|
Table of Content - Volume 18 Issue 3- June 2021
A comparative study of thyroid function tests in children with and without birth asphyxia
Shivprasad Kachrulal Mundada1, Nitin Narayan Ambekar2*
1Professor and HOD, 2PG Resident, Department of Pediatrics, Vilasrao Deshmukh Government Institute of Medical Sciences, Latur, Maharashtra, INDIA. Email: ambekar.nitin214@gmail.com
Abstract Background: Thyroid hormone play an important role in neurodevelopement. Hypoxia impairs thyroid function and causes reduction in T4 metabolism. Thyroid function tests in neonates with birth asphyxia should be studied for adequate treatment. Aim and objective: To compare the thyroid function tests in children with or without birth asphyxia Methodology: Present study was a cross sectional study conducted on 135 low birth weight neonates (<2Kg) admitted at a tertiary care centre. After obtaining thyroid function levels, all newborns were divided into two groups according to presence of birth asphyxia. Thyroid functions were compared in these two groups. Results and discussion: Prevalence of decreased T3 and T4 was higher in newborns with Birth Asphyxia (T3: 64%, T4: 70.5%) compared to those without Birth Asphyxia (T3:22.8%, T4:33.8%). Mean T3, T4 and TSH values were significantly low in newborns with Birth Asphyxia compared to newborns without Birth asphyxia.
INTRODUCTION India constitutes for around 40% of the total Low birth babies born worldwide. Of those total low birth weight babies 60% are born at term with small for gestational age and 40% are born preterm. Intrauterine growth restriction occurs as a result of complex maternal placental and foetal factors.1 Because of these changes SGA new-borns are chronically in stress. This stress leads to retarded development of the thyroid gland which may affect neurodevelopmental outcome. Hormone secreted by thyroid gland are Tri-iodothyronine (T3) and tetra- iodothyronine/Thyroxine (T4). T3 and T4 are iodine containing amino acids. Thyroid synthesis is carried out by complex molecular mechanism with distinctive steps.2 The embryogenesis of thyroid along with pituitary and hypothalamus is almost completed by 12 weeks of gestation. 3-5 However fetal HPT axis becomes functional by mid-gestation followed by proper thyroxine secretion. Until mid- gestation main source of fetal serum thyroxine is transplacental transfer from mother to fetus. 6,7 Most T3 and T4 transferred from mother is inactivated to T2 and rT3 respectively by placental D3. However, sufficient amounts of thyroid hormones reach fetus which are crucial for Central Nervous System development (CNS) till fetal thyroxine secretion starts.5,6,8 Birth Asphyxia is an insult to fetus or newborn due to failure to breath or breathing poorly leading to decreased oxygen perfusion to various organs.9 According to WHO, For intramural babies, birth asphyxia is defined as Apgar score less than 7 at 1 minute of age. For extramural babies, moderate birth asphyxia is slow gasping breathing at 1 minute of age and Severe birth asphyxia is No breathing at 1 minute of age.10 Incidence of birth asphyxia is 2/1000 live birth in developed world. However, incidence up to 20 per 1000 live birth is noted in the developing countries. Mortality is 15 to 20% in patients of perinatal asphyxia and 25% patients suffer from severe neurological sequelae. Many agents affect thyroid hormone concentrations by their action on different stages of metabolism. Little has been studied regarding thyroid hormones in birth asphyxia. Hypoxia impairs thyroid function and causes reduction in T4 metabolism. Many studies regarding thyroid hormones in birth asphyxia have given conflicting results. Some of the Studies revealed that IUGR fetuses have significantly lower levels of free T3 and free T4 with increase in levels of TSH. 11,12 Few Studies showed that TT4, TT3, FT3 values were lower in lower gestational group, while there was no significant difference for FT4 and TSH according to gestational age. 13,14 The levels of thyroid hormone in birth asphyxiated neonates needs to be studied hence present study was conducted to compare the thyroid function tests in children with or without birth asphyxia. Aim and objective: To compare the thyroid function tests in children with or without birth asphyxia
MATERIAL AND METHODS Present study was a cross sectional study conducted at Level III NICU at Tertiary care centre. All the low birth weight neonates (<2Kg) admitted at a tertiary care centre during the study period of 18 months were studied. Inclusion criteria: 1. All 3 day old neonates with birth weight <2 kg Exclusion criteria: 1.Neonates whose parents are not willing 2. Neonates who were discharged against medical advice Study was approved by ethical committee of the institute. A valid wriiten consent was taken from the parents of neonates after explaining study to them. A pilot study was conducted on 14 patients in which prevalence of hypothyroxinemia was found 42.85% Sample size was calculated according to formula (Sample size= Z2PQ/ L2 ). It came as 134. 15 Data was collected with pretested questionnaire by interviewing parents of neonates less than 2 kg weight at birth on 3rd day admitted at a tertiary care centre. Data included demographic data, Antenatal history, perinatal history, post-natal history, past medical history and clinical examination of the neonates. Investigations done in all neonates were T3, T4, TSH levels. After obtaining thyroid function levels, all newborns were divided into two groups according to presence of birth asphyxia. Thyroid functions were compared in these two groups. Hypothyroxinemia was defined as serum T4 concentrations below normal range with TSH levels within the normal range. 16 Reference range for T3 was 75-260 ng/dl and for T4 was 8.2 to 19.9 µg/dl. 177 we have taken self definition of increased TSH as TSH >12mIU/L as TSH >12 mIU/L is associated with poor neurodevelopmental outcome.17 The data were entered in Microsoft Excel and data analysis was done by using SPSS for windows. p<0.05 was considered as level of significance using the Chi-square test.
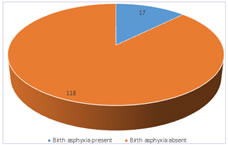
RESULTS We studied 135 neonates. Out of 135 newborns 6 (4.4%) were < 30 weeks of age, 65 (48.1%) newborns were between 30 to 35 weeks. 64 (47.4%) newborns were between 36 to 40 weeks of gestational age. In our study majority of the neonates were with birth weight of 1.5-2kg (56.3%) followed by 1.2- 1.5 kg (36.3%). Babies with birth weight of 1-1.19kg were 6.66%. One baby was with birth weight of less than 1 kg. In our study out of 135 neonates, 17 had birth asphyxia and 118 had no birth asphyxia. (fig 1) Out of total 17 patients with birth asphyxia, 11 (64.7%) had decreased T3 level and 6(35.3%) had normal T3 level. In patients with no birth asphyxia, 27(22.88%) had decreased T3 level and 91 (77.12%) had normal T3 level. Thus prevalence of decreased T3 level was observed more in patients with birth asphyxia than patients without birth asphyxia. This difference was statistically significant (p<0.05). Table 2 shows correlation between Birth Asphyxia and decreased T4 levels. In patients with birth asphyxia, 12 (70.59%) had decreased T4 levels and 5 (29.41%) had normal T4 levels. In patients with no birth asphyxia, 17(14.4%) had decreased T4 level and 101(85.6%) had normal T4 level. Thus, birth asphyxia was associated with significant decreased level of T4 (p<0.05). Table 3 shows mean T3, T4 and TSH levels in low birth weight neonates with and without birth asphyxia. Mean T3 level in patients with birth asphyxia was 93.08 ng/dl and in patients without birth asphyxia was 106.55 ng/dl. Mean T3 level was decreased in neonates with birth asphyxia. Mean T4 level was 8.71 µg/dl in neonates with birth asphyxia and 10.85 µg/dl in patients without birth asphyxia. Mean TSH level in neonates with and without birth asphyxia was 2.1 and 5.5 mIU/L respectively. Mean T3, T4 and TSH values are significantly lower in newborn with Birth Asphyxia compared to those without Birth Asphyxia.
Figure 1: Distribution of neonates according to presence of birth asphyxia
Table 1: Correlation of birth asphyxia with T3 levels in low birth weight neonates
Chi square P value 0.000337 statistically significant
Table 2: Correlation of birth asphyxia with T4 levels in low birth weight neonates
Chi square p value < 0.00001 statistically significant
Table 3: Mean T3, T4, TSH levels in low birth weight neonates with and without birth asphyxia
DISCUSSION In our study, prevalence of decreased T3 level was observed more in patients with birth asphyxia (64.7%) than patients without birth asphyxia (22.88%). In patients with birth asphyxia, 12 (70.59%) had decreased T4 levels and 5 (29.41%) had normal T4 levels. In patients with no birth asphyxia, 17(14.4%) had decreased T4 level and 101(85.6%) had normal T4 level. Thus, birth asphyxia was associated with significant decreased level of T4 (p<0.05). Mean T3 level in patients with birth asphyxia was 93.08 ng/dl and in patients without birth asphyxia was 106.55 ng/dl. Mean T3 level was decreased in neonates with birth asphyxia. Mean T4 level was 8.71 µg/dl in neonates with birth asphyxia and 10.85 µg/dl in patients without birth asphyxia. Mean TSH level in neonates with and without birth asphyxia was 2.1 and 5.5 mIU/L respectively. Mean T3, T4 and TSH values are significantly lower in newborn with Birth Asphyxia compared to those without Birth Asphyxia. In a study by Pereira DN et al., 34 neonates were studied and it showed significantly decreased T3, T4 and TSH levels in asphyxiated than non asphyxiated neonates (p<0.05). 18 Our findings also correlate with those of N Prabhakar et al. (2016).19 Kumar PS et al. studied 50 neonates in a case control study and found that T3, T4 and TSH levels at 24 hours was significantly lower in neonates with birth asphyxia than in patients without birth asphyxia.20 Borges et al.21 observed that in spite of TSH surge T4 and FT4 values failed to increase in neonates with birth asphyxia. In a prospective cross sectional study by Rashmi et al., 1590 neontes were studied for TSH levels and observed that TSH was significantly higher in asphyxiated neonates.22 Possible explanation for this decreased T3, T4 and TSH in newborns with Birth asphyxia is non-thyroidal illness syndrome. It is a type of combined hypothyroidism having both central and peripheral components. Many times, it is associated with other hormonal deficiencies. Also called as euthyroid sick syndrome, it is characterized by decreased T3 and T4 but without elevation of TSH. It occurs in protein energy malnutrition, postoperatively after major surgeries, sepsis and birth asphyxia.19 Decreased T3 and T4 concentrations are probably secondary to decreased TSH values. Alteration in thyroid hormone mechanism due to hypoxia can be another possible explanation. Moshang et al. found that in patients with acute hypoxia, rT3 levels were increased and in chronic hypoxia decreased T3 levels were present with increased rT3 levels. This suggested that there is decreased degradation of rT3 with increased conversion of T4 to rT3. 23
CONCLUSION Birth asphyxia significantly decreases serum T3, T4 and TSH levels so special emphasis should be given on thyroid function in LBW and asphyxiated newborns.
REFERENCES
Policy for Articles with Open Access
|
|
 Home
Home `
`