Official Journals By StatPerson Publication
|
Table of Content - Volume 9 Issue 2 - February 2019
Management of lateral end clavicle fractures using clavicle hook plate vs lateral clavicle locking plate: A comparative study
Sujana Theja J S1*, B Gurumurthy2, Pavankumar Patted3
1,2Assistant Professor, 3Junior Resident, Department of Orthopaedics, JSS Medical College, JSS Academy Of Higher Education and Research, Mysuru, Karnataka, INDIA. Email: drsujantheja@gmail.com
Abstract Background: The study was conducted to compare the functional outcome of clavicular hook plate and lateral clavicle locking plate for displaced lateral end clavicle fractures using Constant Murley score. Materials and methods: This study include total of 30 cases with displaced lateral end clavicle fractures satisfying the inclusion criteria treated with lateral clavicle locking plate (15cases) and clavicle hook plate (15 cases). Patients were followed up at 1st month, 2nd month and 6th month, the functional outcome was assessed using Constant Murley score and the radiological outcome was also assessed. Results: In our study, 15 cases treated with clavicle hook plate had better results than 15 cases treated by lateral clavicle locking plate in terms of fracture union, Constant Murley score, range of movements. At the final follow-up of 6 months, excellent outcome was seen in 26.7% of patients treated with hook plate as compared to 6.7% of patients treated with lateral clavicle locking plate. Conclusion: Both hook plate and locking plate have a good functional outcome for lateral end clavicle fractures. Addressing the coracoclavicular ligaments in case of lateral locking plate is of utmost importance in comminuted lateral end clavicle fractures. Hook plate is an absolute indication for comminuted lateral end clavicle fractures. Hook plate has implant-related complications, hence implant removal at earliest is advisable. Key Word: lateral end clavicle fracture, clavicle hook plate, lateral clavicle locking plate, subacromial osteolysis, acromioclavicular joint dislocation, clavicle fracture
INTRODUCTION Fractures of the clavicle are common injuries with an incidence of 29 per 100,000 population per year.1 It accounts for 2.6–4% of the total adult fractures. Lateral end fracture constitutes 21–28% of all clavicle fractures. Of these 10–52% are displaced fractures.2 While minimally displaced fractures of the lateral end of the clavicle can be managed non-operatively with good clinical outcome, displaced fractures of the lateral end of clavicle have a higher rate of non-union.3High incidence of non-union may be due to the loss of coracoclavicular ligamentous restraint on the medial fragment, muscle forces, and soft tissue interposition between the fracture fragments. Therefore, operative management is preferred for most displaced fractures. There is a wide variety of surgical techniques for the treatment for these fractures. If surgery of lateral end clavicle fractures is indicated, many implants or surgical methods are available, including Kirschner wires, coracoclavicular screw fixation, hook plate fixation, or lateral clavicle locking plate fixation. Although there are many types of operative procedures, no procedures are considered to be the gold standard treatment. The optimal treatment of unstable lateral clavicle fractures is still controversial. Unstable lateral end clavicle fractures often require open reduction and internal fixation.1 The use of a pre-contoured superiorly placed lateral clavicle locking plate and screws, for the lateral end of the clavicle, is a recent development. It is advocated as a satisfactory technique for fixation of displaced fractures of the lateral end clavicle due to good results seen with this fixation.1 High rate of union(95% or higher) and good shoulder function have been reported with use of hook plates, but patient discomfort and acromial osteolysis generally require plate removal as soon as union occurs.4 The purpose of this study is to compare and review the clinical outcomes between the lateral clavicle locking plate and clavicle hook plate in the treatment of unstable lateral end clavicle fractures; moreover, the relevant literature of the two fixation methods will be reviewed systematically to identify the non-union, complications, or functional scores, according to the treatment methods and determine which treatment method is better. The present study compares the functional outcome of clavicular hook plate and clavicular locking plate for displaced lateral end clavicle fractures using Constant Murley score.
MATERIALS AND METHODS 30 cases with lateral end clavicle fractures admitted in JSS Hospital in a period of September 2016 to April 2018 satisfying the inclusion criteria who were treated with lateral clavicle locking plate (15 cases) and clavicle hook plate (15 cases) were enrolled in this study using computer-generatedrandom number. Inclusion criteria
Exclusion criteria
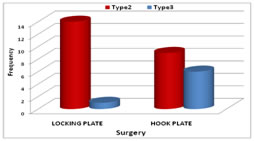
RESULTS There were total of 30 patients, among them 25(83.3%) were male and 5(16.7%) were female. Right sided lateral end clavicle fracture was seen in 18(60%) and left in 12(40%) patients. Road traffic accidents was the cause of trauma in 22 (73.3%) and fall in 8(26.7%). 23(76.7%) patients were type 2 Neer’s fracture and 7(23.3%) were type 3 Neer’s fractures. 14(46.7%) patients were less than 40 years of age ,8(26.7%) patients were of 40-50 years and 8(26.7%) patients were more than 50 years. Lateral clavicle locking plate was performed in 14(93.3%) Neer’s type2 patients and 1(6.7%) Neer’s type 3 patients. Hook plate was performed in 9(60%) Neer’s type 2 patients and 6(40%) Neer’s type 3 patients.
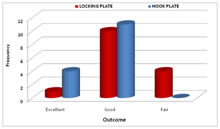
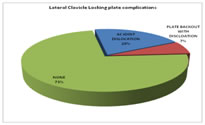
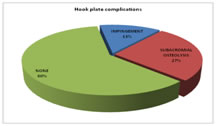
Constant murley score excellent outcome was seen in 1(6.7%) of Lateral clavicle locking plate group and 4(26.7%) of Hook plate group. Good outcome was seen in 10(66.7%) of Lateral clavicle locking plate group and 11(73.3%) of Hook plate group. Fair outcome was seen in 4 (26.7%) of Lateral clavicle locking plate group and there were no patients of Hook plate group. The mean duration of fracture union was 13.3 weeks in Lateral clavicle locking plate group and 12.6 weeks in hook plate group. In the Lateral clavicle locking plate group 3(20%) patients had Acromioclavicular dislocation and 1(7%) patient had Plate backout with dislocation. In the Hook plate group 2(13.3%) patients had impingement and 4(26.7%) patients had subacromial osteolysis. CASE 1

CASE 2
 CASE 3
 DISCUSSION The use of a hook plate in the treatment of fractures of the lateral end of the clavicle is shown to be a good and acceptable treatment option.6 In our study also, we found that hook plate had 100% union and 26.7% had excellent outcome 73.3% had a good outcome which was comparable to the above study. In regards to the use of a hook plate, there are debatable statements regarding retaining the implant for a more longer duration as against removal when the patient is symptomatic.37 In our study, we found that 40% of patients had implant-related complications, but the functional outcome was good to excellent outcome in 100% patients. Most of the patients in this study had an excellent or good outcome which is similar to the findings of various other studies.8,9,10 There is literature questioning the need for either simultaneous reconstruction or repair of the ligaments along with hook plate method of fixation, further suggesting implant removal after radiological or clinical indication and /or reconstruction after plate removal depending on the instability.11In our study, we did not reconstruct the ligaments,5 patients had an excellent outcome as assessed by Constant score. These results are comparable to other studies using a hook plate.12 We have noted the following complications: impingement occurred in 2 patients and osteolysis at the tip of the hook in 4 patients. These results are comparable with other studies.13 The presence of osteolysis between the plate and the acromion has been attributed to the rotational movement (micro motion) which occurs with shoulder movements resulting in rotation of clavicle and the hook plate in respect to the acromion.14 Senthil Loganathan concluded that there is a variation in the anatomy of the acromion in different ethnic groups. Hence a uniform sized hook plate will be inappropriate. A smaller hook depth is needed in South Asian population to prevent impingement and Intraoperatively distance between the acromion and supraspinatus tendon should be measured using depth gauge.15In our study, we found that, in comminuted fracture the placement of the screws for each fragment in lateral end locking plate was difficult, whereas hook plate did well in presence of comminution. In a meta-analysis by Stegeman et al. the hook plate and other fixation methods in the treatment of fracture were compared. There was no difference between the hook plate and other methods with respect to functional results and time to union. But the hook plate fixation was associated with an 11-foldincreased risk of major complications compared to intramedullary fixation and a 24-fold increased risk compared to suture anchoring.16 In our study we found that the hook plate had a 40% of implant-related complication which was similar to above study. Shin et al. reported satisfactory clinical outcomes and high union rates using anatomic clavicle LCP fixation in patients with unstable distal clavicle fractures, even when the lateral fragment was small. They tried to insert more than 4 small screws in the distal fragment to achieve secure fixation. Even though the aim of open reduction and internal fixation is to obtain absolute stability, it is challenging to achieve in cases of unstable distal-third clavicle fractures, particularly in comminuted distal fragments. In some comminuted fracture cases, it is difficult to insert even 2 distal screws. Although recent studies have demonstrated satisfactory clinical and radiologic outcomes after treating Neer type II distal clavicle fracture using anatomic clavicle LCP, we thought that it would be difficult to control the force of the trapezius pulling on the proximal fragment superiorly if we could not insert enough screws in the distal fragment with anatomic clavicle LCP. Therefore, we hypothesized that the AO hook LCP could be an alternative option. Although there is no consensus as to a “gold standard” fixation method for Neer type II distal clavicle fractures, we obtained satisfactory outcomes using the AO hook LCP, despite not repairing or augmenting the coracoclavicular ligament. The favourable outcomes of this study may be due to the traits of the AO hook LCP. Just as in cases of acromioclavicular joint dislocation, this plate does not compress the fracture site firmly but instead works like a lever arm to maintain the level and alignment between the distal fragment and the proximal fragment, which may have migrated superiorly.17. Fleming et al. reviewed 19 patients who underwent surgery with superior pre-countered locking plates for displaced distal-third clavicle fractures18. All patients achieved union by 4 months and no plates have been removed. In our study also, the mean union time was same around 13.3 weeks or 4 months. The rate of union in the present study were similar to other studies by Robinson et al.19, and Rokito et al.20 In the study conducted by Klein et al. for locking plates, had a high union rate (near 100% overall) and relatively few complications. Of 64 total patients, there were five reported complications, including two infections, two occurrences of screw loosening, and one malunion.21In our study we found that one patient had hardware problem and there was need to remove implant after surgery. Our results compare favorably with these studies in terms of union rates, function. In a study conducted by Qureshi et al. for locking plates, had a union rate of 97.7% and constant murley score excellent to good outcome of 73% patients.22 In our study there was 100% union and constant murley score excellent to good outcome in 73% patients which was comparable to the above study.
CONCLUSION From the analysis of this study the following were noted:
REFERENCES
|
|
 Home
Home