Official Journals By StatPerson Publication
|
Table of Content - Volume 8 Issue 2 - November 2018
Management of mucoid degeneration of anterior cruciate ligament
P Saravanan1, T Sundararajan2*
1,2Associate Professor, Department of Orthopedics, Shri Sathya Sai Medical College and Research Institute, Ammapettai village, Nellikuppam-603108 Kanchipuram, Tamil Nadu, INDIA. Email: psaravanan_21@yahoo.co.in
Abstract Background: Mucoid Degeneration of ACL, a rare pathological condition occurring due to deposition of mucinous substance is one of the poorly understood clinical condition affecting the knee joint. This study explains about the clinical assessment and management of patients with Mucoid Degeneration of ACL. Materials and Methods: Twelve patients with a mean age of 33 years were included in this study of which 11 had a clinical history of trivial injury and one patient had a significant injury to knee joint. MRI finding interpreted the presence of thickened and hypertrophied ACL which was confirmed upon Arthroscopy. Debulking was done for ten patients and remaining two underwent ACL reconstruction as one already had torn ACL fibres while other had to be reconstructed due to complete resection while debulking. Notchplasty was not done to any of our patients. Result: Mean follow up of 12 months, ten patients with Debulking of ACL had a pain free terminal flexion. The follow up laxity tests for ACL was good. Conclusion: Mucoid Degeneration of the Anterior Cruciate Ligament should be suspected in patients who had pain on terminal flexion of the knee joint. It was mostly found to be preceded by trivial injury to knee joint. MRI is the most useful investigation to identify the diagnosis which can be confirmed by Diagnostic Arthroscopy. Debulking is the best way of managing the Mucoid Degeneration of ACL to achieve the pain free full ROM. Key Words: Mucoid Degeneration of ACL, Arthroscopic Debulking, Trivial Injury.
INTRODUCTION Mucoid Degeneration of Anterior Cruciate Ligament(ACL), an uncommon condition in knee, is a poorly understood clinical condition affecting knee joint1-3. It occurs due to deposition of mucinous material in ACL in the absence of synovial lining4,5,6. Many theories were suggested7, of which “Traumatic” theory suggesting strain to ACL leading to deposition of glycosaminoglycans8 is considered to be significant. MRI being the preferred diagnostic method9, gets wrongly interpreted to be partial tear of ACL10,11,12. Arthroscopic debulking is the preferred choice of management1,11,13. The main purpose was to understand the clinical condition, diagnostic tools and management of mucoid degeneration of ACL.
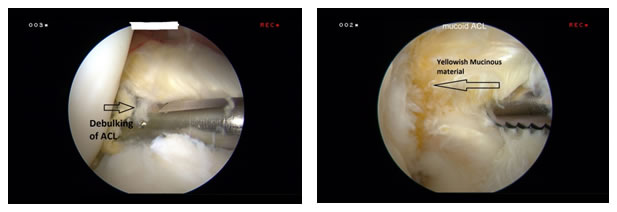
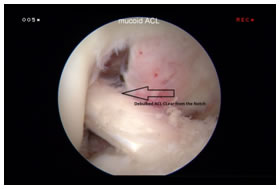
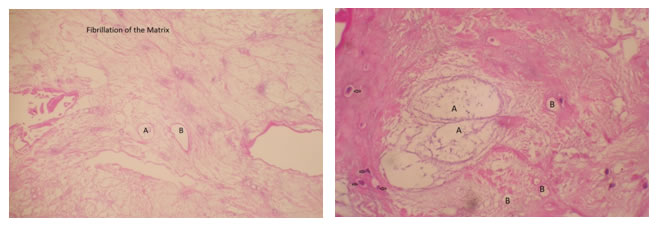
MATERIALS AND METHODS This is a prospective study of 12 patients who were diagnosed to have Mucoid Degeneration of ACL during a period of two years from January 2016- January 2018.A detailed history was elicited from all the patients including history of recent trivial trauma, pain and their activity levels. A proper clinical examination of knee joint was done for all patients. MRI was done as the standard investigation procedure for all patients. The radiological findings reported ACL as thick, hypertrophied, covering inter condylar notch. Three patients were reported to have a partial tear of ACL in both T1 and T2 weighted images. For one patient, following a road traffic accident, MRI was reported to show a complete tear of the ACL from the femoral attachment. Diagnostic Arthroscopy was performed in all patients with a 4mm high definition arthroscope through a standard anterolateral and anteromedial portal. The syonovium, both menisci and the cartilage were examined. ACL was examined with the arthroscopy probe. ACL appeared to be yellowish, thick and hypertrophied occupying the intercondylar notch. It was found impinging on the lateral aspect of the notch in flexion. Careful debulking of ACL was done to ensure removal of only the degenerated portion to avoid complete excision of ACL. The yellowish mucinous material was removed with Basket forceps and sent for histopathological examination. Trimmed ACL was examined carefully for any impingement into the notch. Histopathological examination confirmed as a Mucoid Degeneration. ACL reconstruction was done for one patient who ended up with complete resection of ACL even with utmost care and meticulous debulking. Notch plasty was not done to any of our patients since we did not find the debulked ACL impinging into the notch. Cryotherapy was given for immediate post-operative pain relief. For 10 patients who underwent debulking of ACL no immobiliser or brace was given. Full weight bearing and active Range of Movements were started from the first post-operative day. Knee immobilizer was advised for the remaining two patients who underwent ACL reconstruction for the protection of the reconstructed graft. All the patients were followed up postoperatively for a period of 6 to 18 months for pain and laxity.
RESULTS Out of 12 patients included in our study, eight were male and four female [Table 1]. Mean age was 33 years(Range 28 to 38 years). Eleven of the 12 patients had a history of trivial injury to the knee joint and one patient presented to us following road traffic accident (RTA). All patients presented with pain on terminal flexion of the knee joint. Median duration of pain was 10 months (Range 3 to 24 months). On careful examination, 11 patients had painful knee on deep flexion with no clinical evidence of ligament laxity whereas the one patient with RTA had a lachmann’s and anterior drawers test positive. The terminal flexion is judged with flexion of more than 1100.
Table 1: Describes the clinical presentation of patients with Mucoid Degeneration of ACL
M=Male, F=Female, ROM=Range of movement
Figure 1 and 2: MRI (T1 and T2 weighted sagittal image). ACL(marked in arrow) appearing as bulky,thick and hypertrophied with celery stalk appearance.
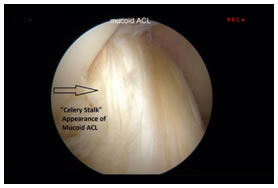
MRI was done for all patients which described the ACL as thick, hypertrophied, appearing as “Celery stalk”6 occupying the entire Intercondylar notch (Figure 1 and 2). In three patients the MRI was reported as a partial tear of ACL.
Figure 3: Arthroscopic image of Right knee, ACL appears bulky, hypertrophied impinging to the lateral femoral condyle. ACL apperaing as celery stalk ( marked in arrow).
Figure 4: Arthroscopic picture of Mucoid ACL showing carefulldebulking of ACL using shaver (marked in arrow). Figure 5: Yellowish mucinous material removed (marked in arrow).
Figure 6: Debulked ACL which is free from notch and adequate thickness is still present (marked in arrow)
Figure 7: Histological slide showing Fibrillation of Matrix with Myxoid degeneration (A) and Microcysts (B). Figure 8: Histological examination showing Myxoid degeneration (A) and Microcysts changes ( B). Chondrocytes seen as marked in arrow.
Arthroscopy was performed in all patients (Figure 3) and a careful and meticulous debulking done (Figure 4,5and6). The excised mucinous material was sent for histopathological examination which confirmed the presence of mucoid degeneration (Figure 7 and 8). One patient had undergone ACL reconstruction as the remaining ACL was insufficient for stability. Four patients had a medial meniscus tear which were oblique and radial present in the avascular region where balancing and trimming was done. None of them had cartilage damage in Arthroscopy. Mean post-operative follow up was 12 months (Range 6 to 18 months). All the patients had regained full range of motion. None of them had pain on deep flexion and had no extension lag. All the patients had resumed their earlier work on an average of 3 months follow up. The Lachman and anterior drawer test were done in the follow up where three patients had grade I laxity and had a firm endpoint which indicates a stable native ACL.
DISCUSSION Mucoid degeneration of ACL is a rare pathology affecting the middle aged and elderly individual1-3. It is often misinterpreted as a partial tear of ACL due to poor knowledge about this condition9-11. Kim et al2 noted Mucoid Degeneration of ACL more commonly in degenerative knees with a mean age of 61 years. The Degenerative Theory states that mucoid degeneration could occur due to aging2. However, the mean age in our study was 33 years where it is explained with different theoretical hypothesis. Lancaster et al14 described the Traumatic theory where repeated micro trauma to the ACL results in cystic secretion in the native ACL which will transform into a mucoid degeneration. In our study 11 patients gave the history trivial injury before the onset of pain. This traumatic etiology seen in our population was well supported by Amiel et al4 where he concluded that the haemarthrosis will cause deleterious effect in an absent synovial lining of ACL. Similarly, Pandey et al13reported that 7 out of 11 patients had previous episode of trivial injury before the onset of pain and absence of synovium in all of his patients. All patients in our study too had absence of synovial lining in ACL. The male to female ratio in our study was 2:1. Bergin et al9 and Salvati et al15 reported with a male to female sex ratio of 1:1 and 1.28:1 respectively. This signifies that the pathological condition is equally distributed in both the genders. Knee pain in both flexion and extension was reported by many authors2,5,7. However, the commonest clinical symptom of Mucoid degeneration of ACL is pain on deep flexion. Studies also showed that pain was present predominantly on the posterior aspect of the knee joint1,2,7,16. Fealy et al5 postulated that the origin of pain was due to increased tension in ACL due to intra tendinous nociceptor irritation. Narvekar and Gajjar17 described the increased mass and tension in the ligament as the cause of pain. All the patients in our study had a significant pain on deep flexion. Arthroscopy is the preferred mode of treatment for the management of Mucoid degeneration of ACL. The arthroscopic features showed an intact ACL which appears thick, hypertrophied and yellowish in colour2,10,17.On examination with a probe all the patients were found to have absence of synovium and ligamentum mucosum9,10,18. On flexion and extension of knee joint, thick ACL fibres were seen impinging against medial aspect of lateral femoral condyle which was the root cause of pain in Mucoid degeneration of ACL. Similarly, pain on posterior aspect is explained by the impingement on PCL and posterior capsule2,19. There are reports of associated cysts formation in the ACL13. However we did not come across any associated cystic lesions in ACL. Arthroscopic debulking is the most appropriate and effective procedure for the management of Mucoid degeneration of ACL. When the mechanical impingement of ACL is removed we found a respite of pain on deep flexion. This signifies the importance of debulking Mucoid Degeneration of ACL1. Kumar et al20 has proposed a complete resection of the mucoid degeneration of ACL as the only choice of completely erasing the mucinous material from the ACL followed by ACL reconstruction. But majority of the authors believed that only the removal of the mucinous material with careful debulking of ACL will suffice to remove the pathology and relieve pain without producing instability1,13,17. Motmans and Verheyden1 described notchplasty was not routinely needed, as the primary pathology is in ACL and not in the notch. Hence they believed a proper debulking will ensure removal of pathology. Notchplasty was not done for any of our patients since a proper and judicious debulking is sufficient to correct the pathology. However there were many authors who felt the need ofnotchplasty especially in individuals with a narrow notch and also elderly patients due to presence of osteophytes12,18,21,23. We did not encounter such problems in our patientsas the age group of patients was middle age who were free from osteophytes and none were found to havea narrow notch. On Postoperative follow up, all patientsachieved pain free full range of motion with no extension deficit. Two patientshad mild pain, one on squatting and other on sitting cross legged which could be better explained due to other coexisting clinical condition likethe development of osteoarthritis. Out of 10 patients where debulking was done, three patients had grade I laxity and had a firm endpoint which indicates a stable native ACL. None had complaint of instability. Lintz et al23 described an increased anterior tibial translation post debulking in his follow up of 2-5 years whichwas probably due to insufficientleft over of ACL on debulking. Secondary instability is a much anticipated complication in younger individuals where debulking was done24,25. A long term follow up is however necessary to identify instability. In such caseACL reconstruction for patients may prove as an effective source13, especially for patients involved in high demanding physical activity.
CONCLUSION Mucoid degeneration of ACL should be suspected in patients presenting with pain in the knee joint especially following a trivial injury. It is commonly seen in middle aged individuals and also in elderly. The clinical presentation in middle aged individuals is precipitated following trivial injury. A careful clinical history and a proper examination of knee joint and correct interpretation of MRI are key manifestations in diagnosis and management of this condition. MRI is the most important diagnostic toolin identifying the Mucoid degeneration of ACL, yet the surgeons should possess the right skills in interpreting the same. In our opinion, Arthroscopic debulking of Mucoid degeneration of ACL is the treatment of choice. Notchplasty may be restricted to patients having a narrow notch or with osteophytes. The choice of reconstruction of ACL should also be kept in mind in demanding patients as long term follow up suggests the clinical laxity in patients with debulking especially in middle aged individuals.
REFERENCES
|
|
 Home
Home