Official Journals By StatPerson Publication
|
Table of Content - Volume 9 Issue 1 - January 2019
Comparative study of outcomes in communited extracapsular fractures of hip treated with cemented bipolar arthroplasty and dynamic hip screw techniques
Zeeshan Muzahid T
Assistant Professor, Department of Orthopaedics, Bhaskar Medical College, Yenkapally(V), Moinabad(M), Ranga Reddy Dist, Telangana, INDIA. Email: zeeshanjahan0204@gmail.com
Abstract Background: Injuries like inter trochantric factures is a common problem in the elderly. The management of communited intertrochanteric fracture is challenging because of excessive collapse, loss of fixation and cut off of the lag screw resulting in poor fixation. Present study has been undertaken to evaluate the functional outcome of communited intertrochanteric fractures with cemented bipolar arthroplasty compared with dynamic hip screw fixation. Objectives: To compare the results, efficacy in meeting the activities of daily routine, functional and clinical outcomes of cemented bipolar anddynamic hip screw fixation as a treatment for comminuted intertrochanteric fractures in elderly patients. Methodology: This prospective study was conductd on 32 cases of intertrochanteric fractures of hip, 16 cases treated with cemented bipolar hemiarthroplasty and 16 cases with Dynamic Hip Screw. The cases were classified according to AO:OTA classification. Hardinge’s modification of antero: lateral approach was used for cemented bipolar cases and lateral approach was used for dynamic hip screw fixation. Pre operative care, inter operative care, post operative care & complications during follow up period were observed. Functional evaluation was done by using Haris Hip Score and data was analysed. Result and conclusion: In a present study, age group ranges for patient was from 60 to 75 years & 56.17% were male & 43.75% were female. Harris Hip Score in cemented bipolar showed 6 (37.5%) excellent, 6 (37.5%) good, 4 (25%) fair results while dynamic hip screw showed 4 (25%) excellent, 6(37.5%) good, 2(12.5%) fair and 4 (25%) poor results. Complications noted in the study of cemented bipolar were 1(6.25%) case of superficial wound infection, 4 (25%) cases of shortening and 6 (37.5%) cases of abductor weakness with Trendelenburg gait while in study of dynamic hip screw were 4(25%) cases of implant failure, 3 (18.75%) cases of non:union, 2(12.5%) cases of knee stiffness and 4 (25%) cases of varus angulation and 1(6.25%) case died due to medical reasons. This study concludes that primarily the cemented bipolar arthroplasty can be considered as one the main treatment option in communited intertrochanteric fractures in elders. Key words: cemented bipolar hemiarthroplasty, dynamic hip screw fixation , comminuted intertrochanteric fractures, fractures in elderly.
INTRODUCTION Intertrochantric fractures are very common around the world. Injuries around the hip is a common problem in the elderly. There were an estimated 1.66 million hip fractures worldwide in 19901. This worldwide annual number is rising rapidly2 with an expected incidence of 6.26 million by the year 20501,3. An increase in these fractures is on the rise due to increased life expectancy of the people and osteoporosis4,5, so intertrochanteric fracture in the elderly patients is a frequent problem. These fractures are caused generally by trivial trauma like fall in bathroom or on floor, slipping while walking. The mainstay of operative treatment options of intertrochanteric fractures are extramedullary devices like dynamic hip screw fixation and intramedullary fixation like gamma nailing and proximal femoral nailing. Stable fractures can be easily treated with osteosynthesis with predictable results. However the management of communited intertrochanteric fractures (AO/OTA type31-A2.2 and 2.3)6 is challenging because of excessive collapse, loss of fixation and cut off of the lag screw resulting in poor fixation. Osteoporosis and instability are the most important factors leading to failure of osteosynthesis7, 8 and also in these elderly patients early mobilization 9 and weight bearing can reduce complications like pneumonia, deep vein thrombosis. The fracture stability, quality of bone and early mobilization of the patient are the factors which determine the functional outcome of intertrochanteric fractures in elderly people. To allow early postoperative weight bearing and to decrease complications of osteosynthesis surgeons have recommended VDP Prosthesis10, primary Bateman Leinbach prosthesis11 or bipolar prosthetic replacement12, 13 for the treatment of communited intertrochanteric fractures in elderly people. The treatment of comminuted intertrochanteric femur fracture in elderly patients has still been a controversy and there is limited literature on prosthetic replacement of comminuted intertrochanteric fracture. So the purpose of this study is to evaluate the functional outcome of communited intertrochanteric fractures with cemented bipolar arthroplasty compared with dynamic hip screw fixation.
METHODOLOGY The present study was a prospective study comprising of 32 cases of intertrochanteric fractures of hip, 16 cases treated with hemiarthroplasty with cemented bipolar and 16 cases with Dynamic Hip Screw at Konaseema Institute of Medical Sciences Foundation, Amalapuram from August 2013 to September 2015. The cases were classified according to AO-OTA classification INCLUSION CRITERIA
EXCLUSION CRITERIA -
Before the start of the study, institutional ethics committee permission was obtained for conducting the study. Written informed consent was obtained from the patient for participating in the study after explaining the purpose of the study Preoperative treatment: On admission to the hospital, x rays were taken and immediate immobilization of fractured limb with skin/skeletal traction with about 3/5 Kg weight respectively was applied to maintain the reduction and to reduce the pain and give comfort and to prevent further soft-tissue damage. Classification was done with A0 Classification system. All routine investigations were done which were the prerequisite for preanaesthetic checkups. As operative treatment is considered, the following factors, which determine the strength of fracture-implant assembly, namely the (i) Bone quality, (ii) Fracture geometry (iii) Fracture reduction, (iv) Implant design, and (v) Implant placement were stressed upon. The anaesthesia employed was left to the anaesthetist’s choice. Local parts were shaved in the ward preoperatively two hours before the operation. Every patient had given prophylactic antibiotic of 1 gm parental ceftriaxone just before surgery. The surgery was carried out on fracture table under C arm control. Parenteral antibiotics (3rd generation cephalosporins) were given. Under epidural/spinal anaesthesia patient was kept in lateral position for hemiarthroplasty with cemented bipolar and supine position on traction table for Dynamic hip screw. Injured hip was prepared by preoperative scrubbing with povidone iodine and painted with povidone iodine solution and hip was draped under strict aseptic conditions. Operative procedure for Bipolar hemi-arthroplasty: Hardinge’s modification of antero-lateral approach has been used for cemented bipolar arthroplasty. Immediate Post-operative protocol:- Postoperatively parenteral antibiotics (3rd generation cephalosporins) were given for 3 to 5 days. Drain was removed on 2nd postoperative day. Patients were ambulated with the help of walker on 2nd to 10th postoperative day depending upon the patient health status and internal fixation. Sutures were removed on 10 th postoperative day and patients were discharged. As the patients encompassed older age and the bones were osteoporotic patients were given calcium citrate maleate and vitamin D and vitamin C supplements. None of the patients were given bisphosphonates preoperatively or postoperatively till the time of discharge. Complications: In the immediate postoperative period patients were observed for the following complications. Respiratory complications like hypostatic pneumonia Cardiovascular complications like myocardial infarction and cardiac failure in patients with hypertension and diabetes mellitus. Wound infection may be superficial or deep. The treatment of an early superficial infection was antibiotics and the removal of sutures to release wound tension and promote drainage. In deep infection, if there was presence of pus or hematoma from the wound on release of skin sutures. Debridement and removal of the implant in extreme cases was done. These complications can be less with bipolar prosthesis that are preassembled and fitted.Limb length discrepancy can occur in patients operated with cemented bipolar hemiarthroplasty. In the follow up period the patients were observed for the following complications.
Classification of heterotopic ossification was done radiologically by Bookeret Classification. Grade 0. No ossification. Grade 1. Islands of bone around the hip. Grade 2. Bone spurs from either the pelvis or proximal femur, but at least 1cm between them. Grade 3. Space between bone spurs less than 1cm. Grade 4. Callous bridging between pelvis and femur. 4. Protrusion acetabula. 5. Loosening of stem. RESULTS In the present study, 16 cases of unstable intertrochanteric fractures treated with cemented bipolar hemiarthroplasty and 16 cases were treated with Dynamic hip screw.
Table 1: Characteristics of study participants
In a present study, age group range from 60 to 75 years with mean value of 68.62 years for cemented bipolar arthroplasty and 63.37 for dynamic hip screws. Out of 16 cases 8(50%) were males and 8 (50%) females in cemented bipolar arthroplasty and 10 (62.5% ) males and 6 (37.5%) females in dynamic hip screw. Out of 16 cemented bipolar cases 4 (25%) were right and 12 (75%) were left and out of 16 dynamic hip screw cases 4(25%) were right and 12 (75%) were left. The classification used in the study was AO classification and it includes 21 (65.62%) of total cases of AO31 2.2 and 11 (34.38%) of total cases of AO 31 2.3.
Table 2: Functional evaluation with Harris hip score in study participants
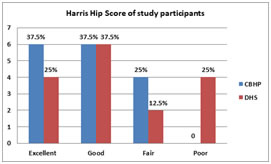
Hardinge’s modification of antero-lateral approach was used for cemented bipolar cases and lateral approach was used for dynamic hip screw fixation. Result of Harris Hip Score reflected that in cemented bipolar out of 16 cases, 6 (37.5%) were excellent, 6 (37.5%) were good, 4 (25%) were fair. In dynamic hip screw out of 16 cases 4 (25%) were excellent, 6(37.5%) were good, 2(12.5%) was fair and 4 (25%) were poor. (Fig -1)
Figure 1: Bar diagram showing Harris Hip Score in study participants Table 3: Complications observed among study participants
*Multiple complications observed in same patient.
Complications noted in the study of cemented bipolar were 1(6.25%) case of superficial wound infection, 4 (25%) cases of shortening and 6 (37.5%) cases of abductor weakness with Trendelenburg gait. Complications noted in study of dynamic hip screw were 4(25%) cases of implant failure, 3 (18.75%) cases of non-union, 2(12.5%) cases of knee stiffness and 4 (25%) cases of varus angulation and 1(6.25%) case died due to medical reasons. All the results comparing with the reported series were similar but bipolar arthroplasty provides early ambulation than DHS.
DISCUSSION Trochanteric fractures of femur are among the most common fractures encountered in orthopedic practice in the elderly. The specialty of a trochanteric fracture lies in the fact that it can be managed both conservatively and surgically. Internal fixation had the advantages of minimizing constant monitoring needed in conservative management. It also reduces the complications of prolonged immobilization like bed sores, hypostatic pneumonia and Deep vein thrombosis. In recent years trend has changed from conservative to surgical management. The mainstay of treatment options of intertrochanteric fractures are extramedullary devices like dynamic hip screw fixation and intramedullary fixation like gamma nailing and proximal femoral nailing. Union rates as high as 100% have been reported in association with well-reduced, stable fractures that were treated with ideal implant placements, failure rates of as high as 56% have been noted in association with unstable fractures, comminutions, suboptimal fracture fixations, or poor bone qualities in elderly patients with DHS15,16. The outcome of fixation depends mainly on quality of bone, age of patient, general health, trauma, surgery interval, and adequacy of treatment, co- morbidities, and stability of fixation. Holt, Dimon and Hughston, Sarmentio and William’s have done outstanding work in attempt to change an unstable intertrochanteric fracture into a stable one and fix it with an appropriate implant until it heals. Intertrochanteric fractures in elderly leads to confusion regarding treatment options osteosynthesis Vs hemiarthroplasty. In this age group the fracture configuration is generally comminuted with presence of extensive osteoporosis. So maintenance of fracture reduction which should be anatomical or near anatomical, proper positioning of the implant and monitored weight bearing are the pre-requisites to achieve good functional outcome with DHS. Osteosynthesis of such fractures may reduce the morbidity of pain. It does not permit an early mobilization with a fear of failure of fixation. The poor mechanical properties of the weak and osteoporotic bones in elderly patients do not provide a good purchase for the screws, which subsequently lead to an early biomechanical failure. This leads to collapse, with migration of the screws and the femoral head into the varus and retroversion, resulting in limping, which is caused by shortening and a decreased abductor muscle lever arm. Thus, it has become clear that walking with full weight-bearing before the fracture has healed is often impossible but early ambulation following surgeries are important, for preventing complications that can be caused by long term bed rests in elderly patients with poor general condition.The special problems associated with unstable fractures in the geriatric agegroup are possibly due to one or more of the following factors. Osteoporosis, Communition, Age related medical illnesses like Hypertension, Diabetes mellitus, Hyperlipidemia, Need for rapid mobilization, Lack of psychomotor skills for partial weight bearing. All these problems are addressed by bipolar hemiarthroplasty. Early mobilization is possible as the technique bypasses of fracture healing and provides immediate stability and mobility thereby avoiding the problems of recumbence. So to allow early post-operative weight bearing and to avoid excessive collapse at the fracture site, some surgeons have recommended bipolar prosthetic replacement for the treatment of communited osteoporotic intertrochanteric fractures. Hemiarthroplasty has been used for unstable intertrochanteric fractures since 1971, however less frequently as compared to femoral neck fracture. Its initial use was as a salvage procedure for failed pinning or other complications of Dynamic hip screw. Green S, Moore T et al12, in 1987 conducted study on 20 elderly patients (average age, 82.2 years) with unstable intertrochanteric hip fractures treated with a bipolar head-neck replacement. Seventeen patients had the prosthesis inserted as primary fracture management, and three, for salvage of failed internal fixation. The patients were ambulated with unrestricted weight-bearing at an average of 5.5 days after the operation. They have taken the greater trochanter as a landmark for precise placement of the femoral head so as to achieve correct limb length and concluded that the bipolar design may permit conversion to a total hip arthroplasty without removal of the femoral component, and may reduce the risk of acetabular cartilage damage. The earliest comparison of prosthetic replacement with internal fixation was undertaken by Haentjens et al17, The study involved 37 patients who were more than 75 years of age and operated with hemiarthroplasty with bipolar prosthesis. The results in this population were compared in a retrospective manner with 42 patients undergoing internal fixation with a blade plate. Patients treated with a cemented hemiarthroplasty were permitted immediate weight- bearing. Those patients treated with internal fixation were not allowed to bear weight fully until osseous union had occurred radiographically. The results were comparable among groups with a significant reduction in the incidence of pneumonia and pressure sores in those undergoing prosthetic replacement. This was thought to be due mainly to rapid mobilization of the prosthetic group as compared with those fixed internally. The functional results were graded according to Merle d’Aubigne and were rated as excellent to good in 75 percent of patients. In another comparison study of hemiarthroplasty versus internal fixation, Kayali et al18, observed that there were no significant differences between the 2 groups in terms of sex, age, fracture type, follow-up period, hospital stay, operating time, receipt of blood transfusions and metabolic and associated diseases. The clinical results of both groups were similar, but hemiarthroplasty patients were allowed full weight bearing significantly earlier than the internal fixation patients.10 Out of 42 patients died in first six months among cemented bipolar prosthesis and 15 out of 42 died among DHS patients. Hardy et al19studied 100 patients who had intertrochanteric fractures with compression hip screw and intramedullary hip screw. Operating time was significantly greater in intramedullary group, blood loss was lesser and perioperative complications were similar in both groups. However, there is only one study by Kim et al20 Which compares the cement Less calcar replacement prosthesis with proximal femoral nailing in a prospective study involving two groups of 29 patients. They could not find any significant difference concerning the functional outcomes, hospital stay, time to weight bearing or general complications but shorter operative time, less blood loss, fewer units of blood transfused, lower mortality rate was seen patients with proximal femoral nailing compared to cementless calcar replacement arthroplasty. The Cochrane database analysis of relevant studies concluded that there is insufficient evidence to prove that primary arthroplasty has any advantage over internal fixation. However, they also mentioned that there were only two randomized trials studied and both had methodological limitations, including an inadequate assessment of the longer term outcome21. Ahmed Elmorsy et al22, in 2011 conducted prospective study on 41 patients (22 females and 19 males—all were 65 years old or above) who had bipolar arthroplasty for unstable intertrochanteric fractures. Modified lateral approach was used in all patients. Harris Hip Score (HHS) used for clinical evaluation. Follow up period ranged from 12 to 24 months. During the last follow up, the Harris Hip Score ranged from 93 to 51 with a mean value 78.19. Four cases (9.76%) were excellent, 16 cases (39.02%) good, 16 cases (39.02%) fair and 5 cases(12.02%) poor. The complications in this study were one patient had infection, one had dislocation, one had stem subsidence, one had acetabular wear, one had intra-operative crack during insertion of femoral stem. Atul Patil et al23 conducted study on Role of Cemented Bipolar Hemiarthroplasty for Comminuted Inter-trochanteric Femur Fracture in elderly osteoporotic patients through a modified Trans trochanteric approach- “SION Hospital Modification” and observed that Mean Harris hip score at the mean follow up of 2.92 years was 80.76. In present study on 16 elderly patients with unstable intertrochanteric fracture treated with cemented bipolar hemiarthroplasty, out of which 8 were males and 8 were females. Out of them 12 had left hip fractured and 4 had right hip fractured, the average preoperative hospital stay was 9.8 days. The average age of patients was 68.62 years which was in the same age range conducted in other studieslike study conducted by Patil A et al 2013 which was 65.5 yeras. This study also targeted the same age group as in other studies. Post-operative ambulation:- The patients started ambulation with walker at an average 5.25 days after surgery (Range, 2–8 days). This is comparable with studies like K.H.Sancheti et al(4.2), Nikunjmaru et al (4.2)days, G.Kirankumar (5.4) days of mean period of ambulation. Postoperative ambulation is the main important one that differs with the studies on internal fixation of intertrochanteric fractures, thus it has become clear that walking with full weight-bearing before the fracture has healed is often impossible in factures that are fixed but early ambulation following surgeries are important, for preventing complications that can be caused by long term bed rests in elderly patients with poor general conditions. So in present study we allowed the patients to ambulate post operatively between 2 to 8 days with mean value of 5.25days depending on patient general condition of the patient post operatively. Harris Hip Score:- At 6 months follow-up 6 patients (37.5%) were graded as excellent, 6 patients (37.5%) as good, 4 (25%) as fair is comparable to studies like K.H.Sancheti et al who had out of 37 patients 7(19.4%) had excellent results, 16(44.4%) had good results and 9(25%) had fair results and 2(5%) had poor results and also Nikunjmaru et al. Out of 28 patients 11(39.2%) had excellent, 10(35.7%) good , 4(14.2%) fair and 2 poor results. At last follow-up, 6patients were walking without any aid, 1patient used a stick for walking (patient was using stick for psychological support). Shortening:- Four patients had shortening of more than 1cm of the operated limb in present study. In studies by Atul patil et al 8 out of 126 patients and K.H.Sancheti et al 10 out of 37 patients and Nikunj Maru et al 5 out of 28 had limb shortening of an average of 1.1cm . Trendelenberg gait:- In present study , out of 16, 6 patients had abductor muscle weakness with a positive Trendelenburg test and Trendelenburg gait at final follow-up. Blood transfusion:- Six out of 16 patients had blood transfusion. Total of 9 units of whole blood were transfused to 6 patients. Complications- There was one case of superficial infection which settled with two weeks course of intravenous antibiotics, and no deep infections in the present study. One case of superficial infections was seen in studies by Nikunjmaru and K.H.Sancheti. 2 cases of superficial infection were seen in studies by Atul patil et al. Stern and Angerman reported a deep infection rate of 2.8%but made no comments on dislocations. There were no cases of heterotrophic ossificaation.KH Sancheti et al. reported heterotrophic ossification at 6-month follow up; however, this did not restrict the range of motion. In two patients there was failure of tension band wiring of greater trochanter in our study. In studies done by Osman Rodop there were 2 cases of failure of tension band wiring and in Atul patil et al there were 2 cases of failure of greater trochanter tension band wiring. There were no dislocation, loosening, late infections, heterotrophic ossification, protrusion acetabuli, implant breakage in this present study. In this study 16 patients with intertrochanteric fractures were treated surgically by means of a Dynamic Hip Screw. Age group: The average age group of the study group was 63.37 years. This is comparable to that quoted by most authors in literature (62.5 years. by Murray and Frew, 62.2 years. by Evans). The average preoperative stay in hospital was 8.4days. Sex: In the present study there is a male preponderance. Ten (62.5%) of the 16 Patients operated on were males. This is in contrast to the studies done in western world where there was a female preponderance in study conducted by Hornby and Grimley Evans 1989 - 82% were females. This is probably because in India, males are engaged in more strenuous activities compared to females who have a sedentary life. Blood transfusion: 5 out of 16 patients had blood transfusion. Total 9 units of blood were transfused to 5 patients. Harris Hip Score:-In the present study functional and anatomical results were graded according to Harris Hip Score criteria as excellent, good, fair and poor. Four out of the 16 patients (25%) had an excellent result. These patients had sound union both clinically and radiologically within 3 months. None of these patients had Varus deformity or shortening. In 6 patients (37. 5%) the result was good. These patients had painless mild limp with negligible shortening and walked independently 2-3 months after surgery. Four patients (25%) had an outcome which was graded as fair. Out of theses 4 patients, 3 (18.75%) had no radiological union after 12 months and 2 patients had knee stiffness and the knee was in functional position and was able to walk with an assistance of a stick. This is almost similar to the incidence of stiffness by conservative management like 4% Murray and Frew series. Four patients had implant failure, four patients had extrusion of the compression screw and varus angulations. Two cases of which showed no radiological union, extrusion of screw and Varus angulation after 6 months of follow up with DHS. Another two cases showed extrusion of compression screw.
CONCLUSION The present study, reflected that primary cemented bipolar hemiarthroplasty in communited intertrochanteric fractures in elderly patients provides painless stable joint allowing the patients to ambulate early in the post-operative period minimizing the complications associated with prolonged recumbency. The results of dynamic hip screw were inferior when compared to cemented bipolar hemiarthroplasty for communited intertrochanteric fractures . This study concludes that primarily the cemented bipolar arthroplasty can be considered as one the main treatment option in communited intertrochanteric fractures in elders. Limitations of study - The study comprises few number of patients. Recommendations:-Cemented bipolar arthroplasty gives better results, early mobilization of patients, less implant failure and complications as compared to DHS. The study comprises only few patients so there is need for a large study with more number of subjects.
REFERENCES
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home