|
Table of Content - Volume 16 Issue 3 - December 2020
A study of association between chest X ray findings and severity of pneumonia in children between 2 to 59 months of age
Chethan K B1, Nandakumar V2*, Spoorthi S M3, Basanth Kumar G R4
1,3Assistant Professor, 2Junior Resident, 4Professor, Department of Pediatrics, JJM Medical college Davanagere Karnataka, INDIA. Email: chethankb9@gmail.com
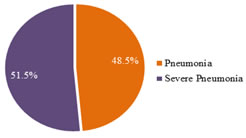
Abstract Background: Pneumonia is one of the major common respiratory problem in present clinical paediatric practice. Chest x ray is presently viewed as a major criterion for identifying the severity of pneumonia. Aim and objective: To study the association between chest x – ray findings and Severity of Pneumonia in children between 2-59months of age presenting with signs and symptoms of pneumonia. Methodology: Present study was a prospective study carried out on Children 2 - 59 months presenting with the symptoms of pneumonia selected as per WHO criteria. Correlation of Severity of pneumonia and x ray finding was studied. Results:n: In present study, out of 332 children admitted with pneumonia 161(48.5%) and severe pneumonia and 171(51%) had pneumonia. chest x-ray abnormalities were seen in 179(53%) cases and in 153(46%) cases. Patients who presented with cyanosis 23(0.69%), grunting 105(31%), hypoxia 106(31.9%) all three had significant radiological association with severe pneumonia (p<0.05).
INTRODUCTION Childhood community acquired pneumonia (CAP) continues to be the single most important cause of childhood morbidity and mortality in the world among under five age group.1 In early 90’s over 25% of annual deaths of children in developing countries before the fifth birthday was attributable to pneumonia. Although the implementation of safe, effective and affordable interventions has reduced pneumonia mortality from 4 million in 19812 to just over one million in 2013, 3,4 pneumonia still accounts for nearly one-fifth of childhood deaths worldwide. Recently the worldwide Global Burden of Disease analysis suggested that CAP accounts for 14% of deaths. In addition to immense public health importance, it has both immediate and late complication. 5 Case management is a cornerstone of pneumonia control strategies. 6 It consists of classifying the severity of illness using simple clinical signs such as fast breathing, chest indrawing and general danger signs, and then applying the appropriate treatment. Treatment includes home care advice, antibiotics for home therapy, or referral to a higher-level health facility The original guidelines classified the respiratory symptoms of children 2 to 59 months of age into four categories (no pneumonia, pneumonia, severe pneumonia, very severe pneumonia).7,8 Data shows that the majority of childhood pneumonia deaths are due to severe pneumonia/severe disease (9); management of these cases requires early identification, prompt referral and the availability of good-quality higher-level care. However, in many low-resource settings, referral is difficult and often does not take place. 10-14 On the basis of this information, WHO undertook a review of the evidence, with the aim of developing a simplified approach that could increase the number of children receiving correct treatment for pneumonia. In addition to the impact of acute disease, respiratory infections (especially when repeated) in young children are associated with long−term lung function abnormality and disease. 15 Early diagnosis and management are critical to short and long−term health outcomes with several clinical guidelines now available for both developing and developed country settings. 16 The implementation and effectiveness of the guidelines vary widely within and between countries and, in many regions, improvements are still required in the diagnosis and management of pneumonia at the community level. 17-20 Many factors contribute to these differences, including: health systems resourcing, the number of possible causative micro−organisms, host and environmental factors, timing of presentation to a health service, expertise of the health service providers at various levels of the health care system, availability of diagnostic facilities and the absence of a true diagnostic gold standard. 15 WHO clinical definition developed for the community setting in developing countries is based on the presence of cough and tachypnoea. 21 This definition was developed particularly with the intention of identifying children who had bacterial pneumonia and required antibiotics. The incidence of pneumonia caused by H. influenzae or S.pneumoniae has been significantly reduced in areas where routine immunization has been implemented. Despite advances in identifying microorganisms using highly sensitive molecular techniques, ascribing causation is problematic, The ideal samples for determining aetiologic agents in bacterial pneumonia are lower airway specimens. It is usually neither necessary nor feasible to obtain either bronchoalveolar lavage or needle lung aspirate specimens in acute pneumonia. 22 Thus, it is not surprising that the chest radiograph (CXR) has long been considered the 'gold standard for the diagnosis of pneumonia in children. Chest X-ray is presently a major criterion for identifying severity of pneumonia. Few studies show correlation between chest x-ray findings and severity 23,24 and few studies show no correlation between chest x-ray findings and severity. 25,26 This study helps us to know the role of chest x-ray in identifying the severity of pneumonia. Aim and objective: To study the association between chest x – ray findings and Severity of Pneumonia in children between 2-59months of age presenting with signs and symptoms of pneumonia.
MATERIAL AND METHODS Present study was a Prospective study carried out in the department of pediatrics J.J. M. Medical College, Davangere. Study population was All patients between the age of 2 months and 59 months presenting with the symptoms of pneumonia were selected as per modified WHO criteria. 27 Study was conducted during January 2018-june 2019. Inclusion criteria:
Exclusion criteria:
Study was approved by ethical committee of the institute. A valid written consent was taken from parents of children after explaining study to them. After considering inclusion and exclusion criteria, 332 children with symptoms of pneumonia were included. Data was collected with pre tested questionnaire. Data included demographic data like age, sex. Detailed history was taken by interview method from the parents of children. Presenting complaints, immunization status was recorded. Through clinical examination was done. All patients underwent investigations like Chest X – Rays, Complete blood count, and Blood culture. Chest x-rays were interpreted by radiologist. The cases were selected as per the WHO criteria for diagnosis of pneumonia and chest radiographs were interpreted as per the WHO guidelines. All patients were followed for clinical severity of pneumonia and course of illness in the hospital. Correlation was assessed of initial chest x – ray finding and severity of pneumonia as per criteria specified. The following WHO definitions and criteria were used for categorizing patients with pneumonia and interpretations of chest x-ray. Data was entered in the excel spread sheet. SPSS (Statistical Package For Social Sciences) version 20. [IBM SPASS statistics (IBM corp. Armonk, NY, USA released 2011)] was used to perform the statistical analysis. Descriptive statistics of the explanatory and outcome variables was calculated by mean, standard deviation for quantitative variables, frequency and proportions for qualitative variables. Inferential statistics like Chi square test was used to test the significance between qualitative variables. The level of significance was set at 5%.
RESULTS Out of 332 patients, 34.6% were in age group of 25-59 months, 34.3% were between 3-12 months and 31% were between 13-24 months. In the present study, 50.6% were females and 49.4% were males. In our study, out of 332 patients, 171 (51.5%) had severe pneumonia and 161 (48.5%) had pneumonia. In our study, majority patients were fully immunized (93.1%). Among all the children, 90.7% were normal, 3.9% were having moderate acute malnutrition and 5.4% were suffering from severe acute malnutrition. In our study, out of 332 patients, majority presented with one or the other symptoms. 59% presented with fever, 78.6% had cough, 99.4% had tachypnea, 99.4% had chest indrawing, 70.5% had bilateral rhonchi and 67.5% had bilateral crepts. Whereas, 77.7% were not having any breathing difficulty. Only 2.1% presented with convulsion/drowsy, 6.9% had cyanosis, 20.2% were pallor, 31.6% had grunting and 31.9% presented with hypoxia. In the present study, out of 332 cases, 196 (59%) presented with fever and 136 (41%%) did not had fever. Out of 196 cases, 127 (64.8%) cases showed positive radiological findings, of which 123 had severe pneumonia and remaining 4 had pneumonia . Association of fever and x ray finding was statistically significant at p value <0.001. (table 1) In our study, out of 332 cases, 105 (31.6%) cases showed clinical signs of grunting. Among 105 cases with grunting, 100% had severe pneumonia. Among the remaining 227 cases, majority of those with radiological findings had severe pneumonia (70) and majority with normal findings had pneumonia (101). This is statistically significant at p value <0.001. If child presents with Grunting likely to have positive radiological findings was observed with severe pneumonia. (table 2) Out of 332 cases, 106 (31.9%) cases showed clinical signs of hypoxia and 226 (68.1%) did not showed any signs. Out of 106 cases, 100 (94.3%) cases showed positive radiological findings and all of them had severe pneumonia and among other 6(5.7%) cases who showed normal chest x-ray findings 4 had pneumonia and 2 had severe pneumonia. And this is statistically significant at p value <0.001. Among the remaining 226 cases, majority of those with radiological findings had severe pneumonia (41) and majority with normal findings had pneumonia (119). This is statistically significant at p value <0.001. If child presents with hypoxia most likely radiological findings was observed with severe pneumonia. (table 3) In our study, out of 332 cases, 23 (6.9%) cases showed clinical signs cyanosis and 309 (93.1%) did not showed any clinical signs. If child presents with cyanosis or not, positive radiological findings was noted among cases with severe pneumonia and normal chest x-ray was noted among pneumonia cases. (p<0.05) (table 4) In the present study, out of 332 cases, only 7 (2.1%) cases presented with convulsions. Out of these 7 cases, 5 (71.4%) cases showed positive radiological findings, of which all of them had severe pneumonia. Of the remaining 325, 174 (53.5%) showed positive chest x-ray findings and 151 (46.5%) showed normal findings. Majority of those with radiological findings had severe pneumonia (136) and majority with normal findings had pneumonia (121). This is statistically significant at p value <0.001. (table 5) Graph 1: Distribution of patients based on the severity of Pneumonia
Table 1: Association between Pneumonia with fever and chest x-ray findings
Table 2: Association between Pneumonia with grunting and chest x-ray findings
Table 3: Association between Pneumonia with hypoxia and chest x-ray findings
Table 4: Association between Pneumonia with cyanosis and chest x-ray findings
Table 4: Association between Pneumonia with convulsions and chest x-ray findings
DISCUSSION In our study total of 332 cases were included 48.5% had pneumonia and 51.5% had severe pneumonia, among them 179 radiological and 153 non radiological cases, no significant association for age(p-0.02),cough(p-0.21) , tachypnea(p-0.212), chest indrawing (p-.21), pallor(p-0.181)with CXR was found . findings on history/examination partial immunization, SAM , fever ,feeding difficulties(p-0.001) had predominantly radiological findings in severe pneumonia cases than pneumonia, clinical presentation like grunting(p-0.001), cyanosis(p-0.04), hypoxia(p-0.001), had significant radiological association, on CXR bilateral infiltrates, primary end point consolidation either lobar or segmental majority cases were of severe pneumonia. A study done by Jain DL et al. at Indra Gandhi government medical college, Nagpur to assess severity of pneumonia aged 3-59 months , total 307 chest xrays, 146 were normal and 148 were abnormal, clinical signs of severity i.e chest indrawing , cyanosis, grunting(p-0.02), convulsions (p-0.03) and hypoxia (p-0.00) were associated with abnormal radiographs. 28 Maria Francesca Patria et al. did similar study in Italy, Seventy-six of the 335 enrolled children (22.7%) fulfilled the criteria for severe CAP. The most frequent radiological presentation was focally distributed parenchymal densities (212, 63.3%). Severe CAP was associated with a bilateral multifocal distribution (OR 2.30; 95% CI, 1.29-4.10). No association was found between CAP severity and the presence of atelectasis, middle right lobe involvement or pleural effusion. 29 Kelly,Matthew S,et al.. did study in that 249 children with evaluable chest radiographs. Median age was 6.1 months, and 58% were male. Chest radiograph classifications were primary endpoint pneumonia (35%), other infiltrate/abnormality (42%) or no significant pathology (22%). 30 Kerry-Ann et al., did study 24 115 hospitalised episodes of care for 9492 children and 13 683 chest radiographs. The average annual cumulative incidence of endpoint consolidation was 26.6 per 1000 population per year (95% CI, 25.3–27.9); 57.5 per 1000 per year in infants aged 1–11 months. 31 Matthew D. Garber et al. concluded A negative CXR result excludes pneumonia in the majority of children. Children with negative CXR results and low clinical suspicion for pneumonia can be safely observed without antibiotic therapy.” Perhaps it is also time to say, “Children with low clinical suspicion for pneumonia can safely be observed without CXRs(65). In our study also non-radiological ( negative CXR was found in 46%), with this we can plan management ,treatment stratergy accordingly. 32 In a prospective study done by Julia E Clark, et al., out of 700 children who presented to the hospital with pneumonia only 20% had lobar x-ray changes. In this study neither CRP, pyrexia or lobar x-ray findings, were associated with severity. 33 Study done by Njeze Ngozi R et al. included a total of 100 chest radiographs of children 16years and below with clinical symptoms of pneumonia and their request forms were reviewed. Thirty seven (37) of the radiographs were in agreement with clinical diagnosis of pneumonia while 63 radiographs had no evidence of infection or inflammation in the lung fields; the authors were of the opinion that Chest radiographs are efficacious in the management of children suspected to have pneumonia but predicting the severity was inconclucive. 34
CONCLUSION Severity of pneumonia like fever, grunting, hypoxia ,feeding difficulty, cyanosis correlate with x-ray findings.
REFERENCES
Policy for Articles with Open Access: Authors who publish with MedPulse International Journal of Pediatrics (Print ISSN: 2579-0897) (Online ISSN: 2636-4662) agree to the following terms: Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution License that allows others to share the work with an acknowledgement of the work's authorship and initial publication in this journal. Authors are permitted and encouraged to post links to their work online (e.g., in institutional repositories or on their website) prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work.
|
|
 Home
Home