|
Table of Content - Volume 18 Issue 1 - April 2021
Clinical and diagnostic variants of tuberculous meningitis presentation
Manojkumar G Patil1, Sampada Tambolkar2, Shradha Salunkhe3, A D Mishra4, Sharad Agarkhedkar5
1,3,4Associate Professor, 2Professor, 5Professor & HOD, Department Of Paediatrics, Dr D.Y. Patil Medical College, Hospital And Research Center & Dr. D.Y.Patil Vidyapeeth, Pimpri, Pune, Maharashtra, India -Pin-- 411018, INDIA. Email: ambrish4764@gmail.com
Abstract Background: Childhood tuberculosis (TB) has a high incidence and prevalence in developing countries like India with tubercular meningitis (TBM) being the most common cause of death. Bacteriological confirmation of diagnosis is ideal but is often difficult because of its paucibacillary nature as well as decreased sensitivity and specificity of diagnostic tests. Early diagnosis and management of the disease, though difficult, is essential to avoid death or neurologic disability. We have studied the TBM pediatric patents in tertiary care center to study the clinical profile. Out of 20 children, 20% mortality and 80% had neurological deficit. So considering high mortality and morbidity, early suspicion diagnosis and compete treatment is most important factors for treating TBM in children. Key words: TBM, Meningitis, CSF.
INTRODUCTION Of all the manifestations of Tuberculosis, meningitis is the most serious. Tuberculosis of central nervous system is the most severe complication and is fatal without prompt and appropriate treatment1. It arises from metastatic lesion in the cerebral cortex or meninges which develop during lymphohematogenous spread of primary infection2. Tuberculous Meningitis (TBM) occurs when Mycobacterium tuberculosis invade the membranes and fluid surrounding the brain and spinal cord. The lesion results in exudate infiltrates, inflammation, obstruction and subsequent infarction in brain parenchyma and meninges. The exudates interfere with cerebro- spinal fluid flow and leads to hydrocephalus. Brain stem being most common site involved results in cranial nerve dysfunction3. Notwithstanding the availability of potent and specific drugs, fatality rate of Tuberculous Meningitis still remains high as compared to that of all other manifestations. Even when it is not fatal, the sequela are so severe and are disabling, We generally estimate the incidence based on hospital figures1. But these are an underestimate and imprecise. How many children die undiagnosed is anybody’s guess. So is the size of the population from which a hospital draws its cases. TBM has highest incidence from 6months to 3years. Primary infection is usually seen in lungs, mediastinal glands, bowel and mesenteric glands. Tubercle bacilli however, are a very sensitive index of the prevalence of pulmonary tuberculosis in a community or country. When tuberculosis starts declining, the decline is first seen in younger age groups and in respect of those manifestations which, like miliary and meningeal disease, result from haemato-genous dissemination soon after primary infection. The higher the age at first infection, the lesser the risk of haematogenous dissemination5. When the infector pool in a community gets reduced, first infection shifts towards higher age groups with resultant reduction in the risk of haematogenous dissemination and, therefore, meningitis. Thus TBM is extremely rare today in low prevalence countries. Stages
Pathology It depends on of affected region i.e, Meninges – exudates, adhesions leads to hydrocephalus, cranial nerve palsies, arterial compression and inflammation Brain – encephalitis, cerebral edema, infarcts, ventricular dilatation, tuberculoma10 Blood vessels – compression or inflammation Factors BCG vaccine given to protect from tuberculosis2. Though TBM can and does develop even in vaccinated children, it is a common observation that if B.C.G. coverage is adequate, incidence of TBM goes down even in the absence of general decline in tuberculosis on the whole. We being in developing country even nutrition and socio economic status plays an important role in spreading infection and sustaining the illness5. The review article in this issue deals exhaustively with the clinical aspects of the disease. A point of utmost importance is that early diagnosis and prompt starting of treatment are imperative for recovery and prevention of serious complications which might lead to irreversible neurological damage. Aim should be to diagnose a case before signs of neurological involvement appear7. It is easier said than done. For early diagnosis, suspicion index of the physician has to be very high because clinical features are protean and equivocal- In a child with unexplained and marked toxemia, lumbar puncture should not be delayed, especially if there has been a recent contact with an open case of pulmonary tuberculosis. Source of contact is, however, more often an unknown extra-familial case. But even the examination of C.S.F. may not provide clinching evidence to make an unequivocal diagnosis. Failure to find tubercle bacilli in C.S.F. in as high a percentage of cases as in western countries is very striking8. Even in the best of hands, say Tuberculosis Research Centre, Madras Laboratory, C.S.F. is not positive in more than 30% or so of cases diagnosed TBM on clinical evidence. And this low figure is definitely not due to any deficiency of technique or diligence. Is it then that many such C.S.F. negative cases are not of TBM but of some other disease simulating tuberculosis. After all, tuberculosis is a notorious mimic! It is obvious that concerted efforts are called for, on priority basis, to solve this problem. Immunology too seems to be opening up a new vista in this field. Animal experiments have shown that immune status of an animal (as judged by tuberculin reaction) and the number and viability of invading bacilli, inter alia, influence the extent and severity of the meningeal involvement and neurological complications11. In other words, negative tuberculin reaction in a morbid case with extensive meningeal involvement may not be the result but even the cause of extensive disease, provided of course the response in animals is applicable to man also3,9. This aspect needs further studies. Thus, while reduction in the size of the infector pool can prevent TBM to some extent, the gut issues involved are authentic criteria for early diagnosis and means to rectify the factors responsible for neurological damage12. It is research in these directions that will be most rewarding. Aims and objectives
MATERIALS AND METHODS 20cases of TBM were observed from May 2014-august 2015.Children Below age of 12 years admitted to the hospital with symptoms suggestive of TBM were considered for selection. The following inclusion and exclusion criteria were applied. Inclusion criteria Two or more of the following features with or without fever should be present to suggest a clinical diagnosis of TBM- altered sensorium varying from drowsiness to coma, headache, vomiting, history of convulsions{focal or generalized},meningeal signs, bulging fontanel ,papilledema, cranial nerve palsy ,and motor weaknesses of limbs. Exclusion Criteria Old cases of TBM treated outside the hospital before referral, children suffering from chronic illnesses or malignancies and children on immunosuppressive drugs were not included in study. After registration, detailed history was elicited. Vaccination and history of contact with a known patient suffering from pulmonary tuberculosis in the house or in the neighborhood was determined. A complete clinical examination was carried out and finding regarding neurological examination were recorded. Socioeconomic status was classified according to Kuppu-swamy classification and nutritional status was assessed and classified according to classification recommended by nutritional subcommittee of the Indian Academy of pediatrics. For all registered case a lumbar puncture {LP} was carried out within 24h ours of admission. The CSF was examined for cells within 10 mins of LP. The CSF was sent for biochemical examination of protein levels. A sample of CSF was sent for isolation of {AFB} acid –fast bacilli by smear and culture. To identify AFB in smear, fluorescent microscopy method was using auramine phenol was used. For AFB culture, the following 4 media were used: Lowenstein –Jensen Medium, Lowenstein Jensen Medium with 0.5 % Sodium pyruvate, 7H11 Middlebrook Medium and Kirschner’s Medium. One loop full of CSF was inoculated into the above three solid media and 0.2ml was added to the Kirschner”s Medium ,using a sterile pipette .The bacteriological examination were carried out at the Tuberculosis research Centre. Chest X-ray and Mantoux skin test and TB PCR carried out for all patients. No alteration were made in the treatment given to child while at the hospital. The standard regimen followed at our hospital for the treatment of TBM is Isoniazid (10 mg/kg), Rifampicin (10-12 mg/kg), Pyrazinamide (30 mg /kg) and Ethambutol (35 mg/kg)with streptomycin(15 mg /kg) as required .this is followed by 10 months of HRE. Steroids are given for the first 4 -6 weeks of treatment. All these patients were reviewed at the time of discharge and advised to continue AKT at the TB clinic in our hospital. The Mortality and morbidity of all cases, were assessed at the end of one month irrespective of bacteriological confirmation of CSF because generally CSF cultures results 6 weeks after the inoculations.
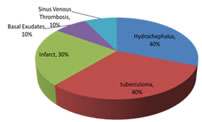
RESULTS Of 20 cases, clinically 85% presented with feverandconvulsions,65% altered sensorium,40% with cranial nerve palsies and 20% with headache and gcs<7.80% were immunized for BCG according to history and only 75% had BCG scar and also 85% were malnourished. Of all 90% were of low socio economic status and poor hygiene. Diagnostically 20% showed mantoux test positive, whereas csf examination showed raised protein and predominantly lymphocytic picture, 60% of children had TB-PCR positive and 40% had raised ada. A total of 70% children were in stage2 TBM and 30% were in stage3 and 40% children had tuberculoma on MRI, 40% had hydrocephalus, 30% had infarcts, 10% also shows basal exudates and 10% sinus venous thrombosis. All patients where started on AKT and steroids, out of which 50% had complications like raised ICP who were treated with hypertonic saline and 40% had hydrocephalus for which VP shunt was placed. Due to AKT20% had hepatotoxicity and 10% had DIC as complication. Among all patients 30% had a total stay of 4months duration and 10% had less than 2 months at hospital. Among 20 patients 4 were expired due to raised ICP and brain damage. Figure 1:
Table 1: Treatment
DISCUSSION In our study, we found that the children between age group 2 to5 years were MOST affected, but the severe form of disease was seen in children less than 2 years and the most common presentation being fever, convulsions and altered sensorium. Karande and Mahadevan et al showed more incidence of severe disease in children below 3 years with 58 % affection in that age group.5-6 But few cases also presented with headache, low GCS, and cranial nerve palsy .Almost 33% cases had nerve palsey in study by Karande et al.5 Out of 20 children majority were in stage 2 ,most of children belong to low socioeconomic status and were malnourished. Our finding also correspond with study of Karande et al5 and Mahadevan et al6. We also observed that the more advanced the stage of the disease; the grater was morbidity and mortality. Similar finding were noted in abode mentioned studies.5-6 CSF shows high protein levels and the most common finding on imaging being hydrocephalus and tuberculoma .These observations also were noted by Mahadevan et al in their studies6. Out of 20 children, 20% mortality and 80% had neurological deficit. Similar finding were shown in Karande et al study and Mahadevan et al in their studies .5-6 CONCLUSION The paediatrician must suspect and diagnose TBM as soon possible so that child is treated empirically and appropriately so as to improve treatment outcome and decrease morbidity.
REFERENCES
Policy for Articles with Open Access: Authors who publish with MedPulse International Journal of Pediatrics (Print ISSN: 2579-0897) (Online ISSN: 2636-4662) agree to the following terms: Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution License that allows others to share the work with an acknowledgement of the work's authorship and initial publication in this journal. Authors are permitted and encouraged to post links to their work online (e.g., in institutional repositories or on their website) prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work.
|
|
 Home
Home