Official Journals By StatPerson Publication
|
Table of Content - Volume 8 Issue 2 - November 2018
Arthroscopic management of giant cell tumor from the posterior cruciate ligament
P Saravanan1, T Sundararajan2*
1,2Associate Professor, Department of Orthopedics, Shri Sathya Sai Medical College and Research Institute, Ammapettai village, Nellikuppam-603108 Kanchipuram, Tamil Nadu, INDIA. Email: psaravanan_21@yahoo.co.in
Abstract Tenosynovial Giant Cell Tumor originates fromsynovium of the joints, tendon sheaths, mucosal bursa and fibrous tissue adjacent tissues. These tumors predominantly involve the palmar side of the fingers and toes and seldom present in large joints. Intra articular Giant Cell Tumor is a very rare clinical condition in Orthopedics. Magnetic Resonance Imaging (MRI) is the best non-invasive diagnostic tool to confirm Tenosynovial Giant Cell Tumor and further confirmed by arthroscopic excision and histopathological examination. This is a case report of a 24-year-old male with complaints of pain in right knee joint for two years with no history of trauma. MRI right knee joint revealed an intra articular mass attached behind the Posterior Cruciate Ligament. Arthroscopy was performed and mass removed for histopathological examination which confirmed the diagnosis of Giant Cell Tumor from the Posterior Cruciate Ligament. Key words: PCL, Giant Cell Tumor, Arthroscopic Management.
INTRODUCTION Tenosynovial Giant Cell Tumor originates from synovial tissue of the joints, tendon sheaths, mucosal bursa and fibrous tissue adjacent to the tissues1. The disease usually presents in localized and diffused forms. It is a rare condition especially seen in large joints such as knee2-4. This article reports rare condition affecting the knee joint1,3,5in a 24 year old male with Tenosynovial Giant Cell Tumor originating from the Posterior Cruciate Ligament (PCL).
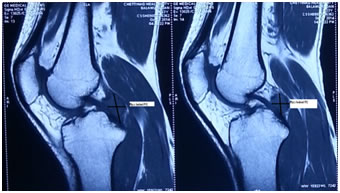
CASE REPORT A 24 year old male who is a mechanic by profession presented with right knee pain for two years duration. The pain was mild to moderate, progressive and worsening during heavy work. No previous history of injury. Clinical examination revealed no localized swelling and tenderness around the knee joint. Range of motion was normal except limited pain during flexion. The special tests for knee instability like Lachmann, Anterior and Posterior Drawers test, Pivot shift test were negative. Meniscal tear tests were negative. All his biochemical and serological lab values were normal. Figure 1: Magnetic Resonance Image of T2 weighted showing a well defined mass measuring 2.1x1.8cm present behind the PCL in sagittal section taken a year back.
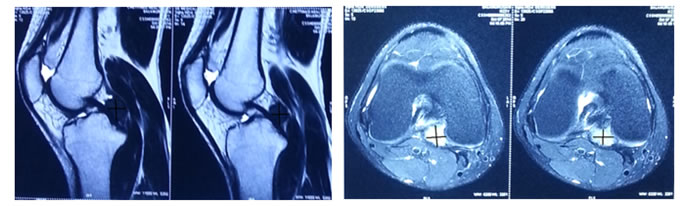
Figure 2a: MRI of T2 weighted sagittal picture taken recently showing a well-defined, circumscribed mass present behind the PCL. Figure 2b: MRI of T1 weighted Axial picture taken recently showing a well-defined, circumscribed mass present behind the PCL
Magnetic Resonance Imaging (MRI) of the right knee joint which was taken one year backrevealed an Intra articular, well circumscribed lesion seen just behind the Posterior Cruciate Ligament (Figure 1). The mass measuring 2.1x1.8 cm was hyperintense on T2 weighted Imaging. It was reported as Pigmented Villonodular Synovitis. A repeat MRI of right knee joint was taken recently after a year which confirmedsame lesion present behind the Posterior Cruciate Ligament with no increase in size and position of the lesion (Figure-2a and 2b). A Diagnostic Arthroscopy of the right knee joint was performed using standard anteromedial and anterolateral portals. Both the Anterior and Posterior Cruciate Ligaments and both menisci were normal. No Chondral lesions present.
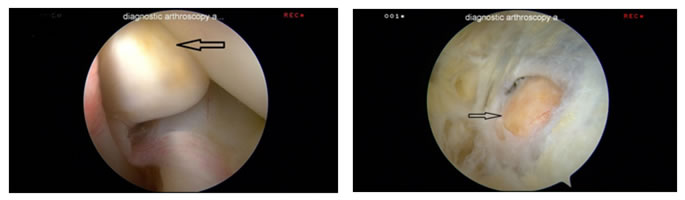
Figure 3: Arthroscopy picture of the mass viewing from the postero medial portal showing the mass lying just behind Posterior Cruciate Ligament. Figure 4: Arthroscopy picture of the mass seen from the postero medial portal.
Figure 5: Arthroscopy picture after the complete excision of the mass seen from the postero medial portal.
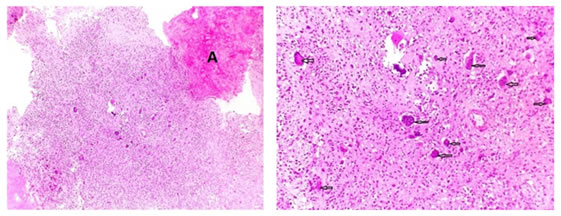
Figure 6: Histo-pathology on Hematoxylin-Eosin staining shows the hyaline cartilage marked as “A” and Multiple Giant cell cells present on fibrous stromal background. Figure 7: On magnification, showing the multiple, multinucleated giant cells (marked with arrows) on a fibrous stromal background
A mass present just behind the Posterior Cruciate Ligament was identified (Figure 3and 4). Accessory postero medial portal was made to get better access to the mass. Mass was well circumscribed and isolated from synovial attachments. A specimen of the lesion was taken using special grasper and sent for histopathological examination. A complete resection of the mass was done using specialized arthroscopy shaver (figure 5). Histopathological examination confirmed the diagnosis of Giant Cell Tumor (Figure 6 and 7). Post-operative course was uneventful at three and six months follow up. The patient was asymptomatic with no complaints of pain. Pain free full Range of Motion was obtained.
DISCUSSION Giant Cell Tumor originates from the synovial tissue of the joints, tendon sheaths, mucosal bursa and fibrous tissue adjacent to the tissues1. Etiology of Giant Cell Tumor is not completely understood2,4,6. Giant cell tumor in knee joint is very rare with incidence of two per 1,000,000 per year in patients < 40 years old7. The common age group of presentation is between 20 to 50 years. Characteristically there is a long history with a delay in diagnosis8. This is a generally slow growing tumor and incidence in men is two times that of woman8. Knee Joint is the commonest site of intra articular lesion when compared to the other major joints. Patient often presents with intermittently tender, painful joints and joint effusion is usually absent. Although this is considered as a benign condition the diffuse form is more aggressive with high recurrence rate of 25% with intra articular joint and 25%-50% with extra articular disease9. With improvements in the imaging notably, MRI has been the best non invasive technique to diagnose this tumor8. On MRI the lesion demonstrates low signal intensity on T1 and T2 sequences. Marked enhancement is seen on T1 weighted MRI Images after the Intra venous injection of GADOLINIUM8. The differential diagnosis on Magnetic Resonance Imaging includes Rheumatoid Panus, Amyloid Arthropathy, Synovial Haemangioma and Dermoid type fibromatosis which can be resolved on clinical history and laboratory findings. The better treatment of choice for Giant Cell Tumor in the knee joint is by local excision. Arthroscopy has been advocated as safe with good functional results and decreased rates of post-operativeknee stiffness. Local recurrence can occur if excision is incomplete10. There were only few case reports of Giant Cell Tumor from the Posterior Cruciate Ligament has been published in the literature1,3,5. All of them have concluded that Magnetic Resonance Imaging is the best non invasive diagnostic tool to confirm the Tenosynovial Giant Cell Tumor. Arthroscopic removal of lesion was performed in all the reported cases which was confirmed by the histopathological report. All the authors have concluded that total Arthroscopic resection can be an effective surgical technique to remove Giant Cell Tumor from the Posterior Cruciate Ligament in the knee joint.
CONCLUSION In this case report we describe the Giant Cell Tumor arising from the Posterior Cruciate Ligament by the confirmation of Magnetic Resonance Imaging, Arthroscopic findings and further confirmed by histopathological examination. Complete and safe excision of the tumor is better done by arthroscopy with additional portal namely the posteromedial portal of the knee joint. Although this condition is a relatively rare clinical disease, it is necessary to always do a MRI for any patients with the complaints of pain above the age of 20 years with no significant injury or instability in knee joint. A diagnostic arthroscopy should be performed with doubtful diagnosis in MRI, for the confirmation of the diagnosis.
|
|
 Home
Home