Official Journals By StatPerson Publication
|
Table of Content - Volume 8 Issue 3 - December 2018
Single stage arthroscopic anterior cruciate and posterior cruciate ligament reconstruction using hamstring tendon autograft
P Saravanan1, T Sundararajan2*
1,2Associate Professor, Department of Orthopaedics, Shri Sathya Sai Medical College and Research Institute, Ammapettai Village, Nellikuppam- 603108, Kanchipuram District, Tamil Nadu, INDIA. Email: psaravanan_21@yahoo.co.in
Abstract Aim: A prospective study of functional outcome of patients with single stage Arthroscopic Anterior and Posterior cruciate ligament reconstruction using hamstring tendon autograft with a minimum follow up of 2 years. Materials and Methods: There were 12 patients included in this prospective study of Arthroscopic ACL and PCL reconstruction using hamstring tendon autograft. The duration of injury to index procedure is from 6 weeks to 12 weeks. The semitendinosus tendon from the uninjured and injured leg was used for PCL reconstruction and Gracilis tendon was used for ACL reconstruction. Both the ACL and PCL grafts were fixed by Endobutton CL on femoral side and Bio absorbable HA interference screws were used for the tibial fixation. Patients were followed up for 2 years and evaluated according to IKDC grade. Results: All the patients in our study had a good knee extension. 3 patients had a grade I laxity on Anterior-Posterior movements. 4 patients had a flexion deficit of 50 and 2 patients with the flexion deformity of 200. The IKDC evaluation 8 patients were graded normal, 3 patients graded near normal and 1 patient with an abnormal grade. Conclusion: A single stage arthroscopic ACL and PCL reconstruction with hamstring tendon autograft will give an excellent result for the multi ligament injuries. A significant improvement in way of function and activity were noted by subjective clinical examination and scales with a minimum follow-up of 2 years. Careful clinical evaluation and good surgical technique will provide a better outcome of surgery for multi ligament injuries in knee. Key Word: Single stage, Arthroscopy, ACL and PCL Reconstruction, Hamstring tendon.
INTRODUCTION Injury to knee with both Anterior and Posterior cruciate ligament tear is often due to high velocity injury and knee dislocation.1,2 There is a marked disability present when associated with medial and lateral complex injuries. Capsular and neurovascular injury is commonly missed out in multiligament injuries and careful evaluation is required.3 Early surgical management for both cruciate ligament tears have been reported,4-6 however a delay in doing surgery will allow healing of the capsule and medial complex injuries non operatively.7A single stage arthroscopic anterior and posterior cruciate ligament reconstruction has been proven to be an effective way of management for multi ligament injuries.8 There are various choices of graft for reconstruction of ACL and PCL have been reported,9,10 the hamstring tendon autograft has been proven to be the most efficient choice of graft for combined cruciate ligament reconstruction.11,12 This is a prospective study of 12 patients with multiligament injuries treated by a single stage arthroscopic ACL and PCL reconstruction with a minimum follow up of 2 years. Only patient with near normal movement of knee and adequate soft tissue healing was taken up for surgery.
MATERIALS AND METHODS This is a prospective study for patients with ACL and PCL tear between the periods of January 2015 to December 2016. There were 12 patients included in this study, of which 11 were male and 1 female. The mean age of patients was 34years (Range22-48). 8 patients had road traffic accident had fall from two wheeler while 4 patients had sports injury. 9 patients presented with right knee involvement and 3 patients with left knee. 7 patients had acute injuries with less than 3 weeks duration and 5 patients had duration of injury between 6 weeks to 10 weeks (Table 1).
Table 1: Patient and injury distribution
M=Male, F=Female, RTA=Road Traffic Accident, LCL= Lateral Collateral Ligament, MCL= Medial Collateral Ligament, MM= Medial Meniscus, LM= Lateral Meniscus, PM= Partial Meniscectomy
Out of 12 patients, 9 had postero medial corner injury with grade II to III valgus instability. Out of which 5 patients had a healed PMC before the index procedure and 2 patients had simultaneous MCL repair and augmentation and 2 patients underwent MCL reconstruction along with main procedure. One patient had a positive PLC tear on clinical examination and simultaneous PLC reconstruction was done. SURGICAL TECHNIQUE All patients were examined under anaesthesia and their clinical findings were recorded. The main procedure was completed in same anaesthesia. Patient positioned supine and both lower limbs were prepared for harvesting of hamstring tendon with both legs under tourniquet control. The semitendinosus and gracilis tendon were harvested using a closed tendon stripper. The harvested tendons were prepared in graft master board where muscles were removed from tendon. Both semitendinosus tendons were quadrupled for PCL reconstruction and 6 strand gracilis tendon was used for ACL reconstruction. The average thickness of the graft for PCL is 9-10mm and for ACL is 7-8mm. The prepared grafts were tensioned in graft master board with tension set at 20lbs and covered with a wet pad. The patellar bone tendon bone graft harvested from injured leg was used for ACL reconstruction for patientswith MCL and PLC tear where the gracilis tendon is used for reconstruction of torn MCL and PLC (Table 2). Table 2: Graft choices for ligament injuries
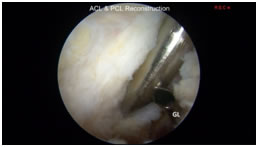
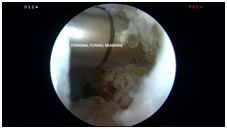
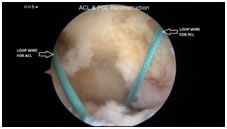
ACL= Anterior Cruciate Ligament, PCL= Posterior Cruciate Ligament, MCL= Medial Collateral Ligament, LCL= Lateral Collateral Ligament, PLC= Postero Lateral Corner, STG= Semitendinosus and Gracilis tendons, ST= Semitendinosus Tendon, BTB= Bone Patellar Tendon Bone. DIAGNOSTIC ARTHROSCOPY A standard diagnostic arthroscopy was performed for all patients throughanterolateral and anteromedial portals. Accessory posteromedial portal (Fig 1) was made for better visualisation of torn PCL and posterior wall. Associated meniscal tears were either repaired for repairable tears and partial meniscectomy done for non-repairable meniscal tears. Figure 1 Figure 2 Figure 3 Figure 4 Figure 5 Figure 6 Figure 7 Figure 1: Accessory postero medial portal made (Viewed from antero lateral portal) and cannula placed for better preparation of PCL tunnel; Figure 2: Guide Loop (GL) passed through tibial tunnel for passage of loop wire (viewed from antero lateral portal) taking care for posterior structures by pushing behind; Figure 3: A loop wire is passed through tibial tunnel and retrieved into the antero lateral portal before femoral tunnel preparation; Figure 4: Acufex PCL femoral Zig placed 8mm proximal to articular cartilage margin; Figure 5: PCL femoral tunnel reaming done by inside-outside approach from the antero medial portal; Figure 6: ACL & PCL tunnelling done with loop wire for passage of hamstring tendon grafts; Figure 7: A complete single bundle ACL & PCL reconstruction done using Semitendinosus/Gracilis Grafts
Cartilage lesions were graded and recorded. Shaving, abrading and microfracture done for grade III cartilage defects. Thorough removal of remnant torn fibres of ACL and PCL were done. The foot prints of ACL and PCL were marked using an ablator. Notchplasty was not done for our patients. TIBIAL TUNNEL PREPARATION FOR PCL The tibial tunnel position was better seen through the anterolateral and posteromedial portal. Using a special PCL zig from Acufex, zig is placed through the anteromedial portal and 2 cm below posterior tibial slope at the level of PCL origin. Using this zig and viewing through posteromedial portal will avoid use of fluoroscopy for tibial tunnel preparation. A guide wire is passed through Zig and over drilled with appropriate size of graft thickness using tibial reamers taking caution to posterior structures using a protective curette placed over the guide wire. A loop wire is then passed through the tibial tunnel using guide loop (Fig 2, Fig 3). FEMORAL TUNNEL PREPARATION All patients were fixed with Endobutton CL on femoral component. The femoral tunnel was made by an inside- outside technique. Acufex PCL femoral Zig was placed 7-8 mm proximal toarticular cartilage margin (Fig 4). A guide wire was passed from outer to inside joint. The guide wire is over reamed with 4.5mm drill for passage of the Endobutton. The length of femoral tunnel was measured. Guide wire is passed from inside the joint and exited outside the skin. With knee in slight flexion the reaming of femoral tunnel made (fig 5) from inside the joint leaving a 6mm cortex for placement of Endobutton. A loop wire which is present in antero lateral portal is then retrieved into the femoral tunnel for passage of graft. TUNNEL PREPARATION FOR ACL RECONSTRUCTION Femoral tunnel was made by transportal technique for anatomical ACL reconstruction. A guide wire is passed behind the residents ridge and over reamed with 4.5mm reamer. Length measured and reaming for graft is done by femoral reamer. Tibial tunnel was made using zig with a fixed angle of 500. Both ACL and PCL tunnelling done with loop wire present for passage of grafts (Fig 6). PCL GRAFT PASSAGE Endobutton CL is placed over prepared graft and quadrupled. The graft is then passed into tibial tunnel through loop wire. It takes an acute bend at end of tibial tunnel to enter into the notch. Care should be taken at this bend as it becomes tight on pulling from the femoral side. The graft then passes into femoral tunnel and Endobutton is fixed over the medial femoral cortex with a flip. Cycling of graft is done routinely after tensioning graft. ACL GRAFT PASSAGE The prepared ACL graft is passed through tibial tunnel and passes into femoral tunnel. The graft is then fixed with Endobutton CL on femoral end. TIBIAL FIXATION The Bio absorbable HA interference screw was used for fixation of ACL and PCL graft in tibial tunnels. For PCL fixation knee is flexedat 700 and for ACL it is flexed at 300. The screws were selected 1mm above the size of tunnel. For patients with BTB graft choice for ACL reconstruction, the femoral and tibial end were fixed with Bio absorbable HA interference screws. Arthroscopy was then performed to check graft strength (Fig 7). POSTOPERATIVE MANAGEMENT Knee is keptin hinged brace of 200-700 with a posterior support placed over the calf muscle region to avoid sagging of tibiafor 6 weeks postop.Strict non weight bearing for 6 weeks followed by partial weight bearing for 3 weeks. Knee bending was begun after 6 weeks and gradual quadriceps and hamstring strengthening exercises were taught. Patients were advised to return to normal activity at 6 months and to light sports at 9 months. Active sports involvement was allowed only after one year.
RESULT There were 12 patients with combined ACL and PCL tear included in this study. All had undergone simultaneous arthroscopic ACL and PCL reconstruction. The time duration from injury to index procedure was 6 weeks, to allow capsule, bone contusions and other soft tissues to heal. The operating time of main procedure ranges from 80 minutes to 100 minutes with a range of 87 minutes. No immediate or late complications like infections, neurovascular injury were encountered during the study. All patients were followed up at 6 weeks, 3 months, 6 months, 1 year and 2 years. The patients were assessed with IKDC score. Knee range of movements was assessed preoperatively. Out of 12 patients, 4 patients had a flexion deficit of 50& 2 patients with a flexion deficit of 200. All other patients had a normal knee flexion. At final follow up of 2 years, no patient had limitation of knee extension. For patients who underwent MCL & PLC repair done there was a flexion deficit noted at final follow up. None of the patients needed manipulation of knee joint.
DISCUSSION Knee dislocation or subluxation is one of the commonest cause of multi ligament injuries in knee joint. Road traffic accident is one of the commonest cause of knee dislocation followed by sports injuries. Roman et al.13 reported 60% out of 30 patients had injury due to road traffic accidents which is consistent with our study where 8 out of 12 patients presented with road traffic accident and 4 with sports injuries. Taylor et al.14 in their study of 26 patients of multi ligament injuries due to knee dislocation, 18 patients had good results in conservative management. However immobilisation of more than six weeks will result in knee stiffness. In 1971,Meyer’s and Harvey15 mentioned that all patients with knee dislocation treated by non-operative method had unstable and symptomatic knee at their final follow-up. Surgical management for multi ligament injuries were either through open procedure, two stage ACL & PCL reconstruction, single stage arthroscopic ACL & PCL reconstruction and collateral ligament reconstruction. Noyes and Barber-Westin16 reviewed between open versus arthroscopic approach using allograft as predominant for repair of ACL and PCL and suggested arthroscopic procedure to be better option.Mariani et al.1 reported 15 patients with multi ligament instability treated by simultaneous arthroscopic reconstruction of ACL & PCL will have a high level of efficacy and safety and to avoid major exposure with open reconstruction. The timing of surgery is significant in multi ligament injuries as damages to the medial and lateral collateral ligaments along with bicruciate ligaments, posterior capsule and neurovascular structures were expected in knee dislocations. IndelicatoPA17has observed a successful healing of interstitial collateral tears by conservative method initially for knee dislocations. It is also observed that acute MCL tears heels better with bracing and the results were on par or equal to surgical correction of MCL. However grade III valgus laxity required surgical management. It is believed that a delay in doing primary procedure of single stage arthroscopic ACL & PCL reconstruction for up to 6 weeks will allow healing of posterior capsule and posterior structures which will eventually be damaged in knee dislocations. It also decreases the incidence of arthrofibrosis.18 In our study of 12 patients, 9 had an associated medial collateral ligament injury. Out of 9 patients 5 patients had a MCL recovery from grade II to grade I laxity at 6 weeks follow-up. For 4 patients MCL repair was done with primary index procedure. One patient with a positive Dial test at 300& 900 of knee flexion and varus instability at 300flexion19,20 was diagnosed with postero lateral corner injury and a PLC reconstruction was done. At final follow-up, the Dial test was found to be negative and grade I laxity was present on varus stress. There are various choices of grafts available for multi ligament reconstruction. Allografts can be used for cruciate ligament reconstruction with a better clinical outcome, 5,6,16,21 however it is mainly used for severe soft tissue injuries in knee dislocation.Mariani et al1 proposed a Bone Patellar tendon Bone autograft for PCL reconstruction and double hamstring tendon for ACL graft for 15 patients. At final IKDC grade, 3 were graded Normal, 7 Nearly normal and 3 had abnormal result. One patient was reported to have severely abnormal grade. Strobelet al.22 reported use of hamstring tendon autograft for 17 patients with combined ACL,PCL, and PLC reconstruction. The IKDC evaluation at final follow-up was 4 normal, 10 abnormal and 2 severely abnormal grade. None had a normal IKDC grade. In our study of 12 patients the hamstring tendon autograft was used for reconstruction of ACL&PCL. The tendons were harvested from injured and uninjured leg. The four strand semitendinosus graft was used for the PCL reconstruction and a six strand gracilis tendon for reconstruction of ACL. For patients with MCL and PLC reconstruction, Patellar bone tendon bone graft was used for ACL reconstruction. Knee stiffness is the most commonly occurring morbidity in multi ligament reconstruction.23,24Mobility of knee joint is mostly sacrificed when try to achieve a good stability of knee joint. An aggressive rehabilitation protocol is necessary to achieve a good range of motion in knee along with a strong ligament construct. Two out of 12 patients in our study had a flexion deficit of 200 and4 patients with 50 flexion deficits. Shelbourne et al.25 suggested that a good preoperative knee movements will give a better outcome for multi ligament reconstruction. All our patients were given aggressive physiotherapy preoperatively before the index procedure. We followed post-operative protocol of Wascheret al.6 where has been mentioned a careful rehabilitation and post-operative management for multi ligament reconstruction. They proposed strict non weight bearing in a hinged knee brace between 200-700 for six weeks, in order to prevent the stretching of the PCL graft during rehabilitation. Knee range of motion is only allowed after six weeks and the brace is worn for 3 months postoperatively. On final evaluation of our study 10 patients had achieved good range of motion and two had a minimal extension lag of 100. No patients were manipulated and all achieved normal movements with a good rehabilitation. The final IKDC results were 8 normal grades, 3 nearly normal grades and 1 abnormal grade.
CONCLUSION 1. Multi ligament injuries are more common in knee dislocation following high velocity injury. 2. A systematic clinical evaluation and preoperative assessment is essential for its management. 3. A single stage Arthroscopic ACL & PCL reconstruction is highly recommended for multi ligament injuries. 4. Grade II MCL tear with combined ACL and PCL tear can be treated non operatively. 5. Hamstring tendon autograft is a better graft choice for the bicruciate ligament reconstruction. 6. A delay in doing the surgery will allow the healing of unnoticed capsular tear, bony contusions and other soft tissue injuries. 7. A careful and aggressive rehabilitation is absolutely necessary to achieve a good clinical outcome.
REFERENCES
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home