|
Table of Content - Volume 18 Issue 3- June 2021
A study of clinical profile and spectrum of functional disability in children with cerebral palsy
Shivprasad Kachrulal Mundada1, Deepak Khushalrao Jaybhaye2*, Vikas Narayan Solunke3
1Professor and HOD, 2PG Resident, 3Associate Professor, Department of Pediatrics, Vilasrao Deshmukh Government Institute of Medical Sciences, Latur, Maharashtra, INDIA. Email: djaybhaye7@gmail.com
Abstract Background: Cerebral Palsy is one of the common motor disorder observed in children. Cerebral palsy has major impact on life of patient as it affects physical, social and economic condition of the patient. Aim and objective: To study the clinical profile and spectrum of functional disability in children with cerebral palsy. Methodology: Present study was a cross sectional study carried out on 84 patients with cerebral palsy from paediatric Outpatient and Inpatient department. Data collected was demographic data, clinical features and functional disability. Assessment of Motor Impairment was assessed by Gross Motor Function Classification System (GMFCS). Data analysed with appropriate statistical tests. Results and Discussion: Spastic type (90%) of cerebral palsy was the most common clinical type. Quadriplegia (54.7%) was the most common topographical type of spastic cerebral palsy followed by diplegia (22.6%). 47.6% of children in this study had seizure disorder. Of these 50% had generalized tonic clonic seizure followed by myoclonic seizure (30%). 52.3% were Class III according to gross motor classification (GMFC).
INTRODUCTION Cerebral palsy is primarily a disorder of movement and posture. It is defined as an - "umbrella term covering a group of non-progressive but often changing, motor impairment syndromes secondary to lesions or anomalies of the brain arising in the early stages of its development". It may be explicit as a static encephalopathy in which, even though the first lesion, anomaly or injury is static, the clinical pattern of presentation may change over the period due to growth and developmental plasticity and maturation of the central nervous system.1 Worldwide incidence of CP being 2 to 2.5 per 1000 live births. Recent advances in neonatal management and obstetric care have not shown a decrease in the incidence of CP. On the contrary, with a decrease in infant mortality rate there has actually been an increase in the incidence and severity of CP. The incidence in India is approximately 1-2 per 1000 live births.2 The symptoms of the cerebral palsy depend on the clinical type of the neuromotor deficit. Usually symptoms such as abnormality of movement, posture and delayed milestones are noticed by parents only after the first six months of life of their child, indicating the presence of cerebral palsy. Clinically cerebral palsy can be spastic, atonic, dyskinetic or ataxic type. Depending on type of involvement spastic type can be quadriplegic, diplegic, triplegic, monoplegic, hemiplegic or double hemiplegic.3 For some children who have cerebral palsy, there appears to be no single event but rather, a sequence of events, responsible for the motor damage. This has led to the concept of “causal pathway”-a sequence of interdependent events that culminate in disease. Risk factors may be present before and during pregnancy, during labour and birth, and in period shortly after birth.4 The Gross Motor Functional Classification System has shown particular utility in clarifying prognosis as functional levels have been shown to be fairly stable over time and are very helpful in research. CP children are more likely to underweight and short as compared to peers 5 most evidence in regards to stature. 6 Because of chronic underweight short stature is common. Adequate assessment of growth status can be difficult in this population. Parents are the primary care givers for a child. Care of a CP child requires more attention and longer duration of care compared to care of normal children. As CP is an important problem with physical, social and economic effects in life of a person functional disability should be studied in detail. Present study was conducted to study the clinical profile and spectrum of functional disability in children with Cerebral Palsy. Aim and objective: To study the clinical profile and spectrum of functional disability in children with cerebral palsy
MATERIAL AND METHODS Present study was a cross sectional study carried out on patients with cerebral palsy from paediatric Outpatient and Inpatient department. Inclusion criteria: 1. All patients of cerebral palsy attending the department of Pediatrics 2. Children up to 12 yrs of age. Exclusion criteria: 1.Children with non-central causes of motor deficits 2. Parents of those children not willing to participate in the study Study was approved by ethical committee of the institute. A valid written consent was taken from the parents of children after explaining study to them. After considering inclusion and exclusion criteria 84 children were selected for the study. Data was collected with pre designed and pre tested questionnaire. Data was collected with pretested questionnaire. Data included demographic data, clinical features. Cerebral palsy was diagnosed with developmental milestones and a thorough neurological examination and observation of the child in various positions such as supine, prone, sitting, standing, walking and running was made. Based on the type of neuromuscular deficit CP classified in to spastic, dyskinetic (inclusive of choreoathetoid and dystonic), ataxic, hypotonic and mixed. Type of spastic cerebral palsy further classified on topographic involvement. Complete evaluation of CP child includes an assessment of associated problems in vision, speech and hearing, epilepsy and cognitive functioning, orthopedic evaluation and psychiatric assessment. EEG was indicated in children presenting with seizures, history of neonatal seizures, underlying malformation or lesion of brain found on neuroimaging and during follow-up. Assessment of Motor Impairment was assessed by Gross Motor Function Classification System (GMFCS). The GMFCS describes the functional characteristics in five classes from 1 to 5, class 1 being the mildest in the following age groups: up to 2 years, 2 - 4 years, 4 - 6 years and between 6 to 12 years. For each class, separate descriptions are provided. Children in class 3 usually require orthoses and assisting mobility devices, while children in class 2 do not require assisting mobility devices after age 4. Children in class 3 sit independently, have independent floor mobility and walk with assisting mobility devices. In class 4, affected children function in supported sitting but independent mobility is very limited. Children in class 5 lack independence even in basic antigravity postural control and need power mobility. The Denver Developmental Screening test was used to assess 4 parameters: Gross motor, fine motor, language and social development. Dangling toy test was used for assessment of vision. The convergence test for ocular dyspraxia was performed. Eye examination was done for presence of strabismus and refractive error. The fundus examination after pupil dilatation was done. Impendence audiometry was performed to look for any pathology in the middle ear. The use of brain stem-evoked studies (BERA) was done if information obtained from other hearing test was inconclusive. The assessment of nutritional status was done using the IAP (Indian Academy of Pediatrics) classification for malnutrition. Microcephaly was defined as head circumference less than third centile for the age. Data was entered in excel sheet and analysed with appropriate statistical tests.
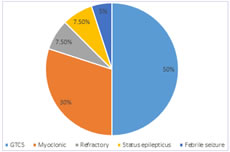
RESULTS In this study majority of patients (52%) were in 2-5 years of age group followed by less than 2 years and more than 5 years. In our study male patients (55.95%) were more than female (44.05%). Male to female ratio was 1.27:1. Maternal age (32.14%), severe asphyxia (76.2%), Neonatal hyperbilirubinemia as most common prenatal, perinatal and postnatal risk factor respectively. Most commonly observed clinical type of cerebral palsy was spastic quadriplegia (54.7%) followed by spastic diplegia (22.6%). Similar findings were seen in males and females. Prevalence of spastic quadriplegia was observed more in females (64.8%) than males (46.8%). Spastic diplegia was more prevalent in males (25.5%) than females (18.9%). In total patients spastic double hemiplegia was observed in 11.9% patients, whereas it was observed in 17% and 5.4% in males and females respectively. Spastic monoplegia and hypotonia were least observed clinical type in both the genders. Hypotonia was not observed in females. (table 1) Assessment of Motor Impairment was assessed by Gross Motor Function Classification System (GMFCS). Majority of the patients were in class 5(38%) followed by class 4(26%). 21.4% were in class 3 and 9.5% in class 2. Only 4 (4.7%) patients were in class 1. Similar pattern was observed in males and females. (table 2) Majority children had grade1 (55.9%) and grade 2(29.7%) whereas 3.5% had grade 3. 10% had normal nutritional status. Malnutrition in female (94.5%) was more compared to male (89.2%). (table 3) Microcephaly was observed in 78.5% patients and 21.4% had normal circumference. In male patients 87.2% children had microcephaly and 12.8% had normal head circumference. In female patients 67.5% had microcephaly and 32.5% had normal head circumference. (table 4) In our study, 47.6% of children with cerebral palsy in this study had seizure disorder. Among them 50% were generalized tonic clonic seizure, myoclonic seizure (30%), refractory seizure (7.5%), status epilepticus (7.5%) and febrile seizure (5%). Most commonly observed seizure was Generalized tonic clonic seizure. (fig 1)
Table 1: Distribution of CP children according to clinical type and sex
Table 2: Distribution of CP children according to GMFCS class and sex
Table 3: Distribution of CP children according to nutritional status and sex
Table 4: Distribution of CP children according to head circumference and sex
Figure 1: Distribution of CP children according to seizures DISCUSSION In this study majority of patients (52%) were in 2-5 years of age group followed by less than 2 years and more than 5 years. In a study by Kondle et al.7 also showed most patient presented at age of 1-5 years. In our study Male to female ratio was 1.27:1 similar results were seen in Nabanita Das et al.8 In our study, Maternal age (32.14%), severe asphyxia (76.2%), Neonatal hyperbilirubinemia were most common prenatal, perinatal and postnatal risk factor respectively. Similar observation was found in study by Nabanita Das et al.8 and Anant Bendale et al.9 In this study among the spastic group, quadriplegias were 55%, diplegia 22%, monoplegia 1% and double hemiplegia 12%. There are other comparable studies Kondle et al. 7, P.Singhi et al.10, Bendle et al.9 showed spastic cerebral palsy was the commonest type. Study by P. Singhi et al.10 compared two groups of children with CP during two decades, showed quadriplegic CP is most common in their set up with a trend towards increase in diplegic and decrease in the quadriplegic CP. Similarly, Study by Nonica Laisaram et al.11 showed proportion of diplegic has increased being most common spastic type and quadriplegia has decreased showing an evolving clinical spectrum of CP in developing countries. Clinical profile of CP in developing countries is different from that in developed countries. With advancement in maternal and neonatal care and trend of increasing survival of preterm babies in developing countries clinical profile in developing countries is showing a gradual change.11 In our study GMCSF class was used for assessment of motor system. Majority were in class 4 and class 5 (64.2%). Only 15.4% of class 3 followed by class1 and class 2 (10.7%). Similar observation in study by Hongbo Zhang et al.12 showed maximum patient were of class 4 and class 5 (37.5%) followed by class 1,2 (35.5%) and class 3 (27%). GMFCS has been validated as a reliable instrument to classify the severity of gross motor dysfunction in cerebral palsy cases across different age bands. In children with cerebral palsy, health related quality of life is closely related to motor function and intellectual ability. Hence cerebral palsy therapy should focus on restoration of motor and intellectual functions, especially with the goal of being able to live and work independently. It is well known that the early onset of long term regular treatment is pivotal for children with cerebral palsy to obtain a desirable outcome. In our study, Majority were grade I malnourished (55.9%) and grade II malnutrition (29.7%), whereas 3.5% had grade III malnutrition. 10.3% patients had normal nutritional status as compared to study by Singhi Pratibha D et al.10 in which 50.6% were malnourished and 28.1% were severely malnourished. We found 78.5% children had microcephaly and only 21.5% had normal head circumference, whereas study by Singhi Pratibha D et al.10 showed (88.6%) with microcephaly. In this study, 47.6% of children with cerebral palsy in this study had seizure disorder. Among them 50% were generalized tonic clonic seizure, myoclonic seizure (30%), refractory seizure (7.5%), status epilepticus (7.5%) and febrile seizure (5%). In the study done by Singhi PD et al.10 they observed 105 children, 60% of these children with cerebral palsy had seizure disorder. Among them 52.08% were generalized tonic clonic seizure, myoclonic seizure were (20.83%), febrile seizure (12.5%), refractory seizure (8.33%). In study by Delgato et al. 13 reported that focal or secondarily generalized seizures were common in children with CP, whereas primary generalized epilepsies were less frequent. In contrast, Kwong et al.14 demonstrated that generalised epilepsies were less frequently observed in patient with CP, where polymorphic seizure type were more common. Similarly in present study more frequently partial seizure secondarily generalized were observed in CP patient. The presence of neurologic deficits was considered by many authors to be an unfavourable factor in seizure remission. Early prediction of intractable epilepsy would be valuable because rapid identification of patient at highest risk would allow physicians to consider them earlier for treatment with the recently approved medications and other surgical and non- surgical treatments. In this study the majority of patient had a severe form of CP and there is straight relationship between degree of severity and occurrence of epilepsy. Neonatal seizure and positive family history were a common finding associated with epilepsy and it is difficult to have seizure control in these patient. Although none of the patient of this study was submitted to surgery intervention, the new antiepileptic drugs and advances on surgery intervention are promising in improving the care of epileptic children with CP, offering a better quality of life and allowing the integration of these patients and their families in the society.14
CONCLUSION Cerebral palsy patients most commonly present with Spastic type and majority belong to Class III according to gross motor classification (GMFC).
REFERENCES
Policy for Articles with Open Access
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home `
`