|
Table of Content - Volume 16 Issue 3 - December 2020
Sensorineural hearing loss in infant following acute bacterial meningitis
Swati Jain1*, Vaibhav Gode1, Ashwini Kundalwal1, Leena Jain2
1Department of Paediatric, 2Department of ENT, SMBT Medical College and Research Centre, Dhamangaon, Igatpuri, 422403 INDIA. Email: drswatijain85@gmail.com Abstract Background: To study the incidence of sensorineural hearing loss (SNHL) in infants with acute bacterial meningitis (ABM). Methods: It was an ambispective observational study carried out in paediatric department of medical college and tertiary care centre in Northern Maharashtra. Total of 50 infant who had done hearing assessment after acute bacterial meningitis were included. After history and physical examination, CSF cytology, biochemistry and culture sensitivity were sent. Imaging of brain was done if required. Ear examination was done to rule out any cause for conductive hearing loss. An audiological assessment of the patient was done at the time of discharge using BERA by “Intelligent Hearing system” Results: Of the 50 children with ABM, 50% were less than one month old, 38% were 1-6 month, and 12% were 6-12 month of age. 56% were females and 44% were males. Refusal to feed, seizure and fever were the most common presenting symptoms. 44% had abnormal imaging of Brain. Hydrocephalus being the most common abnormal finding seen in 22% cases. 13(26%) developed SNHL following ABM. SNHL was bilateral in 7(14%) and unilateral in 6(12%) cases. 3(6%) had mild SNHL, 5(10%) had moderate SNHL, 4(8%) had severe and 1(2%) had profound hearing loss. Conclusions: 26% infants developed sensorineural hearing loss after ABM which emphasizes the need for audiological evaluation of a child after meningitis. BERA is a helpful tool for screening the SNHL especially in the young children. Keywords: SNHL (sensorineural hearing loss), ABM (acute bacterial meningitis), BERA- (Brainstem Evoked Response Audiometry), CSF (cerebrospinal fluid)
INTRODUCTION Deafness is one of the most common serious complication of acute bacterial meningitis (ABM) in children1. Complete or partial Deafness occurs in 5% to 35% of survivors of meningitis. Profound bilateral hearing loss will occur in up to 4% of patients2. It is one of the leading cause for acquired deafness in infancy and childhood and accounts for 90% of all causes of acquired hearing impairment by the age of 3 years.3,4 It is the result of cochlear or auditory nerve inflammation.5 Most meningitis-associated SNHL emerge in the acute stage of meningitis and remain stable after recovery, but there can be spontaneous regressions, fluctuations, or progressions in hearing after recovery from meningitis.6 Early identification is essential for successful rehabilitation, including cochlear implantation.7 School-age meningitis survivors has either serious and disabling sequelae or a functionally important behavior disorder, neuropsychological or auditory dysfunction adversely affecting academic performance.8 Hearing loss in very early life can affect the development of speech and language, social and emotional development and communication skills, social adjustment and academic achievement of the young child. Hearing assessment is difficult in infants. Auditory brain stem evoked response (ABER) is used to assess hearing in this population.9 Early intervention could be done if SNHL detected early, which if left untreated may lead to serious handicap affecting the overall development of child. Assessment of hearing in children after meningitis is recommended.5 since there are very few Indian studies of assessment if hearing loss in ABM, we decided to study incidence of sensory neural hearing loss (SNHL) in cases ABM.9
METHODS It was an ambispective observational study conducted in pediatric department of tertiary care hospital in northern Maharashtra. Fifty infants with ABM were enrolled in the study with written informed consent from parents. Details were recorded in a pre-decided proforma. Including age, gender and detailed history followed by complete physical examination. Lumber puncture was performed in all the children for CSF examination. Diagnosis of ABM was considered when CSF examination showed polymorphonuclear pleocytosis, low sugar and high protein for age and /or CSF culture positive for bacterial growth. Children with age more than 1 year, history of neurodevelopmental delay, tubercular meningitis, head injury, associated comorbid condition like HIV infection, heart disease, neural tube defects or Pathological hyperbilirubinemia in newborn period were excluded from study. Fundus examination was done to look for papilledema. ABM was treated as per standard guidelines. Some patients were also given dexamethasone. Radio imaging of brain was done if required. Ethical approval was taken from hospital ethical committee. Ear examination was done by otorhinolaryngologist in all cases to rule out causes for conductive hearing loss. An audiological assessment of the patient was done at the time of discharge using Brainstem Evoked Response Audiometry (BERA) by “Intelligent Hearing system (I.H.S.) the data was presented in an excel sheet and analyzed statistically using SPSS 17 software. Ethical approval: taken
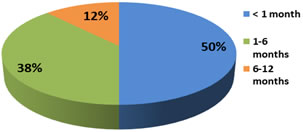
RESULTS Fifty children below 1 year of age diagnosed to have ABM were enrolled in the study. Cases were categorized into two groups as with SNHL present (group I) and SNHL absent (group II). Of the 50 children with ABM, 25(50%) were less than one month old, 19(38%) were 1-6 month, 6(12%) were 6-12 month of age. (Figure 1) 28(56%) were females and 22(44%) were males. Female to male ratio was 1.27:1. Refusal to feed, seizure and fever were the most common presenting symptoms in our study. (Table 1). 22(44%) had abnormal imaging (USG/CT/MRI) of Brain. (Table 2) Hydrocephalus being the most common abnormal finding was seen in 11 cases. Table 1: Symptoms in ABM and their frequency
Table 2: Abnormal findings on brain imaging in ABM and its percentage
13(26%) out of 50 children developed SNHL following acute bacterial meningitis. SNHL was bilateral in 7(14%) and unilateral in 6(12%) cases. SNHL was mild in 3 patient, moderate in 5 patients, severe in 4 patients and only 1 patient had profound hearing loss. (Table 3). Table 3: Distribution of SNHL in children with acute bacterial meningitis
Figure 1: Age Distribution of the cases among sensory neural hearing loss (SNHL)
Incidence of SHNL was more in infants below one month. It was observed that incidence of SHNL was decreased as age increases but this trend is not statistically significant (p value=0.3). 25% of females and 27.27% of males developed SNHL, but no correlation was found between gender and occurrence of SHNL. Mean days of illness before admission was 3.44 days. There was no relationship found between no. of days of illness before treatment and development of SNHL. Amongst 27 cases with altered sensorium, 9 developed SNHL, which suggests that there is increased risk of development of SNHL in patient with altered sensorium in ABM which was statistically found to be significant (P- value 0.04) Amongst 13 cases with Glasgow coma scale (GCS) less ≤ 8, 7 developed SNHL. Risk of developing SNHL was found to be higher in patient who had GCS less than 8.This correlation was found statistically significant (P value 0.02) but there was no significant correlation between fever, seizure and development of SNHL in patient with ABM. Out of the 13 cases of SNHL, etiology could be identified in 5(38.4%) cases. S. Pneumoniae, E. coli, Klebsiella, Gram positive cocci, Gram negative bacilli were responsible for 1 case each. Among 18 cases who have received dexamethasone, 6 developed SNHL, which was found to be statistically insignificant. Dexamethasone therapy was not associated with decreases incidence of SNHL in present study. Among 45 cases who had received amikacin in recommended dosages, 12 developed SNHL, which also was found to be statistically insignificant. (P-value: 1.0) Patient with high value for Mean ± SD for Total nucleated cells in CSF for group I was 1675.4 ± 2318.6 while for group II it was 444.57±360.3. CSF Total Neutrophil count had more incidence of SNHL. (P value 0.003). Mean ± SD for Protein (mg/dl) in CSF for group I was 415.2 ± 484.1 while for group II it was 204.1 ± 210.3. Patient with higher value for CSF protein had more SNHL. (P value 0.036). Mean ± SD for Sugar (mg/dl) in CSF for group I was 25.5± 15.8 while for group II it was 40.3 ± 15.9. Patient with low value for CSF sugar have more SNHL. Among 9 cases with CSF sugar less than 20, 5 developed SNHL, which was statistically significant (P value 0.03). Risk of developing SNHL is higher in patient who have CSF sugar less than 20. There was no significant difference in WBC, Hb and platelets count between 2 groups. Among 23 cases who had abnormal imaging of brain, 10 developed SNHL. Hydrocephalous, Acute infarcts, subdural effusion andcerebral edema, Ventriculitis with hydrocephalous, and subdural hemorrhage were few abnormal findings noted in brain imaging. Though patients with abnormal imaging of brain had more SNHL but this observation was not statistically significant in present study.
DISCUSSION Of the 50 children enrolled in the study, 13(26%) developed SNHL following acute bacterial meningitis which was found to be similar to other studies where incidence of SNHL was 25.7%, 28.1% and 20.8% in ABM.9,10,11 Widely variable incidence of SNHL in ABM has been reported in studies done in India. Variations of incidence ranged from 36.6% to 64% on higher end while in some studies reported much lower incidence of 6%- 7%. 12,13,14 15,16 In the present study, SNHL was bilateral in 14% and unilateral in 12% cases, which was found to be similar when compared with a study done by Damodaran et al., where bilateral SNHL was present in 11.4% and unilateral SNHL was present in 14.3% of cases.9 Taylor et al. reported an incidence of 11.3%, with 6.1% being unilateral and 5.2% being bilateral.17 Higher Incidences of bilateral SNHL were seen in some other studies.10,12,18 Lower incidence of bilateral hearing loss of only 4% along with unilateral SHNL of 3% is seen in a study done by George CN et al..16 In studies done by Cherian et al. uniilateral SNHL was present in 6.2 %, which was much lower as compared to results of our study.10 In our study, 6% had mild SNHL, 10% had moderate, 8% had severe and 2% had profound SNHL. In study done by Cherian et al.. 3.14% had mild SNHL, 12.47% had moderate, and 12.47% had severe profound SNHL.10 In a study by Singh et al., 6.6% had severe and 30% had moderate SNHL.13 These variations in the incidence and type of SNHL can be due to various other factor affecting development of SNHL in patient with ABM. Out of the 50 cases of ABM, etiology could be identified in 5 cases of which S. Pneumoniae, E. Coli, Klebsiella, Gram positive cocci, Gram negative bacilli were responsible for 1 case each and all 5 cases developed SNHL .No definite etiology for ABM could be identified in most cases as patients had already received antibiotics before being referred to us. Panjarathinam R et al. concluded that culture positivity varied form 12.12 to 56%.19 In a study, Hemophilus was the most common bacteria (49%) causing ABM, followed by Pneumococcus (22%) and Meningococcus (15%).20 Higher incidence of hearing loss is seen in pneumococcal meningitis.5,21,22In present study there was no association found between sex of patient and incidence of ABM (P value = 1). Similar results were seen in study done by singh et al.. In the study by Gupta V, age and sex of the patient were not significant risk factor in the development of hearing impairment.11 Refusal to feed (72%), seizure (68%), fever (68%) and altered sensorium (54%) and irritability (52%) were the most common presenting symptoms in our study. From a study done by Roine et al.with bacterial meningitis, approximately 78% were lethargic, 7% were somnolent, and 15% semi-comatose or comatose at the time of admission.23 In present study, no correlation was found between fever, seizure and development of SNHL in cases with ABM. It was similar to study by Charuvanij et al. where no significant correlation was observed between hearing loss and various clinical and demographic factor.18 Cherian et al. observed that the total duration of fever was significantly different in those with and without SNHL (P < 0.05) but presence of seizure was not significantly associated with SNHL.10 Seizure was found to be a strong predictor for hearing loss in ABM in various other studies.12,13,22,24In our study, altered sensorium and GCS <8 were significantly associated with increased risk of SNHL in patient with ABM (P value = 0.04 and 0.02). Roine I et al. also observed that the level of consciousness is the most important predictor of neurological sequel.23 Cherian et al. observed that presence of altered sensorium were not significantly different in those with and without SNHL.10 In another study by Kapoor et al., modified GCS < or = 8 was significantly associated with abnormal BAER with P value < 0.001.12 In the present study CBC parameter were not significantly associated with hearing impairment. CSF pleocytosis was significantly associated with development of SNHL in the present study with p value of 0.003 and was consistent with other studies where CSF pleocytosis was strongly correlated with SNHL.9,25,26 In study by Bhatt SM, onset of hearing loss was proceeded by a CSF leukocytosis of > 2000 cells/ mm3.25 Increased CSF protein levels were significantly associated with SNHL in the present study with p value of 0.036 which was found to be consistent with other studies where high protein in CSF was associated with a significantly higher risk of hearing loss.10,11 Association of low CSF sugar with SNHL was statistically significant in the present study (P value = 0.006) which was found to be similar with the other study.11,26 In study by Kapoor et al., CSF sugar (<20mg%) was significantly associated with abnormal BAER (P value< 0.05).12Among 18 cases who received dexamethasone, 6 developed SNHL. Dexamethasone therapy was not associated with decreases incidence of SNHL in present study which was comparable with other studies.21, 27 Contrary to above observation, significant reduction in incidence of hearing loss after dexamethasone therapy was noted by Girgis NM et al..28 In present study, amikacin was not associated with increased risk of SNHL, which was similar to study done by Cherian B et al.. where aminoglycoside usage were not significantly different in those with and without SNHL.10Patients with abnormal imaging of brain had more SNHL compared to those with normal, but there was no correlation found between abnormal imaging of brain and increased incidence of SNHL in present study, this is similar to study by Singh K et al.,where no relation was observed between hydrocephalous, subdural effusion and higher incidence of SNHL.13
CONCLUSIONS The present study throws light on the occurrence of sensorineural hearing loss following acute bacterial meningitis. SHNL, which if left untreated may lead to serious handicap affecting the linguistic performance and overall development of the child. Hence our study emphasizes the need for complete audiological evaluation of a child recovered from meningitis. BERA is a helpful tool for screening the sensorineural hearing loss especially in the young children and infants in whom other conventional methods may not be of much use. With the advent of newer vaccncies, the incidence of bacterial meningitis and its sequelae has dramatically decreased in the developed countries. Hence there is an urgent need to include the H. influenza and pneumococcal vaccines in the routine immunization schedule thereby decreasing the incidence of bacterial meningitis and its sequelae like sensorineural hearing loss. Since there are very few Indian studies of assessment of hearing loss in ABM and there are lot of variation in finding noted by various researchers which warrants need of further studies of hearing loss in ABM. ACKNOWLEDGEMENTS We wish to thank the consultant paediatricians, audiologists, microbiologists, and the resident doctor and nursing staff of paediatric department of SMBT medical college and research centre, Dhamangaon, igatpuri
REFERENCES Richardson MP, Reid A, Tarlow MJ, Rudd PT. Hearing loss during bacterial meningitis. Arch Dis Child. 1997; 76 134- 138.
Jama and Archives Journals. Risk Factors Identified For Hearing Loss In Children With Bacterial Meningitis. Science Daily. [Internet]. 2006, September 25. Available from: http://www.sciencedaily.com/releases/2006/09/060918192239.htm
Vernon M. Meningitis and deafness: the problem, its physical, audiological, Psychological, and educational manifestations in deaf children. Laryngoscope.1967 Oct; 77(10):1856-1874.
Fortnum HM. Hearing impairment after bacterial meningitis: a review. Arch Dis Child. 1992 Sep; 67(9):1128-1133.
Janowski AB, Hunstad DA. Acute Bacterial Meningitis beyond the neonatal period. Nelson Textbook of Pediatrics, 21st ed. Philadelphia: ELSEVIER; 2020: 3223-3232.
Brookhouser PE, Auslander MC, Meskan ME. The pattern and stability of Postmeningitic hearing loss in children. Laryngoscope. 1988 Sep; 98(9):940-948.
Grimwood K, Anderson VA, Bond L, Catroppa C, Hore RL, Keir EH et al.. Adverse outcomes of bacterial meningitis in school-age survivors. Pediatrics. 1995 May; 95(5):646-656.
Damodaran A, Aneja S, Malhotra VL, Bais AS, Ahuja B, Taluja V. Sensorineural hearing loss following acute bacterial meningitis--a prospective evaluation. Indian Pediatr. 1996 Sep;33(9):763-766
Panjarathinam R, Shah RK. Pyogenic meningitis in Ahmedabad. Indian J Pediatr. 1993 Sep-Oct; 60(5):669-673.
Roine, I. Peltola, H. Fernández et al.., Influence of admission findings on death and neurological outcome from childhood bacterial meningitis. Clin Infect Dis 2008; 46(8):1248-1252.
Girgis NI, Farid Z, Mikhail IA et al.. Dexamethasone treatment for bacterial meningitis in children and adults. Pediatr Infect Dis J. 1989 Dec;8(12):848-851.
Policy for Articles with Open Access: Authors who publish with MedPulse International Journal of Pediatrics (Print ISSN: 2579-0897) (Online ISSN: 2636-4662) agree to the following terms: Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution License that allows others to share the work with an acknowledgement of the work's authorship and initial publication in this journal. Authors are permitted and encouraged to post links to their work online (e.g., in institutional repositories or on their website) prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work.
|
|
 Home
Home