|
Table of Content - Volume 20 Issue 3 - December 2021
Study of prevalence of anaemia and haematological parameters in children below 12 years
Mohana
Professor, Department of Paediatrics, Akash Institute of Medical Sciences & Research Centre, Devanahalli, Bangalore - 562110, Karnataka, INDIA.
Email: mohanagm@yahoo.com
Abstract Background: Anaemia is a major global health problem; it results in significant morbidity and mortality among children Method: 85 children below 12 years having anaemia were studied. Complete blood count was done to determine PCV, MCV, MCH, MCHC, RDW, Hb %, along with Peripheral smear (PS) study, Reticulocyte count and Serum iron (Fe), Serum B12 and Folic acid levels were done Results: Types of anaemia were 50 (58.8%) Iron deficiency anaemia, 12 (14.1%) Thalassemia, 8 (9.41%) Megaloblastic anaemia, 7 (8.23%) Anaemia of acute haemorrhage, 5 (5.88%) Sickle cell anaemia, 2 (2.35%) Aplastic anaemia, 1 (1.17%) Leukemia. The clinical manifestations were 85 (100%) pallor, 71 (83.5%) weakness and fatigability, 32 (37.6%) fever, 23 (27.05%) 17 (20%) shortness of breath, 15 (17.6%) hepatomegaly, 12 (14.1%) cough, 11 (12.9%) history of pica, 11 (12.9%) spleenomegaly, 9 (10.5%) petechiae, 8 (9.4%) Nausea/vomiting, 8 (9.4%) koilonychia, 4 (4.7%) hyper pigmentation, 5 (5.8%) tremors. Out of the total number of patients screened 18 (21.1%) had mild, 39 (45.8%) moderate and 28 (32.9%) had severe anaemia. Conclusion: The present study of anaemia had Iron deficiency as the major cause followed by Thalassemia, Megaloblastic anaemia, acute Haemorrhage, Sickle cell anaemia and Aplastic anaemia. This study will be helpful to paediatricians to treat such patients efficiently to avoid morbidity and mortality.
Keywords: Haemoglobin, Iron deficiency, Thalassemia, Serum Fe, Serum B12
INTRODUCTION
Anaemia is a term used for all pathological conditions in which the blood haemoglobin concentration decreases to an abnormally low level, due to a deficiency in one or more micro nutrients. The main nutrients involved in the synthesis of haemoglobin are iron, folic acid, and vitamin B12. Anaemia is a serious health problem in India and under developed countries.1 About two million people (30% of world population) are anaemic and it’s mainly due to iron deficiency; in developing countries like India this figure is exacerbated by malaria worm infestations and mal-nutrition.2 As per the NFHS (National Family Health survey) report prevalence of anaemia among children less than 12 years of age is 60-70%.3 Anaemia usually develops as breast milk is replaced by food that are deficient in micro nutrients including iron, vitamin B12 and folic acid, during early childhood, bad feeding habits, especially during weaning period, exacerbate the problem. Impaired cognitive function, growth and psychomotor development are the manifestation of anaemia in children (4). Hence an attempt was made to evaluate the clinical manifestations, grades of anaemia in different age groups so that the study will be a guide line for paediatricians.
MATERIAL AND METHODS
85 (Eighty-Five) children aged below 12 regularly visiting to paediatric OPD of Akash Institute of Medical Sciences and research centre, Devanhalli, Bangalore-562110 were studied.
Inclusive Criteria: Children between the age group of 6 months to 12 years with pallor clinically diagnosed as anaemia were selected for study.
Exclusion Criteria: Children more than 12 years, less than 6 months, children with congenital heart disease, immune compromised, tuberculosis and hepatitis were excluded from study.
Method: Routine blood examination for anaemia was morphologically based on peripheral smear (PS) findings packed cell volume (PCV), Mean corpuscular volume (MCV), Mean corpuscular haemoglobin (MCH), Mean corpuscular haemoglobin Concentration (MCHC) and red cell distribution width (RDW) were determined by automated cell counter Haemoglobin was estimated by sahil’s method and expressed in gm%, PS (peripheral smear) was stained by Leishman’s stain. Retilculocyte count was done by Brilliant crystal stain method; serum iron determination was done by Romany’s bipyridyl method. Total iron binding capacity was determined by Ramsay’e method, serum vitamin B12 and folic acid was determined by architect method. The duration of study was June-2020 to July-2021
Statistical analysis: Various findings including different types of anaemia, clinical manifestations, grades of anaemia were classified with percentage. The statistical analysis was done in the SPSS software. The ratio of male and female was 2:1.
OBSERVATION AND RESULTS
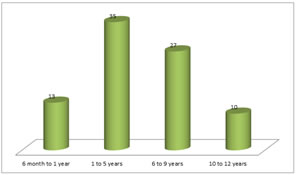
Table-1: Age wise distribution of paediatric patients – 13 (15.2%) patients were between 6 months to 1 year, 35 (41.1%) were 1 to 5 years, 27 (51.7%) was between 6 to 9 years, 10 (11.7%) were 10 to 12 years of age.
Table 1: (Total No. of patients: 85) Age wise distribution of patients of anaemia
| Age in years |
- No. of patients
|
- Percentage %
|
| 6 month to 1 year |
- 13
|
- 15.2
|
| 1 to 5 years |
- 35
|
- 41.1
|
- 6 to 9 years
|
- 27
|
- 31.7
|
- 10 to 12 years
|
- 10
|
- 11.7
|
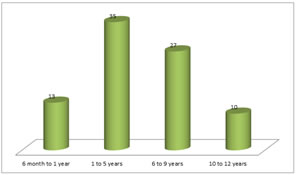
Table 1: Age wise distribution of patients of anaemia
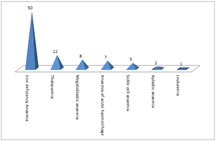
Table-2: Prevalence of different types of Anaemia 50 (58.8%) Iron deficiency, 12 (14.1%) thalassamia, 8 (9.4%) megaloblastic anaemia, 7 (8.23%) anaemia of acute haemorrhage, 5 (5.88%) sickle cell anaemia, 2 (2.55%) were aplastic anaemia, 1 (1.4%) leukaemia.
Table 2: Prevalence of different types of Anaemia
- Diseases
|
- No. of patients
|
- Percentage %
|
- Iron deficiency Anaemia
|
- 50
|
- 58.8
|
- Thalassemia
|
- 12
|
- 14.1
|
- Megaloblastic anaemia
|
- 8
|
- 9.41
|
- Anaemia of acute haemorrhage
|
- 7
|
- 8.23
|
- Sickle cell anaemia
|
- 5
|
- 5.8
|
- Aplastic anaemia
|
- 2
|
- 2.35
|
- Leukaemia
|
- 1
|
- 1.17
|
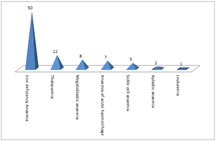
Table 2: Prevalence of different types of Anaemia
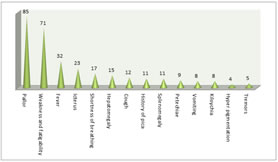
Table-3: Clinical manifestations of Anaemic patients 85 (100%) had pallor, 71 (83.5%) weakness and fatigability, 32 (37.6%) fever, 23 (27.05%) Icterus, 17 (20%) shortness of breath, 15 (17.6%) hepatomegaly, 12 (14.1%) cough, 11 (12.9%) History of pica, 11 (12.9%) spleenomegaly, 9 (10.5%) petechiae, 8 (9.4%) nausea/vomiting, 8 (9.4%) koilonychia, 4 (4.7%) hyper pigmentation, 5 (5.8%) tremors
Table 3: Clinical Manifestations in Anaemia patients
- Clinical Manifestations
|
- No. of Patients
|
- Percentage %
|
- Pallor
|
- 85
|
- 100
|
- Weakness and fatigability
|
- 71
|
- 83.5
|
- Fever
|
- 32
|
- 37.6
|
- Icterus
|
- 23
|
- 27.05
|
- Shortness of breath
|
- 17
|
- 20
|
- Hepatomegaly
|
- 15
|
- 17.6
|
- Cough
|
- 12
|
- 14.1
|
- History of pica
|
- 11
|
- 12.9
|
- Splenomegaly
|
- 11
|
- 12.9
|
- Petechiae
|
- 9
|
- 10.5
|
- Nausea/Vomiting
|
- 8
|
- 9.4
|
- Koilonychia
|
- 8
|
- 9.4
|
- Hyper pigmentation
|
- 4
|
- 4.7
|
- Tremors
|
- 5
|
- 5.8
|
-
-
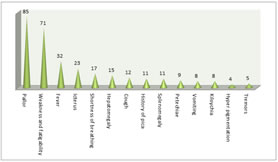
- Table 3: Clinical Manifestations in Anaemia patients
-
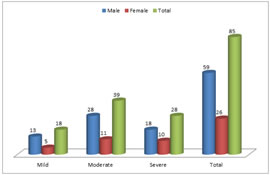
- Table-4: Grades of Anaemia on the basis of haemoglobin level – Mild 13 male, 5 female, total 18 (21.1%), Moderate 28 male, 11 female, total 39 (45.8%) severe 18 male, 10 female, total 28 (32.9%).
- Table 4: Grades of Anaemia on the basis of haemoglobin level
- Grades of anaemia
|
- Male
|
- Female
|
- Total
|
- Percentage %
|
- Mild
|
- 13
|
- 5
|
- 18
|
- 21.1
|
- Moderate
|
- 28
|
- 11
|
- 39
|
- 45.8
|
- Severe
|
- 18
|
- 10
|
- 28
|
- 32.9
|
- Total
|
- 59
|
- 26
|
- 85
|
- 100
|
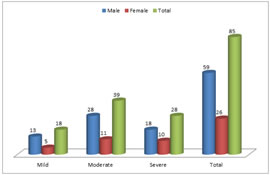
Table 4: Grades of Anaemia on the basis of haemoglobin level
-
- DISCUSSION
- In the present study of prevalence of anaemia and haematological parameters in children below 12 years – 13 (15.2%) children were between 6 months to 1 year, 35 (41.1%) were between 1 to 8 years, 27 (31.7%) were aged between 6 to 9 years, and 10 (11.7%) were between 10 to 12 years (Table-1). Types of anaemia were 50 (58.8%) had iron deficiency 12 (14.1%) had thalssemia, 8 (9.4%) had megaloblastic anaemia, 7 (8.23%) had anaemia of acute haemorrhage, 5 (5.88%) had sickle cell anaemia, 2 (2.35%) had aplastic anaemia, 1 (1.17%) had leukaemia (Table-2). The clinical manifestation included 85 (100%) pallor, 71 (83.5%) weakness and fatigability, 32 (37.6%) had fever, 23 (27.05%) Icterus, 17 (20%) had shortness of breath, 15 (17.6%) hepatomegaly, 12 (14.1%) had cough, 11 (12.9%) had history of pica, 11 (12.9%) had spleenomegaly, 9 (10.9%) had petechae, 8 (9.4%) had nausea/vomiting, 8 (9.4%) koilonychia, 4 (4.7%) hyper-pigmentation, 5 (5.8%) had tremors (Table-3). 18 (21.1%) had mild, 39 (45.8%) moderate, 28 (32.9%) had severe grade of anaemia (Table-4). These findings are more or less in agreement with previous studies.5,6,7 During the study of anaemia in paediatric patients included pertinent issues, related to the history, physical examination and initial laboratory investigations, Hematocrit, (HCT) is the fractional volume of whole blood sample occupied by RBC expressed as percentage. As an example the normal HCT in children from 6 months to 12 years is approximately 40% and Haemoglobin in children of 6 months to 12 years is approximately 13.5 g/dL (135 g/L). Characterising the symptoms help to elucidate the severity and chronicity of anaemia and may identify patients with blood loss or haemolytic aetiologies. Common symptoms of anaemia include lethargy, tachycardia and pallor (8). Infants with anaemia may present with irritability and poor oral intake. Changes in urine colour, scleral icterus or jaundice may indicate the presence of haemolytic disorders, such as G6PD (glucose 6-phosphate dehydrogenase) deficiency. Bleeding from GIT (gastro-intestinal tract) includes changes in stool colour; identification of blood in stool, history of bleeding symptoms must be reviewed. Severe or chronic epistaxis also may result in anaemia from blood loss and iron deficiency. Previous medical history also plays vital role to find out the cause of anaemia in children, duration of gestational age at birth, hospitalisation and history of jaundice and / or anaemia in the new born period. Travel to / from areas of endemic infections (Eg. Malaria, hepatitis, tuberculosis) should also be ruled out to evaluate the cause of anaemia. Moreover herbal or oxidant drugs may cause haemolysis particularly in patients with G6PD deficiency, possible environmental toxins exposure should be explored including lead exposure and nitrates in well water, family history of inherited haemolytic anaemia.9 Anaemia with high absolute reticulocyte count (ARC) reflects an increased erythropoietic response for haemolysis or loss of blood. Anaemia with a low or normal ARC reflects deficient production of RBC (i.e. reduced bone morrow response to anaemia). However, haemolysis or blood loss can be associated with low concurrent disorder that impairs RBC production. In some cases reticulocyte count depends on the phase of illness.10 Review of PS (peripheral smear) is an essential part of anaemia evaluation. Even if patients RBC indices are normal review of the blood smear may reveal abnormal cells that can help to identify the cause of anaemia. The diagnostic approach to anaemia includes pancytopenia in leukaemia, thrombocytopenia indicate haemolytic uremic syndrome and thrombocytosis in iron deficiency, leukocytosis or elevated WBC count includes leukaemia and infections.SUMMARY AND CONCLUSION
- The present study of anaemia in children below 12 years of age is mainly related to malnutrition. The prevalence of high lymphocyte count in anaemia indicates viral infection. The prevalence of anaemia was higher in the lower age group is due to frequent infections. Girls of preschool age had a probable iron, vitamin B12 or foliate deficiency as indicated by high RDW values. Girls of adolescent age (11-12 years) were more anaemic indicating more nutritional requirement with onset of puberty. Overall children below 12 years boys were found to be suffering from higher level of hypochromic and microcytic anaemia. The present study recommends about pure drinking water, sanitation and nutritional counselling to the parents having low social economic status.
- Limitation of study: Owing to tertiary location of present institution, limited number of patients, lack of latest (advanced) instruments we have limited findings.
- REFERENCES
- Slotzfus RJ, Dreyfus ML – Nutrition foundation; A draft document prepared for the international Nutritional Anaemia consultative group (INCAG) 17th July 1997 Geneva.
- World health organisation Switzerland WHO 2008, Global burden of diseases 2004 update WHO 20, Avenue Appia 12
- National family health survey for Indian conducted by Mumbai, India. International Institute for population science 2006, N. F, H. S. 3rd.
- Notional family health survey India International Institute for population science 1999, N.F.H.S. 2nd.
- Silva D G, France schini SC – Anaemia ferro private meriandasnarede publica de saude do municipio de vicasa minas Gerais. Rev. Nutr. 2002, 15 (3); 301-8.
- Santosh Kumar, Jayant Prakash – Prevalence of anaemia under five years old children. A cross sectional hospital based study – Int. J. of contemporary Medicine 2018, vol. 6(2); 52-57.
- Piel FB, Patil AP – Global epidemiology of Sickle haemoglobin in neonates. Lancet 2013, 38 (1); 142-51.
- Panigrahi S, Patra PK – The screening and morbidity pattern of anaemia in chattisgarh. Ind. J. Haotol. Blood Transfus. 2015; 31 (1); 104-9.
- Madoori S, Ramya C – Clinico- haematological profile and outcome of anaemia in children at tertiary care hospital Karim Nagar, Int. J. Res. Med. Sci. 2015, 3; 3567-71.
- Meshram SA – A hospital based study of anaemia in children of Adilabad a tribal district of Andhra Pradesh Int. J. Biol. Med. Res. 2013, 4 (1); 2894-7.
Policy for Articles with Open Access
Authors who publish with MedPulse International Journal of Anesthesiology (Print ISSN:2579-0900) (Online ISSN: 2636-4654) agree to the following terms:
Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution License that allows others to share the work with an acknowledgement of the work's authorship and initial publication in this journal.
Authors are permitted and encouraged to post links to their work online (e.g., in institutional repositories or on their website) prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work.
|
|
 Home
Home