Official Journals By StatPerson Publication
|
Table of Content - Volume 9 Issue 2 - February 2019
Functional outcome of distal humerus fractures treated with an extensor mechanism sparing Paratricipital approach
Rajesh K Ambulgekar1, Kapil R Saoji2*
1Professor and Head, 2IIIrd year Resident, Department of Orthopaedics, Dr Shankarrao Chavan Government College and Hospital Nanded, Maharashtra, INDIA.
Abstract Background: Management of distal humerus fracture in adult often poses a challenge to even the most experienced surgeon. The paratricipital approach have several advantages, complications of olecranon osteotomy can be avoided, triceps tendon insertion not disrupted, allows early range of motion. Aim: To evaluate the functional outcome of fracture of distal humerus in adults by extensor mechanism sparing paratricipital approach. Material and Methods: A hospital based prospective study was done with 30 patients of fracture of distal humerus in adults treated with open reduction and internal fixation with bicolumnar plating by extensor mechanism sparing paratricipital approach. Patients were followed up post-operatively at 1 month, 2 months, 6 months after treatment and were evaluated clinically by Mayo Elbow Performance Score. Results: The mean range of motion was improved over 6 months follow up. At the end of 6 month follow up as per Mayo Elbow Performance Score, excellent result was found in 26 patients, good result in 3 patient and fair in one patient. Using Mayo elbow score we had more than 96% excellent to good results with mean score of 95.46. Conclusion: Extensor Mechanism sparing paratricipital approach preserves triceps and extensor mechanism thus it helps in early mobilization gives better functional range of motion and therefore better functional outcome. Key Word: Distal humerus fractures, Extensor Mechanism sparing paratricipital approach, Mayo Elbow Performance Score, functional outcome
INTRODUCTION Distal humerus fracture in adult often poses a challenge to even the most experienced surgeon. The surgeon is technically demanding an adequate exposure of the distal humerus articular surface is important for the surgery. The fixed olecranon and triceps tendon limit direct visualization of elbow joint. Multiple exposures such as olecranon osteotomy approach and dissociation of the triceps from the olecranon have been described to address this limitation. But these are not free of complications and that complications necessitate more surgery and predispose to infections.1 To avoid these complications an extensor mechanism sparing paratricipital posterior approach to Distal Humerus through midline posterior incision was suggested by Schildhauer et al.2 The paratricipital approach have several advantages, complications of olecranon osteotomy can be avoided, triceps tendon insertion not disrupted, allows early range of motion. This approach also preserves innervations and blood supply of anconeus muscle3,4 which provides dynamic postero-lateral stability of elbow. Finally, if further exposure require paratricipital approach can be converted to olecranon osteotomy and if further proximal exposure is required for associated fractures shaft humerus, lateral side paratricipital approach can be converted into Gerwin et al approach.5 The purpose of this study was to evaluate the functional outcome of fracture of distal humerus in adults treated with open reduction and internal fixation with bicolumnar plating by extensor mechanism sparing paratricipital approach.
MATERIAL AND METHODS This prospective study was conducted in Department of Orthopedics of a Tertiary care hospital over a period of two years. All patients with distal end humerus fracture were screened using the inclusion and exclusion criteria. Informed consent was taken for all patients willing to undergo the trial were included. Approval of the Institutional Review Board was obtained prior to the commencement of the study. Inclusion Criteria
Exclusion Criteria
METHODOLOGY Detailed history was taken from the patient regarding the etiology of the fracture, associated injuries, general examination, physical examination of the corresponding shoulder, elbow and wrist joints was carried out. Investigations were done in the form of elbow X-rays (AP and lateral views; both oblique views if required) and were evaluated. Fractures were classified based on the AO classification. Primary management was done and fracture immobilization in above elbow slab upto mid-arm level and the patient was shifted to ward with elevation of the affected upper limb. Patients included in the study were treated with open reduction and internal fixation with bi-columnar plating by Extensor Mechanism sparing paratricipital approach, and were assessed intra-operatively for blood loss, fracture reduction and articular continuity under the image intensifier (C-arm). Operative technique: The patient was taken up for surgery after regional/general anaesthesia. Lateral decubitus position was given with arm supported and forearm hanging. The standard midline postero-medial approach was taken with incision beginning 1 cm distal to the tip of the olecranon and extending proximally in the arm up to 8 cm above the tip of the olecranon.After skin incision, the subcutaneous tissue was dissected and firstly ulnar nerve was identified and dissected from surrounding soft tissue and fascia proximally along the medial border of the triceps and released from the cubital tunnel distally, through the flexor pronator aponeurosis to the level of its first anterior motor branch. The ulnar nerve was retracted using feeding tube which was placed around it and protected throughout the entire procedure. Once the ulnar nerve was secured, medially the triceps was dissected and separated from subcutaneous tissue and medial intermuscular septum. Similarly, on lateral side, it was dissected and separated from subcutaneous tissue and lateral intermuscular septum. The interval between the triceps and anconeus muscles was incised to expose the joint. Finally, whole of the distal half of the triceps bulk was elevated off the posterior surface of distal humerus with the help of deep muscle retractor and supracondylar and intercondylar area was exposed along with the elbow joint. Attention was first directed toward the intercondylar area with special focus on articular continuity when fracture was having Intercondylar and intra-articular extension. The articular continuity could be assessed under direct vision on full flexion of the elbow joint or C arm image intensifier. The fracture sites were cleared of clotted blood and infolded soft tissue, and the fragments were gently reduced back into anatomic position, with care to avoid the fragmentation. Kirschner wires and guide wires were useful here, both for manipulating the small fragments and for temporary fixation. reducing and securely fixing the articular fragments. After reduction of articular fragments, temporary fixation was done with insertion of a guide wire through both the condyles under C-arm image intensifier. Cannulated drill bit was drilled over the intercondylar guide wire and 4mm cannulated cancellous screw was inserted over the guide wire to fix the distal articular fragments. Now the reconstructed major distal fragment chunk was reduced to the medial and lateral pillars and was temporarily fixed with multiple K-wires. If the fracture was only extra-articular and there was no intercondylar extension, then the fragments were reduced and directly fixed using K-wires for temporary stabilization till further fixation was done. After preliminary fixation with K-wires, reduction was confirmed under Image intensifier. Once the reduction was found satisfactory, medial and lateral pillars were fixed with two plates placed at right angle to each other. After fixation the elbow was put through the range of motion flexion and extension to test the stability of fixation. Haemostasis was achieved and a negative suction drain kept in situ and closure was done in layers. Pressure bandage was applied using crepe bandage. Patient was shifted to the recovery room. Patients were followed up post-operatively at 1 month, 2 months, 6 months after treatment, and were evaluated clinically by Mayo Elbow Performance Score at each follow-up visit, along with X-rays (AP and lateral views). Secondary outcome measures used consisted of Elbow pain, Active and passive ROM (flexion, extension) of both elbow joints using a universal goniometer, Disability in performing daily activity and Complications (infection, neurovascular compromise, stiffness, subsequent or secondary intervention, arthritis). X-rays (antero-posterior and lateral views) were evaluated on every follow up for the signs of fracture healing and hardware failure or any other complications. Union was defined as the presence of bridging callus or the disappearance of the fracture line on three of four cortices seen on the anteroposterior and lateral radiographs.
RESULTS Majority of case i.e., 56.67 were in the age group of >30 years. The mean age of the patients in the study was 38.77 years. Males were more common patients with intercondylar humerus fracture accounts for 56.67% of the cases. Road traffic accidents accounted for nearly 60% of the cases as a cause. Right side had a marginal high predominance than Left side. Majority of the cases studied were type A2 (30%) followed by type A3 (20%) supracondylar humerus fracture.
Table 1: Elbow range of movements
By using paired t-test, p-value was <0.001. Therefore, there was highly statistical significant difference between mean ROM at postoperative day - 1 to 1 month, 1 month to 2 month and 2 month to 6 month.
Table 2: Mayo elbow performance score (MEPS)
By using paired t-test p-value was <0.001. Therefore, there was highly significant difference between mean MEPS at POD 1 to 1 month, 1 month to 2 months, 2 months to 6 months. Table 3: MEPS score
Table 4: Comparison of functional outcome with various studies
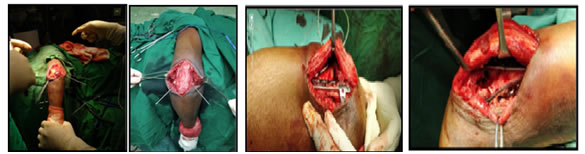
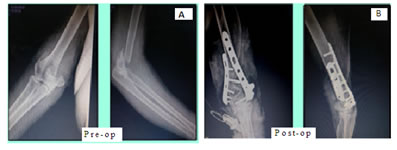
Figure 1 Figure 2 Figure 3 Figure 1: Temporary stabilization using K-wires; Figure 2: The lateral column plate- placed posteriorly curving around the capitulum and lateral condyle; Figure 3: The medial column plate – placed over medial surface of the medial pillar Figure 4: AP and Lateral view X-ray (A) Pre-op (B) Post-op
Figure 5: Follow up after 6 months
Figure 6: AP and Lateral view X-ray a. Pre-op b. Post-op Figure 7: Follow up after 6 months DISCUSSION In our study, 30 patients with distal humerus fractures were treated with open reduction and internal fixation with bicolumnar plates using extensor mechanism sparing paratricipital approach. In our study, we used Mayo Elbow Performance Score for functional outcome. At the end of 6 month follow up, we found excellent result in 26 patients, good result in 3 patient and fair result in 1 patient. Using Mayo elbow score we had more than 96% excellent to good results with mean score of 95.46. We did not have any poor results at the end of 6 month follow up. Since, we could achieve good reduction, stable fracture construct, early rehabilitation we were able to get functional range of motion of 94-166 degrees in most of the patients, and thus our functional outcome measures were also good. At the end of 6 month follow up in our study, the mean range of motion of elbow was 141.5 degree (94-166°). In our study we found that there is significant difference between mean ROM at POD 1 to 1 month, 1 month to 2 month and 2 month to 6 month follow up. In the study of Mondal J et al,9 the median arc of elbow motion was 115 degrees (range 70 to 140 degrees) with standard deviation of 1.33. Arc of motion >120 degrees seen in 66.66% of patients, arc 90-120 degrees present in 23.33% of cases, arc <90 degrees seen in 10% of cases. In the study of Patel J et al,7 24(60%) patients could move their elbow with an arc of 50-100 degrees and 4(10%) patients could move their elbow with an arc of less than 50 degrees, 12(30%) patients could move their elbow with an arc of more than 100 degrees. In the study of Yadav V et al,8 mean motion arc was 114.92°(range 65°-140°). In the study of ErpeldingJM et al,10 the median arc of elbow motion was 126 degrees (range, 60 to 141 degrees).
CONCLUSION Extensor Mechanism sparing paratricipital approach is a better alternative for Fracture of Distal Humerus in adults. It preserves triceps and extensor mechanism thus it helps in early mobilization. Bicolumnar Plating by Extensor Mechanism sparing paratricipital approach gives better functional range of motion and therefore better functional outcome.
REFERENCES
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home