Official Journals By StatPerson Publication
|
Table of Content - Volume 8 Issue 2 - November 2018
Association between femoral stem positioning and functional outcome in total hip arthroplasty
Aakarsh Mahajan1, R N Shewale2*
1Resident, 2Professor and HOD, Department of Orthopedics, MGM Medical College and Hospital, Aurangabad, Maharashtra, INDIA. Email: mahajanaakarsh15@gmail.com
Abstract Background: The development of uncemented stems with hydroxyapatite (HA) coating may decrease the incidence of loosening, distal migration and may enhance integration and prosthetic stability. Aim: To evaluate the functional and radiological outcome in patients with primary ceramic-on-ceramic Total Hip Arthroplasty in the management of hip joint pathologies. Material and Methods: A total of 30 hips of either sex, undergoing ceramic on ceramic total hip arthroplasty were prospectively evaluated over a period of two years. All patients were examined radiologically and clinically post-operatively for functional outcome with Harris Hip score and Modified Merle d'Aubigné and Postel Score. Results: Stem alignment was central in 93.33 % of cases (28 cases) and valgus in 6.67 % cases. On comparison of post-operative Harris Hip Score among different alignment of stems, no significant association was found (p value = 0.246). On comparison of post-operative Modified Merle d’Aubigné and Postel Score among different alignment of stems, no significant association was found (p value=0.765). There were no major complications observed in any of our patient. Conclusion: Total Hip Arthroplasty with primary ceramic-on-ceramic technique provides excellent clinical outcome and provides early rehabilitation. Key Word: Total Hip Arthroplasty, ceramic-on-ceramic, Harris Hip Score, Modified Merle d’Aubigné and Postel Score, Outcome
INTRODUCTION Total hip arthroplasty is one of the most successful and cost-effective surgical procedures and remains the treatment of choice for long-term pain relief and restoration of function for patients with diseased or damaged hips.1 The first generation of cementless femoral stems and subsequent generations of uncemented femoral stems have been developed to address complications like osteolysis and the volume of micro particles, which are released from implant surfaces by friction during normal joint function.2 The development of uncemented stems with hydroxyapatite (HA) coating may decrease the incidence of loosening, distal migration and may enhance integration and prosthetic stability. Bearing technology has focused on increasing implant survival by decreasing wear and resulting osteolysis, and reducing dislocation rate. Bearing surfaces are of two types: low wear metal on polyethylene articulations and bearing surfaces such as ceramic-on-ceramic. Early reports on ceramics-on-ceramics total hip arthroplasty have demonstrated excellent clinical and radiological results. The theoretical advantages of ceramic-on-ceramic are represented by its remarkable sliding characteristics and its very low wear debris generation. The present study was conducted to evaluate the functional and radiological outcome in patients with primary ceramic-on-ceramic Total Hip Arthroplasty in the management of hip joint pathologies
MATERIAL AND METHODS A total of 30 hips of either sex, undergoing ceramic on ceramic total hip arthroplasty were prospectively evaluated over a period of two years. Inclusion Criteria
Exclusion Criteria Patients with following conditions were excluded from the study:
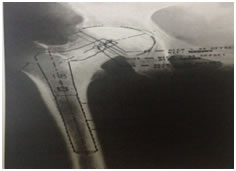
Preoperative work up After taking informed consent, all patients underwent detailed clinical and radiological examination along with all routine investigations. Pre-operative Harris hip score3andModified Merle d'Aubigné and Postel Score4,5 were calculated for all the patients. Pre-operative templating Pre-operative leg length discrepancy was determined, clinically and with a radiographic analysis. Acetabular templating was performed first because the acetabular component establishes the centre of rotation of the arthroplasty. Acetabular templating was done by placing the template of the cup of the appropriate size, extending from the supero-lateral margin of the acetabulum upto the lateral margin of the teardrop infero-medially. The template which matched the contour of the acetabulum without removing excess subchondral bone was chosen. This centre of the acetabulum component determined the centre of rotation of the hip joint (Fig. 1).For the templating exercise, the acetabular centre of rotation is considered the fixed reference and the femoral head centre is considered variable. Figure 1: Acetabular templating
The femoral component template size that fitted the distal femur and equalised leg lengths was selected. Proper offset was determined by matching the cup’s centre of rotation with the desired head centre of rotation (Fig. 2). The neck resection line was drawn at the point where the selected stem provided the desired amount of leg length. The stem size chosen in the A-P plane was also verified in the lateral plane.
Figure 2: Femoral stem selection
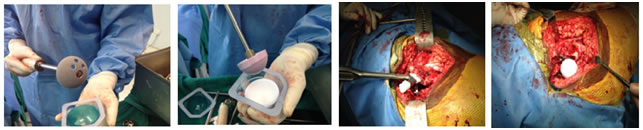
Surgical Technique All patients were positioned in a lateral position on the table with the side to be operated facing towards the ceiling. The hip joint and proximal femur were exposed either through anterolateral approach or posterolateral approach (Fig. 3). Figure 3: Positioning of the patient Figure 4: Intra-op Femoral Neck templating The trial stem was aligned with the centre of the femoral shaft, and matched the centre of the trial femoral head with that of the patient. Neck was resected at same distance from the tip of the lesser trochanter, as was determined by pre-operative templating (Fig. 4). Osteotomy was performed with an oscillating power saw. Femur was retracted anteriorly with bone hook to keep anterior capsule under tension and aid its cut. After cutting anterior capsule curved cobra or Hohmannretractor was used to expose the acetabulum. Acetabular cavity was reamed with subsequent reamers. The acetabular cup was then inserted in correct inclination. Appropriate sized ceramic liner was placed (Fig. 5 and 6). Figure 5 Figure 6 Figure 7 Figure 8 Legend Figure 5: Acetabular cup; Figure 6: Ceramic liner; Figure 7: Femoral stem insertion; Figure 8: Femoral head placement
After serial reaming of the femoral canal, taking anteversion in consideration, femoral stem was inserted (Fig.7). Ceramic femoral head was placed and reduction was done (Fig. 8). Capsule was closed, drain placed and wound was closed in layers. Post-Operative Management On first post-operative day, radiographs were done bedside only, to check the position of the implant. Isometric quadriceps and gluteal exercises were started from 2nd post-operative day. The suction drains were removed after 48 hours. All patients were immobilised with an abduction splint for 48 hours and thereafter an abduction pillow was given. Intravenous antibiotics were continued for 72 hours post-operative. All wounds were routinely inspected on fifth day and at the time of suture removal on fourteenth day unless there was a specific indication e.g. fever. All these patients were kept in the ward at least till the time of suture removal and then discharged. Partial weight bearing was started on 2nd post-op day and gradually increased as tolerated by the patient. Full weight bearing was generally started after 6 weeks. The patients were followed up at 6 weeks, 3 months, 6 months and 1 year and then annually. At each visit patients were assessed for clinical/functional status, radiological evaluation, complications-early or late.
RESULTS Age varied from lowest of 21 years to highest of 64 years. Maximum number of patients (i.e.9) were from the age group of 31-40 years. Mean age at the time of surgery was 40.9 years.25 patients (83.33%) in our study were males and 5 were females (16.67%) with Male: Female ratio of 5:1. Out of 30 patients, 19 (63.33%) were operated on right side, and 11 (36.67%) were operated on left side. Out of a total of 30 cases, 19 (63.33%) were those with avascular necrosis, 9 (30%) cases were of trauma (of which 6 were neck of femur fractures, one intertrochanteric fracture, and one was acetabulum fracture), and one case each (3.33%) were of ankylosing spondylitis and rheumatoid arthritis. All the patients were outinely followed up at 6 weeks, 3 months, 6 months and 1 year after surgery. Maximum duration of follow up was 21 months, and minimum was 8 months. Mean period of follow up was 14.63 months. Pre-operatively the mean Harris Hip Score was 35.03 (Range from 20 to 44), which increased to a mean of 88.43 (Range from 74 to 95) post-operatively. 90% of hips had good to excellent results at latest follow up. This improvement in Harris Hip Score from a mean of 35.03 pre-operatively to 88.43 post-operatively, is statistically significant (p value < 0.0005). Pre-operatively the mean Modified Merle d'Aubigné and Postel Score was 9.33 (Range from 6 to 12), which increased to a mean of 16.17 (Range from 13 to 18) post operatively. 90% of hips had good to excellent results at latest follow up. This improvement in Merle d'Aubigné and Postel Score from a mean of 9.33 pre-operatively to 16.17 post-operatively, is statistically significant (p value < 0.0005). Stem alignment was central in 93.33 % of cases (28 cases) and valgus in 6.67 % cases (2 cases).
Table 1: Alignment of femoral stem
On comparison of post-operative Harris Hip Score among different alignment of stems, no significant association was found (p value = 0.246). Table 2: Comparison between stem alignment and post-operative Harris hip score
On comparison of post-operative Modified Merle d’Aubigné and Postel Score among different alignment of stems, no significant association was found (p value = 0.765). Squeaking was not found in any of our patient. None of the patients showed heterotopic ossification, osteolysis, or stem loosening. There were no major complications observed in any of our patient. Table 3: Comparison between stem alignment and post-operative Modified Merle d’Aubigné and Postel score
DISCUSSION Ceramic bearings are widely used in Total Hip Arthroplasty along with metal and polyethylene bearings. There were several studies in past few years accessing the advantage of one over the other. The mean age of patients in our study was 40.09 with age ranging from 21 to 64 years; majority of them being from age group 31-40 years. Nizard et al6 reported on ceramic-on-ceramic hips that had been implanted in a group of 101 patients (132 hips), younger than 30 years old (mean age: 23.4 years,range: 13-30 years). In our study, age was not associated with any significant difference in the clinical outcome, as suggested by age distributed mean Harris Hip scores and Modified Merle d'Aubigné and Postel scores. In our study, out of 30 hips, 5 were that of females with male: female ratio of 5:1. A study conducted by Reuven et al7 included 10 males and 40 females. No significant statistical differences were seen comparing pre and post-operative Harris hip scores. We too did not find any correlation between the sex of the patient and clinical outcome. This increased male to female ratio in our study could be due to the fact that in Indian context, males are more exposed to trauma due to increased outdoor activity level, and also to avascular necrosis due to smoking and consumption of alcohol. The mean period of follow up in our study was 14.63 months (ranging from maximum of 21 months to minimum of 8 months). This follow up is small due to limited time frame we had but we intend to continue the study for longer period. Lins et al8 reported 81% of femoral componentsand 97% of acetabular components were stable at mean follow up of 60 months following uncemented fixation, while Mont et al9 reported good to excellent results in 94% of patients at short-term follow-up. We evaluated the clinical outcomes based on Harris hip score and Modified Merle d'Aubigné and Postel score as has been done by various authors. The mean Harris hip score in our study increased from 35.03 pre-operatively to 88.43, post operatively at the latest follow up with 90% hips having good to excellent results. The Modified Merle d'Aubigné and Postel score in our study increased from 9.33 pre-operatively to 16.17 post-operatively with 90% hips having good to excellent results. This improvement was statistically significant (p<0.005). Our results are comparable to a study done by Reuvenet al7in which pre and post-op Harris Hip scores were 45 and 88 respectively with 80% patients having good or excellent results. Another study was done by Millar et al10 in which pre and post operative Harris hip scores were 29.4 and 85.7 respectively at minimum of 24 months of follow up. On evaluation of alignment of femoral stem 28 stems were central (93.33%) and 2 stems in Valgus (6.67%) and none in varus position. There was no significant correlation between stem alignment and clinical outcome based on Harris hip score or Modified Merle d'Aubigné and Postel score. Long term follow up is needed to show exact result of this. No cases of focal osteolysis or heterotopic ossification were seen in our study. This is in contrast with study of Simonet al11 where osteolysis was seen in 6 out of 34 hips, 3 being grade 1, 2 grade 2 and 1 grade 3. Various other authors have reported osteolysis ranging from 7% to 78% (Christie12, Tanzer13, Bono14). This could be due to shorter duration of follow up in our study and small number of study population. Stem loosening was not seen in any patients till recent follow up. This is in accordance with study of Simonet al11 where osteolysis was seen in only 1 out of 34 cases with long follow up without clinical signs of loosening. Squeaking was not seen in any patient in our follow up. Jarrett et al15 described a group of 131 patients from which 14 (10.7%) suffered an audible “squeak” during normal activities (however, only 4 of these patients were able to reproduce the “squeak” during the clinical review session). After 10 years of follow-up Chevillotte et al16 discussed the performance of 100, third generation ceramic-on-ceramic joints. By use of a questionnaire, 5% of these patients reported the occurrence of “squeaking”. All of these patients were active, sporty and heavy men. None of the major threatening complication was noticed during evaluation of our cases. A study was done by Aoude et al17, in which outcome of 133 total hip arthroplasties with ceramic on ceramic bearings was analysed. In this study, one hip underwent two staged revision for infection and another underwent revision for dislocation. In our study, we have achieved excellent clinical outcome and fixation by bony ingrowth comparable to available literature. Osteolysis and heterotopic ossification were not seen in any of the patients as reported in literature, which could be due to short period of follow-up. No major threatening complication was seen in our study. The limitation of our study includes the lack of a control group with alternate bearing surfaces, and lack of longer term follow up.
REFERENCES
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home