|
Table of Content - Volume 18 Issue 3 - June 2021
A study of electrolyte and acid base disturbances in acute gastrointestinal diseases in children
Rajendra Hiralal Bedmutha1*, Mohammed Ajaz Mohammed Haneef Shaikh2
1,2Associate Professor, Department of Paediatrics, Dr. Ulhas Patil Medical College, Jalgaon, Maharashtra, INDIA.
Abstract Background: The main cause of death in acute diarrhoea is dehydration, which results from the loss of fluid and electrolytes in diarrhoeal stools, vomit, sweat, urine and breathing. Electrolyte disturbances may remain unrecognized and result in increased morbidity and mortality in children with acute gastroenteritis. Aim and objective: To study the electrolyte and acid base disturbances in acute gastrointestinal diseases in children Methodology: Present study was a prospective study carried out in paediatric department on paediatric patients admitted in paediatric ward with diarrhoea. Systemic examination of patients was done with assessment of severity of dehydration, sensorium of patient, preformed proforma. Laboratory investigation like Hemogram, Sr. Sodium, Sr. Potassium, Sr. Creatinine and Sr. Urea and ABGA analysis were done. Data was analysed with appropriate statistical tests. Results and Discussion: Mean serum sodium level was 136.43 ±6.3 mmol/l. Out of total 100 patients, isonatremia was seen in 72% patients, hyponatremia is seen in 23% patients. Hypernatremia was observed in 5% patients. Hypokalemia was seen in 6% patients. Decreased serum bicarbonate level was seen in 15% patients. Patients with severe dehydration had PH less than 7.35. Mean PH level was 7.38±0.6. Metabolic acidosis is associated with severe dehydration (p=0.01).
INTRODUCTION Diarrhoea is a global problem, but is especially prevalent in developing countries in conditions of poor environmental sanitation, inadequate water supplies, poverty and limited education.1 According to WHO, approximately one billion cases of diarrhoea occur each year worldwide causing a burden that was about 99.2 million DALYs (disability adjusted life years) lost (Bull World Health Organ 2003). Each year diarrhoea kills around 5,25,000 children under five. Globally, there are nearly 1.7 billion cases of childhood diarrhoeal disease every year (WHO May 2, 2017).2 Diarrhoea is the third leading cause of childhood mortality in India, and responsible for 13% of all deaths/year in children under 5 year of age. Diarrhoea accounts for 21% of all diseases causing deaths at below five years of age and causes 2.5 million deaths per year, although diarrhoea morbidity remains relatively unchanged, about one billion episodes or 3.2 episodes per child-year.3-5 The aetiology of acute gastroenteritis variable with two main entities: infectious and non-infectious, with the former being the most common.6 Diarrhoea can be caused by a variety of bacterial, viral and parasitic organisms. Infection is spread through contaminated food or drinking water, or from person-to-person as a result of poor hygiene.7,8 In addition, many time this number have long-term, lasting effects on nutritional status, growth, fitness, cognition, and schoolperformance.9 Some studies have revealed the impact of diarrhoea on growth.10-12 However, in clinical settings, the degree of dehydration is often classified as no, some or severe based on the estimated fluid loss and other clinical parameters. 13 In the same vein, altered biochemical parameters have also been found to be closely related to prognosis.12 When assessed at admission, these biochemical parameters provide valuable information for the optimal and specific management of the patient. Dehydration, acid base and electrolyte imbalance are common complications of acute diarrhoeal disease in children. This is because children exhibit major physiologic differences from adults in their total body surface area, immature renal structures, endocrine systems and higher metabolic rate. Each of these factors predisposes them to developmental variations in fluid and electrolyte balance.7 Presence of different types of electrolyte disorders is associated with significant increase in mortality rates among children with diarrhoea. Electrolyte disorders may remain unrecognized and result in increased morbidity and mortality. Timely recognition, a high index of suspicion and a thorough understanding of common electrolyte abnormalities is necessary to ensure their correction. Present study was conducted to see the electrolyte and acid base disturbances in acute gastrointestinal diseases in children Aim and objective: To study the electrolyte and acid base disturbances in acute gastrointestinal diseases in children.
MATERIAL AND METHODS Present study was a prospective study carried out in paediatric department at a tertiary health care centre. Study population was paediatric patients admitted in paediatric ward with diarrhoea. Inclusion criteria: 1. Paediatric patients admitted in paediatric ward with diarrhoea age > 1 month and below 14 years Exclusion criteria: 1. Children with acute gastroenteritis with non-infective etiology 2. Children with chronic diarrhoea 3. Children with HIV Study was approved by ethical committee of the institute. A valid written consent was taken from parents of patients after explaining study to them. Data was collected with pre tested questionnaire. Information was obtained from parents/guardians of children. Data included sociodemographic data like age, sex. Detailed clinical history was noted. Detailed clinical history including associated symptoms was noted and history regarding urine output in last 24 hours was noted. Systemic examination of patients was done with assessment of severity of dehydration, sensorium of patient, nutritional status and immunization status were noted in preformed proforma. Laboratory investigation like Hemogram, Sr. Sodium, Sr. Potassium, Sr. Creatinine and Sr. Urea and ABGA analysis were done. Serum Sodium below 135 mmol/l, above 145 mmol/l, defined as hyponatraemia, hypernatraemia, respectively. Potassium levels below 3.5 mmol/l and above 5.5 mmol/l were categorized as hypokalemia and hyperkalemia, respectively. Serum bicarbonate below 20mmol/l was Metabolic acidosis, 20-28mmol/l is Normal and above 28mmol/l was considered as Metabolic alkalosis. pH below 7.35 was considered as Metabolic acidosis, pH of 7.35-7.45 was Normal and pH above 7.45 was considered as Metabolic alkalosis. All the patients were treated according to WHO guidelines for treatment of diarrhoea. The electrolyte abnormalities and acid base abnormalities detected were treated according to standard treatment. Data was entered in excel sheet. Data was analysed with SPSS version 23.
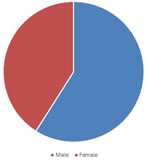
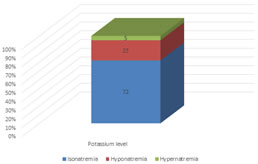
RESULTS Table 1 shows distribution of patients according to age group. Majority of the patients were from the age group of 1-5 year (51%) followed by 5-14 years (39%). Patients below 1 year were 10% of total study population. In our study, 59% patients were male and 41% were female. Male to female ratio was1.43:1. In our study, all patients complained of increased frequency of stool. vomiting was observed in 71% patients. Fever was recorded in 45% patients. other presenting complaints were not able to drink (10%), decreased urine output (9%), increased efforts of breathing (8%), altered sensorium (3%) and convulsions (2%). Out of total 100 patients, 83% patients had some dehydration and 17% had severe dehydration. Mean serum sodium level was 136.43 ±6.3 mmol/l. Out of total 100 patients, isonatremia was seen in 72% patients, hyponatremia is seen in 23% patients. Hypernatremia was observed in 5% patients. (fig 2) Table 4 shows distribution of patients according to Potassium level. In our study, potassium level was normal. Hypokalemia was seen in 6% patients. Hyperkalemia was not observed in any of the patients. Mean serum potassium level was 3.78± 0.5mmol/l. Mean bicarbonate level in our study was 20.81±0.6 mmol/l. 85% of the study population had normal bicarbonate level. Decreased serum bicarbonate level was seen in 15% patients. Table 6 shows distribution of patients according to PH and severity of dehydration. 86% of patients had PH of 7.35-7.45. Patients with severe dehydration had PH less than 7.35. Out of 100 patients, 9% patients had PH ranging from 7.25-7.35. Patients with PH less than 7.25 contributed 5% of study population. Mean PH level was 7.38±0.6. Metabolic acidosis is associated with severe dehydration (p=0.01). Table 1: Distribution of patients according to age group
Figure 1: Distribution of patients according to age group
Table 2: Distribution of patients according to presenting complaints
Table 3: Distribution of patients according to severity of dehydration
Figure 2: Distribution of patients according to Potassium level
Table 4: Distribution of patients according to age potassium level
Table 5: Distribution of patients according to Bicarbonate level
Table 6: Distribution of patients according to PH and severity of dehydration
DISCUSSION Majority of the patients were from the age group of 1-5 year (51%) followed by 5-14 years (39%). Patients below 1 year were 10% of total study population. Similar results were seen in the study done by Ritika Ghosh Dastidar et al.15reported acute gastroenteritis among 11.5%, 44%, and 44.5% respectively in the infants, 1-5 yrs, and >5 yrs age group. In our study, 59% patients were male and 41% were female. Male to female ratio was1.43:1. Similar results were seen in Ritika Ghosh Dastidar et al.15and Srivastava et al.16 In our study, all patients complained of increased frequency of stool. vomiting was observed in 71% patients. Fever was recorded in 45% patients. Other presenting complaints were not able to drink (10%), decreased urine output (9%), increased efforts of breathing (8%), altered sensorium (3%) and convulsions (2%). This was similar to the study conducted by Dr.Bela H Shah et al. 17 reported, majority of cases had increased frequency of stools 150 (100%), vomiting 108 (72%), least common complaint was altered sensorium 06 (04%). Convulsions with gastroenteritis are commonly observed in infancy and childhood, to the extent that it is a familiar phenomenon among pediatric neurologists and general pediatricians.18,19 Out of total 100 patients, 83% patients had some dehydration and 17% had severe dehydration in our study. The findings were in contrary to study done by Mittal et al.20 who has reported 50.52%of moderate dehydration and 21.95% severe dehydration in their study. But similar with the study reported by Ritika Ghosh Dastidar et al. 15 who revealed 166 (83%) of the children had moderate degree of dehydration and 34 (17%) children had severe dehydration. In our study, isonatremia was seen in 72% patients, hyponatremia is seen in 23% patients. Hypernatremia was observed in 5% patients. Similar findings were reported by Ritika Ghosh Dastidar et al.15 who in their study found isonatremic dehydration as the commonest 71.5%, followed by Hyponatremic dehydration 22% and Hypernatremic dehydration 6.5%. Gauchan E et al.21 reported that isonatremic dehydration 70.66% was the predominant one, followed by hypernatremic and hyponatremic dehydration was 19.34% and 10.00% respectively. Mean serum potassium level was 3.78± 0.5mmol/l. Majority of the cases in the study had normokalemia followed by hypokalemia. Approximately similar results were shown by Ritika Ghosh Dastidar,15 they found 170 children (85%) had normokalemia and 30 cases (15%) had hypokalemia and none of the cases had hyperkalemia. Mean bicarbonate level in our study was 20.81±0.6 mmol/l. 85% of the study population had normal bicarbonate level. Decreased serum bicarbonate level was seen in 15% patients. Dr.Bela H Shah 17conducted a study showed that 17% cases of severe dehydration had reduction in bicarbonate level. Patients with severe dehydration had PH less than 7.35. Out of 100 patients, 9% patients had PH ranging from 7.25-7.35. Patients with PH less than 7.25 contributed 5% of study population. Mean PH level was 7.38±0.6. Metabolic acidosis is associated with severe dehydration (p=0.01). The study conducted by Marin del Barrio S et al. 22 hadabnormal results were seen in 77.9% of cases mainly metabolic acidosis which was high compared to the present study.
CONCLUSION Most common electrolyte imbalance in acute gastroenteritis is hyponatremia followed by hypernatremia and hypokalemia. Metabolic acidosis is common in severe dehydration compared to some dehydration.
REFERENCES
Policy for Articles with Open Access: Authors who publish with MedPulse International Journal of Pediatrics (Print ISSN: 2579-0897) (Online ISSN: 2636-4662) agree to the following terms: Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution License that allows others to share the work with an acknowledgement of the work's authorship and initial publication in this journal. Authors are permitted and encouraged to post links to their work online (e.g., in institutional repositories or on their website) prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work.
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home