ed), B.I. Churchill Livingstone, New Delhi 1998 387pp.
-
Brown PW, Urban JG, 1969: “Early weight bearing treatment of open fractures of the tibia: An end result-study of sixty three cases” J Bone Jiont Surg, 51A:59-75.
-
Bach A W, and Hansen Jr: ST,1989: “Plates versus external fixation in severe open tibia shaft fractures: A randomised study” Clin Orthop: 241:89-94.
-
Ruedi T, Webb JK, and Allgoer M, 1976: “Experience with the dynamic compression plate (DCP) in 418 recent fractures of tibial shaft” injury, 7:252 – 257.
-
Smith JE 1974: “Results of early and delayed internal fixation for tibial shaft fractures: A review of 470 fractures” J Bone Joint Surg (Br), 56-b 469-477.
-
Holbrook JL, Swiontiowski MF, Sanders R 1989: “Treatment of open fractures of the tibial shaft: Ender nailing versus external fixation; a randomised prospective comparison” J Bone Joint Sur, 71A:`131 –1238.
-
Vineet Jain, Ayush Agarwal, A M Mithaiani, Punkaj Jain, Vishal Garg, B K Dhan. Dept of Orthopedics, M.A.MC and associated L N Hospital, New Delhi. Indian Journal of Orthopedics 2000, Vol 39, Issue 1, Page 30 – 32.
-
Whittle AP Russell TA, Taylor JC, Lavelle DG, 1992: “Treatment o open fractures of the tibial shaft with the use of interlocking nailing without reaming”. J Bone Joint Surg, 74A:1162 – 1171.
-
Anderson LD, Hutchens WC, Wright PE, and Disney JM, 1974: “Fractures of the tibia and fibula treated by casts and transfixing pins” Clin Orthop. 105: 179 – 191.
-
Johner R, and Wruhs O. 1983: “Classification of tibial shaft fractures and correlation with results after rigid internal fixation”. Clin orthop, 178:7-25.
-
Klemm KW, Borner and Mortin. 1986: “Interlocking nailing of complex fractures of the femur and tibia” Clin orthop, 212:89-100.
-
Bhandari M, Guyatt G H, Tony D, Adili A, Shounghnessy S G : “Reamed versus Non-reamed Intramedullary Nailing of Lower Extremity of Long Bone Fractures. A systemic overview and meta-analysis.” JOT 2000; 14: 2-9.
-
Finkemeier, Christopher G, Schmidt, Andrew H Kyle, Richard F, Templeman, David C, Varecka, Thomas F. “The Prospective Randomized Study of Intramedullary Nails Insertion with and without Reaming for the Treatment of Open and Closed Fractures of the Tibial Shaft.” Journal of Orthopaedic trauma 14(3):187-193, March/April 2000.
-
Keating J F, O’Brien P J, Blachut P A, Meek R N, Broedkhuyse H M. Vancouver British Columbia, Canada. J Bone Joint Surg [Am] 1997; 79-A; 334-41.
-
Reamed Interlocking Intramedullary Nailing of Open Fractures of Tibia.” Keating J F, O’Brien P J, Blachut P A, Meek R N, Broekhuyse H M. Clin Orthop Res. 1997 May; (338):182-91.
|
|