Official Journals By StatPerson Publication
|
Table of Content - Volume 8 Issue 3 - December 2018
Outcome of supracondylar fractures of the humerus in children treated byclosed reduction and percutaneous pinning
Anil Kumar D N1*, Bahskar Gouda2
1Assistant Professor, 2Professor and HOD, Department of Orthopaedics, Raichur Institute of Medical sciences, Raichur 584101, Karnataka. Email: anildn@gmail.com
Abstract Background and Objectives: Supracondylar fractures of humerus is the commonest injury, constitutes about 65.4% of all fractures about the elbow in children. Displaced supracondylar fracture of humerus demand great respect and challenging one to treat, since it requires accurate anatomical reduction and internal fixation to prevent complications. So in this study we reported the results of closed reduction and percutaneous pin fixation with K-wires in the displaced (Gartland’s type III) supracondylar fracture humerus in children. Methods: 30 cases of displaced (Gartland’s type III) supracondylar fractures treated by closed reduction and percutaneous pin fixation with K-wires were studied between September 2012 –August 2013 at our institution and followed for an average of 12 months. Results: In our study of 30 patients, all were closed Gartland’s type III fractures withthe mean age of 5.76 years, 18 patients sustained fracture due to fall while playing, 18 had on left side, with posteromedial displacement in 20 patients. 1 patient had associated distal end radius fracture. Majority of patients operated on 2nd day and discharged on 2nd postoperative day. 2 patient had superficial pin tract infection, 1 had cubitus varus deformity. Conclusion: This study shows that, closed reduction and percutaneous pin fixation with K-wires gives better anatomical reduction, stable fixation with minimal complications and it is most commonly accepted method for fixation of supracondylar fracture of humerus is children. Key Word: closed reduction, humerus, percutaneous pinning, supracondylar fracture
INTRODUCTION Supracondylar fracture of humerus is the commonest injury around elbow in children. It constitutes about 65.4% of all the fractures about the elbow in children. The occurrence rate increases progressively in the first five years of life to peak between 5-7 years of age1. The supracondylar fracture of humerus demand great respect in Treatment because if it is not treated properly it may give rise to many complications such as Volkmann’s ischaemic contracture, Neurovascular injury, Myositis ossificans, Stiffness of elbow and Malunion2.There is no controversy in the management of the un-displaced fractures. But various modalities of treatment have been proposed for the treatment of displaced supracondylar fractures of the humerus in children, such as closed reduction and plaster of paris slab application, skin traction, overhead skeletal traction, closed reduction and percutaneous pin fixation and open reduction with internal fixation4 Closed reduction with splint or cast immobilization and treatment with traction has traditionally been recommended for displaced supracondylar fractures, but difficulty in reduction, loss of reduction postoperatively or during follow up leads tomalunion and elbow stiffness5 .But now a lot of changes in medical field has taken place especially in orthopaedic trauma. A better understanding of bio-mechanics quality of implants, principles of internal fixation, soft tissue care antibiotics and asepsis have all contributed to the radical changes. Thus we have advanced from the conservative approach to closed reduction and percutaneous pin fixation in fractures as an acceptable mode of treatment6.Closed reduction and fixation with percutaneous Kirschner (K) wire was first described by Swenson.7He pointed out the advantage as 1) stable fixation of fracture fragment, 2) decreased risk of circulatory compromise in the form of restoration of radial pulsein nearly 90 percent of cases of brachial artery injury, and 3) a simple and cost-effective procedure. The purpose of this study was to assess the ability of closed reduction and percutaneous K-wire fixation, to obtain and maintain an adequate fixation, and to evaluate the recovery of elbow range of motion (ROM) and carrying angle.
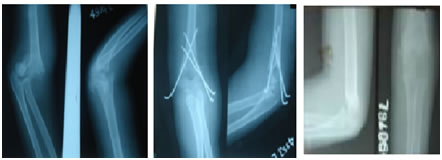
MATERIAL AND METHODS This is a prospective, observational and clinical study done at the department of Orthopedics, Raichur institute of medical sciences Raichur from September 2013 to September 2014. A total of 30 children with fractures supracondylar of humerus Grade III closedor Grade I open were included after taking informed consent. The patients were aged between 3-anda-half to 11 years with the mean age of 5.76 years.We excluded Grade I and Grade II fractures and open fractures of more than Grade I. bilateral fractures and those cases which had previous contralateral fractures around the elbow were also excluded. The time of operation ranges from the first day of injury to the eighth day of injury with the mean time of operation being4.6 days. The patients were evaluated as described by Flynn and the results compared with the contralateralnormal elbow.9 Under general anesthesia, using c-arm fluoroscopy closed reduction was done. The forearm was then pronatedand the elbow acutely flexed. Pronation de-rotates the distal fragment from its frequently medially rotated position and locks it in correct alignment.10 When satisfactory reduction had been achieved then fixation was done by two cross Kwiresof 1.5 or 2.0 mm size (Figure 2).The pins were bent and cut off outside the skin and a well-padded, above-elbow, posteriorback-slab was applied. The elbow could be held in anyposition without losing the reduction, and the optimumposition, usually 60 to 90 degrees of elbow flexion, allowed free blood flow. The patient was carefully observed for twelve to seventy-two hours (average 58hours) and then discharged. The above-elbow plaster of paris (POP) back slab was kept for four weeks and the pins and slab were removed in the out-patient (OPD) clinic. Elbow ROM was started after removing the POP back slab. The follow-up was arranged as follows: the first followupon the seventh day to inspect the wound; the second follow-up on the second week for wound inspection orsuture removal and to see the pin configuration; the third follow-up on the fourth week for the removal of plaster slab and pins and to start physiotherapy; the fourth follow-up on the eighth week post-operatively to see the ROM and carrying angle of the elbow; and the final follow-up on the fourteenth week post-operatively to see the final result of the study (Figure 3, 4). All the statistical data were analyzed with Microsoft excel.
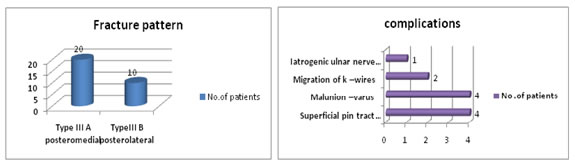
RESULTS Observation and analysis of results were done in 30 patients who were operated in our hospital in relationship to age, sex, type of injury, laterality of fracture, fracture pattern, associated injuries. Time of surgery, duration of hospital stay, complications of treatment and functional outcome. In our series majority of 15 (50%) of patients were found to be between age group of 4-6 years. The least number of cases are found in the age group between 13-15 years. The average age of the patient is 7 years. Majority of the patients were males i.e., 18 (60%) and 12(40%) patients were females. In our series the most commonest cause of injury was fall while playing 18patients, followed by fall from bicycle in 9 patients and in 3 patients it was due to fall from tree. In our clinical study we had 20 patients with posteromedial displacement and 10 patients with posterolateral displacements.
Figure: Flexion Extension Normal Carrying Angle Figure A: pre op Figure B: post op Figure C: Follow up Xray
DISCUSSIONS A supracondylar fracture of the humerus is the most common fracture of the elbow in children. Unfortunately, it can also be one of the most difficult fractures to treat. While some authors have relied on a child’s remodelling capability to compensate for inadequate reduction, most authors agree that accurate reduction with minimum joint and soft-tissue trauma is required to achieve the best possible functional result.11-13 In this study, the results of both lateral and cross pin insertion groups at eighth post-operative week showed excellent results in around seventy percent of patients. At the 14th week post operatively these excellent results were seen in more than ninety percent of the cases. We believe that this increase of range of motion of the elbow was because of the physiotherapy. Those patients who had good or fair results were having severe soft tissue injuries or repeated closed reduction performed in another center. Khan obtained 88% excellent, four percent good and four percent poor results in his study.14 Tiwari observed 88 percent satisfactory results, among which 42% were excellent, in his series of late-presenting supracondylar fractures of humerus in children.15 These two studies are comparable to our study. Cubitusvarus deformity is the most common problem seen after the treatment of supracondylar fractures. The cause of the deformity is coronal rotation, or tilting of the distal fragment.16 Some investigators believed that varus deformity is due to epiphyseal growth disturbance or rotation of the distal fragment.17 Smith suggested that residual medial tilt after reduction is the most important factor in varus angulations, with isolated rotational deformities being corrected by compensatory rotation at the shoulder.18 This concept has become popular in understanding the sequel of alteration in carrying angle.19 The incidence of postoperative nerve injury has been estimated to range from 5 to 19%.20 Culp recommends that initial observation and supportive therapy for neural injury associated with a closed, displaced, supracondylar fracture of the humerusand that if there is no clinical or electromyography evidence of return of neural function at five months after injury, exploration and neurolysis should be performed. If the nerve is in continuity, the prognosis after neurolysis is excellent.21 In the present series, two (1.2%) patients developed pin-tract infections, which were superficial and healed after removing pins and administration of oral antibiotics. No deep infection or septic arthritis was found. Pirone found superficial pin-tract infection in two percent of cases with no deep infection and septic arthritis.24 We had more pin tract infection which was probably because of poor hygienic conditions of the patient. Gordon observed pin-tractmigration in six percent of cases and Lee noticed the loss of reduction in seven percent of cases.25-26
CONCLUSIONS Closed reduction and percutaneous K-wire pinning in the management of supracondylar fractures of the humerusin children is safe as regards avoidance of vascular complications, effective in obtaining good results, and relatively economical regarding hospitalization. The disadvantage is the need for technical proficiency and the availability of c-arm fluoroscopy. There is a risk of injuring the ulnar nerve in cross pinning and this can be avoided by pinning only lateral two pins.
REFERENCES
|
|
 Home
Home