Correlation of serum bilirubin level by transcutaneous blood and conventional blood sample
Prakhar Mohniya1*, Prashant Shah2, C D Aundhakar3, Amit Galgali4
1Senior Resident, SNMC, Agra, Uttar Pradesh, INDIA.
2Assistant Professor, 3Professor, Department of Pediatrics, Krishna Institute of Medical Science, Karad, Maharashtra, INDIA.
4Junior Consultant Health Care Global, Bangalore, Karnataka, INDIA.
Email: shrutishah024@gmail.com, prakharmohniya@gmail.com
Abstract Background: Neonatal hyperbilirubinemia is a known, treatable risk factor for bilirubin encephalopathy, and is detectable by several methods. Universal pre-discharge newborn screening for hyperbilirubinemia has been proposed as a method to screen for risk of developing chronic bilirubin encephalopathy. Aim: To correlate serum bilirubin level by transcutaneous blood and conventional blood sample. Material and Methods: Results: Cord blood Bilirubin level of ≥1.78 mg/dl was taken as cut off value based on the receiver operating characteristic (ROC) curve where it gives best sensitivity and specificity simultaneously. On 3rd day, 5th day and 7th day bilirubin value by both TCB methods are positively correlated with conventional serum Bilirubin value. However, on day 3 and day 7 TCB forehead value had stronger correlation with serum blood than TCB sternum value while on day 5 TCB sternum value had stronger correlation with serum blood than TCB forehead. Conclusion: Trancutaneous bilirubinometer was effective in the estimation of serum bilirubin in term neonates. However, due to insufficient evidence to show the effectiveness of transcutaneous bilirubinomter in preterm neonates, serum bilirubin levels should be confirmed with chemistry analyzer.
Key Word: Neonatal hyperbilirubinemia, serum bilirubin level, transcutaneous blood, conventional blood
INTRODUCTION
Neonatal hyperbilirubinemia is a common problem encountered in the newborn babies. It commonly occurs in approximately 65% of all full term babies with the peak bilirubin levels occurring on day 5 of life.1 Because neonatal hyperbilirubinemia is a known, treatable risk factor for bilirubin encephalopathy, and is detectable by several methods, universal pre-discharge newborn screening for hyperbilirubinemia has been proposed as a method to screen for risk of developing chronic bilirubin encephalopathy. In 2004, the American Academy of Pediatrics (AAP) published updated guidelines on screening and management of neonatal hyperbilirubinemia which emphasized assessing newborns for risk of subsequent hyperbilirubinemia by examination, transcutaneous bilirubin (TcB) or total serum bilirubin (TSB) screening in the nursery; evaluation of the risk of subsequent hyperbilirubinemia with a nomogram standardized to age in hours; and revised treatment guidelines, based upon consensus and limited evidence.2 Various methods have been developed to aid non-invasive diagnosis of hyperbilirubinemia and total serum bilirubin. Transcutaneous bilirubinometers can serve as a screening tool, especially where services of a neonatologist are not available. This can be very helpful in the community or peripheral health setup for the grass root level workers to screen neonatal hyperbilirubinemia. The present study was conducted to correlate serum bilirubin level by transcutaneous blood and conventional blood sample.
MATERIAL AND METHODS
In this cross-sectional study, a total of 200 full term normal neonates delivered in hospital over a period of two years were included. Patients were included in the study after taking the voluntary informed consent of their parents. The random selection of the cases who met the inclusion criteria were done by tossing a coin. If the head comes, then that participant was included in the study. Both the genders were included in the study.
Inclusion criteria
- All full term normal newborn babies delivered in hospital
Exclusion criteria
- Babies with haemolytic disorders like Rh iso-immunization and ABO incompatibility
- Preterm and IUGR babies
- Babies of mother with bad obstetric history
Umbilical cord mixed blood samples was collected in a sterile container drawn from placental side of the umbilical cord incised while severing it at the time of birth of the baby. The mother’s age, parity, residence, community, blood pressure, diabetes, use of iodine antiseptics on the mother prior to delivery will be recorded. The type of medications/anesthesia given including doses used, duration of anesthesia given to the mother till birth of the baby were recorded. At birth, the babies weight, sex, time to first cry, congenital abnormalities, Apgar scores was noted. Bilirubin was estimated within 24 hours by laboratory investigation, again blood sample was collected in sterile container on day 3, day 5 and day 7 by all aseptic means and serum bilirubin of particular day was also recorded by non-invasive hand held Trans-cutaneous bilirubinometer from Drager JM-103 for the comparison with its lab value.
Ethical issues: The study was commenced after approval from the Scientific and Ethical Committee of the Institution. All the participant’s parents were also informed about the study procedure and the information required from them for the study. A voluntary informed written consent was taken from the participant’s parents those who consented were included in the study.
Statistical Analysis: Data management and analysis was done using Microsoft excel and Epi-info software. The categorical variables were assessed using Pearson Chi-square. Sensitivity, specificity, positive predictive value, negative predictive value was assessed and the study subjects were compared using suitable statistical tests.
RESULTS
Out of 200 neonates, 90 (45%) were female child while 110 (55%) were male child, with female to male sex ratio of 0.81:1.Before the completion of the study, 18 (9%) neonates lost to follow up. They were not turned up for follow up visit. Total 137 (68.5%) children were discharged to home while 45 neonates were found with hyperbilirubinemia during study period and were admitted in the NICU for phototherapy.
Table 1: Test Result Variable(s): S. Bilirubin mg/dl at birth of CB
Cord Blood Bilirubin level |
Sensitivity |
Specificity |
Area under curve (AUC) |
PPV |
NPV |
Std. Error |
P value |
≥1.78 mg/dl |
91.9% |
84.6% |
0.918 |
83.4 |
91.1 |
.022 |
<0.001 |
Cord blood Bilirubin level of ≥1.78 mg/dl was taken as cut off value based on the receiver operating characteristic (ROC) curve where it gives best sensitivity and specificity simultaneously. Cord blood was taken for each case. The mean level of bilirubin was 1.75 mg/dl with standard deviation of 0.54. Cord blood bilirubin level was divided in to ‘Less than 1.78 or mg/dl’ and ‘1.78 mg/dl or more’. There were 113 (56.5%) cases having S. bilirubin less than 1.78 mg/dl while remaining had level 1.78 or more. At day three based on the serum Bilirubin level 43 (21.5%) neonate had hyperbilirubunemis while remaining 157 (78.5%) Bilirubin level within normal limit.
Table 2: Comparison of cord blood Bilirubin level and neonatal day 3 hyperbilirubinemia
S. Bilirubin Cord Blood |
S. Bilirubin Day 3 |
|
|
< 17 mg/dl |
% |
≥17mg/dl |
% |
Total |
P value |
less than 1.78 or mg/dl |
103 |
65.6% |
10 |
23.3% |
113 |
<0.001 |
1.78 mg/dl or more |
54 |
34.4% |
33 |
76.7% |
87 |
|
Total |
157 |
100.0% |
43 |
100.0% |
200 |
|
P value calculated using chi square test
As shown in above table, in normal Bilirubin group 65.5% had cord blood Bilirubin less that 1.78mg/dl while in hyperbilirubinemia group 23.3% had blood Bilirubin less that 1.78mg/dl. This difference was statistically significant (p<0.01). Transcutaneous Bilirubin level over forehead and sternum taken at different interval were compared with total serum Bilirubin level taken at the same time. A scattered diagram was drawn with trend line to compare results.
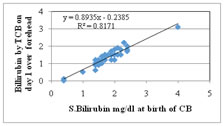
Figure 1: Comparison of TCB over forehead at day 1 with cord blood Bilirubin
On the first day, bilirubin value by TCB over forehead and sternum both methods were positively correlated with cord blood Bilirubin value with r2 value over 0.8 indicating strong linear correlation.
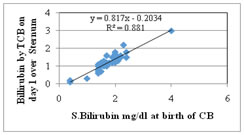
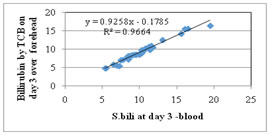
Figure 2: Comparison of TCB over sternum at day 1 with cord blood Bilirubin; Figure 3: Comparison of TCB over forehead with S. Bilirubin at day 3
On the third day Bilirubin value by both TCB methods were positively correlated with conventional serum Bilirubin value with r2 value more than 0.95 indicating strong linear correlation.
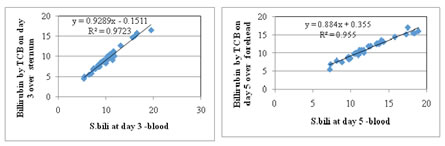
Figure 4: Comparison of TCB over sternum with S. Bilirubin at day 3; Figure 5: Comparison of TCB over forehead with S. Bilirubin at day 5
On the fifth day Bilirubin value by both TCB methods were positively correlated with conventional serum Bilirubin value with r2 value 0.95 indicating strong linear correlation.
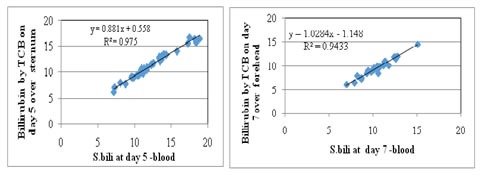
Figure 6: Comparison of TCB over sternum with S. Bilirubin at day 5; Figure 7: Comparison of TCB over forehead with S. Bilirubin at day 7
On the seventh day Bilirubin value by both TCB methods were positively correlated with conventional serum Bilirubin value with r2 value 0.9 indicating strong linear correlation.
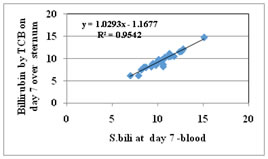
Figure 8: Comparison of TCB over sternum with S. Bilirubin at day 7
The efficacy of Trans cutaneous Bilirubin level was measure to diagnose hyperbilirubinemia in normal neonate. The present study investigated the transcutaneous Bilirubin over sternum and forehead and the total cord bilirubin measurement by a direct spectrophotometric method in the laboratory. Transcutaneous bilirubin over forehead as well as over sternum both showed a good correlation with total cord bilirubin; the highest correlation coefficient was significant in both cases (P<0.05). Transcutaneous bilirubin cut off values of 2.4 mg/dl and 2.6 mg/dl, for TCB over forehead and sternum respectively, have highest sensitivity and specificity. Both the TCB value over sternum and forehead were very well correlated, however TCB over sternum give slightly better yield then TCB over forehead as far as the sensitivity and specificity is concerned. Thus, TCB method can be used for diagnosis of hyperbilirubinemia with very high sensitivity rate. TCB over sternum give slightly better yield then TCB over forehead as far as the sensitivity and specificity is concerned.
DISCUSSION
In the present study, transcutaneous Bilirubin level over forehead and sternum taken at different interval were compared with serum Bilirubin level taken at the same time. On the first day Bilirubin value by TCB method is positively correlated with cord blood Bilirubin value with r2 value 0.8 indicating strong linear correlation. On the third day Bilirubin value by TCB method is positively correlated with conventional serum Bilirubin value with r2 value 0.97 indicating strong linear correlation. On the fifth day Bilirubin value by TCB method is positively correlated with conventional serum Bilirubin value with r2 value 0.95 indicating strong linear correlation. On the seventh day Bilirubin value by TCB method is positively correlated with conventional serum Bilirubin value with r2 value 0.95 indicating strong linear correlation. In the present study, ROC curve indicate that Bilirubin value of 5.1mg/dl by TCB over forehead indicates hyperbilirubinemia with sensitivity of 90.7%. Bilirubin value of 4.75 mg/dl by TCB over sternum indicates hyperbilirubinemia with sensitivity of 93.0%. Thus TCB method can be used for diagnosis of hyperbilirubinemia with very high sensitivity rate. Rosenfeld et al. reported infants with cord bilirubin levels less than 2.0 mg/dl have only a 4% chance of developing hyperbilirubinemia and a 1.4% chance of needing phototherapy. However, if serum cord bilirubin levels are more than 2.0 mg/dl, the infant has a 25%chance of developing subsequent hyperbilirubinemia.3 Knudsen et al. reported umbilical cord serumbilirubin concentration as a predictor of subsequent jaundice was studied in 291 newborns. It was possible to define subgroups of infants with significantly higher or lower risks of developing jaundice. If cord bilirubin was below 1.17 mg/dl, 2.9% became jaundiced as opposed to 85% if cord bilirubin was above 2.3 mg/dl. Furthermore, 57% of jaundiced infants with cord bilirubin above 2.3 mg/dl required phototherapy, but only 9% if cord bilirubin was 2.3 mg/dl or lower (P<0.0030).4 Trivedi et al. reported cord serum un conjugated bilirubin level >2.0 mg/dl and total cord serum bilirubin level >2.5 mg/dl appeared as high risk indicator towards predicting neonatal hyperbilirubinemia.5 Bernaldo et al.6 reported that the unconjugated bilirubin levels in cord blood were indicative of the jaundice severity developed by full-term newborns without complications, up to their third day of life. Levels that were equal to or greater than 2 mg/100 ml indicated a 53% probability of the need for further treatment by phototherapy. Shaker et al7reported that a critical cut off level of cord bilirubin was 2 mg/dl predicted 71% of the newborns who developed jaundice. However, the cord bilirubin level of <2 mg/dl has not completely excluded the development of significant hyperbilirubinemia. 1.9% of the newborns with cord bilirubin levels of <2 mg/dl have developed hyperbilirubinemia. Knüpfer et al.8 reported that for the prediction of further need of phototherapy using umbilical cord serum bilirubin cut-off level of 1.76 mg/dl, they found a sensitivity of 90% and a negative predictive value of 99.1%, indicating that all patients with umbilical cord serum bilirubin values below 1.76 mg/dl (443/1100 or 40.2%) were at a very low risk of developing dangerous hyperbilirubinaemia. A study by Tommy SK et al concluded that the JM-103 (as a point-of-care screening device) can be used safely in the Emergency Departments (AED) or Maternal and Child Health Centres (MCHC) for healthy-looking neonates aged 3 to 7 days; a transutaneous bilirubin (maxTcB) of less than 230 μmol/L can be used to let the patient return home for follow-up. However, the study found that a serum bilirubin assay still appears necessary for neonates with a maxTcB within the grey zone (230-298 μmol/L).9 In another study, a new transcutaneous bilirubinometer (JM-103 Minolta Airshields) for detection of hyperbilirubinemia in term or near-term healthy Chinese newborn was evaluated. TcB was significantly correlated with TSB, with a correlation coefficient of 0.83 (p= 0.001).10 Another prospective descriptive study by Janjindamas W concluded that serum bilirubin can be accurately measured by the transcutaneous bilirubinometer index in full term newborn infants prior to any intervention modalities.11The author revealed that the measurement technique was rapid and simple, and it was easy to perform repeated measurements over time, thus reducing the likelihood of error. Serum bilirubin measurements are still required when treatment with phototherapy or exchange transfusion is being considered. Another cross sectional study by Mahajan G et al.12to find out the correlation of transcutaneous bilirubinometer index (TcBI) with serum bilirubin levels in term, pre-term, small for gestation age babies, with and without phototherapy in neonates with jaundice. A total of 104 neonates were studied. The mean serum bilirubin was 16.6 mg/dL±6.1 (283.9 μmol/L) (SD) range (7.0-34.0), the mean transcutaneous bilirubin index reading over forehead was 22.7 mg/dL ±4.999 (388 μmol/L), (SD) range (14.0-37.0) and sternum was 21.2 mg/dL ±4.9 (363.5 μmol/L), (SD) range (12.0-36). Overall correlation coefficient of 0.878 at forehead and 0.859 at sternum was observed.
CONCLUSION
Trancutaneous bilirubinometer was effective in the estimation of serum bilirubin in term neonates. However, due to insufficient evidence to show the effectiveness of transcutaneous bilirubinomter in preterm neonates, serum bilirubin levels should be confirmed with chemistry analyzer.
REFERENCES
-
Shapiro SM. Definition of the Clinical Spectrum of Kernicterus and Bilirubin- Induced Neurologic Dysfunction (BIND). Journal of Perinatology 2005; 25: 54-59.
-
American Academy of Paediatrics Subcommittee on Hyperbilirubinemia. Management of hyperbilirubinemia in the newborn infant 35 or more weeks of gestation. Paediatrics 2004; 114(1):297-316.
-
Rosenfeld J. Umbilical cord billirubin levels as predictor of subsequent hyperbilirubinemia. J Fam Pract 1986; 23: 556-8.
-
Knudsen A. Prediction of the development of neonatal jaundice by umbilical cord blood bilirubin. Acta Paediatrica 1998; 78(2):217-221.
-
Trivedi DJ, Markande DM, Vidya BU, Bhat M, Hegde PR. Cord serum bilirubin and albumin in neonatal hyperbilirubinemia. Int J Int Sci Inn Tech Sec A 2013; 2(2):39-42.
-
Bernaldo NJA, Segre MAC. Bilirubin dosage in cord blood: could it prevent neonatal hyperbilirubinemia? Sao Paulo Med J 2004; 122(3): 99-103.
-
Shaker K. Gatea. Cord bilirubin level as predictor for Newborns at Risk for post natal Hyperbiliruinemia. Kufa Med.Journal 2009; 12(2):109-117.
-
Knupfer M, Pulzer F, Gebauer C, Robel-Tillig E, Vogtmann C. Predictive value of umbilical cord blood bilirubin for postnatal hyperbilirubinaemia.Acta Paediatr 2005;94(5):581-7.
-
Tommy SK, Lam KL, Kam CW. Evaluation of a point-of-care transcutaneous bilirubinometer in Chinese neonates at an accident and emergency department. Hong Kong Med J 2008; 14: 356-60.
-
Ho HT, Ng TK, Tsui KC et al. Evaluation of a new transcutaneous bilirubinometer in Chinese newborns. Arch Child Fetal Neonatal. Ed 2006; 91: F431-F438.
-
Janjindamas W, Tansantiwong T. Accuracy of Transcutaneous Bilirubinmeter Estimates Using Bili Check in Thai Neonates. J Med Assocc Thai 2005; 88(2):187-190.
-
Mahajan G, Kaushal RK, Sanchyan N, et al. Transcutaneous Bilirubinometer in Assessment of Neonatal Jaundice in Northern India. Indian Pediatrics 2005; 42:41- 45.