Official Journals By StatPerson Publication
|
Table of Content - Volume 9 Issue 1 - January 2019
Reliability and validity of clinical signs for anemia detection in school children
S Srikrishna1*, K Nagendra Prasad2, Natasha Ahmad3, Ravi kiran M4, Ajay Kumar Reddy Bobba5
1Associate Professor, Department of Paediatrics, Apollo Medical College, Hyderabad, Telangana, INDIA 2Associate Professor, Department of Paediatrics, Santhiram Medical College, Nandyal, Kurnool, AP, INDIA. 3Senoir Resident, Department of Paediatrics, Nice hospital, Hyderabad, Telangana, INDIA. 4,5Assistant Professor, Department of Community Medicine, ASRAM Medical College, Eluru, AP, INDIA. Email:
Abstract Anemia is widely prevalent in developing world and also is a public health challenge in India. It is a serious concern because it can result in impaired cognitive performance, behavioural and motor development, coordination, language development, and scholastic performance. It also leads to increased morbidity from infectious diseases. The present study was designed to evaluate the accuracy and reliability of clinical signs in children by studying their sensitivity and specificity in comparison to haemoglobin assessment in diagnosis of anaemia and to study the inter-observer agreement of pallor examination to diagnose anaemia in urban school children 6-14 years of age in this region. An Observational cross- sectional study was conducted among school children aged 6–14 years in urban government schools from January 2017 to January 2018. In this study, 450 urban government school children in age group of 6-14 years were included and they were observed by two separate doctors for clinical signs of Anemia. 54 students were excluded. The incidence of Anemia was 60% i.e. 237 children out of 394. Both doctors found that palmar pallor had highest sensitivity when Anemia was severe. The sensitivity for mild and moderate was quite low. Specificity of all sites was high and for severe pallor was 100%. Fleiss Kappa was used as a measure to review inter observer reliability at the different sites. It is to be noted that the Kappa for all sites are above 0.8 which indicates an almost perfect agreement on the pallor between the 2 observers. In the present study, the prevalence of Anemia was high in school children. According to the present study conjunctiva and palm were the most sensitive to assess the severity of Anemia. Clinical assessment of pallor can be used as initial screening tool for diagnosing Anemia in school children especially in places where prevalence in high and early incorporation of treatment. Key Word: Anemia, Conjunctiva pallor, Palmar pallor, School Children.
INTRODUCTION Anemia is highly prevalent in children of developing countries. It is associated with impaired physical growth and mental development. It is also associated with a higher risk of infant and child mortality, particularly when it co-exists with malnutrition and other risk factors. It is therefore important to make a timely and accurate diagnosis and initiate an early intervention to reduce the negative impact of anemia. The laboratory diagnosis of anemia through any of several techniques is not widely available and its cost is often unaffordable in poor areas of the world. These challenges have encouraged several studies to assess the accuracy of clinical signs for screening of anemia.1,2 According to the World Health Organization (WHO), there are two billion people with anemia in the world and half of the anemia is due to iron deficiency. Of these, 9 of 10 persons affected by anemia live in developing countries. The estimated prevalence of anemia in developing countries is 39% in children <5 years, 48% in children 5–14 years, 42% in women 15–59 years, 30% in men 15–59 years, and 45% in adults >60 years. These staggering figures have important economic and health consequences for low and middle-income countries.3,4 Anemia is associated with less than optimal behaviour in infants and children. It is a nutrition problem worldwide. Young children and pregnant women are the most affected, with an estimated global prevalence of 43% and 51% respectively. Anemia prevalence among children of school age is 37.70%.5 Clinically, anemia can be detected on the basis of pallor of the palms, nailbeds, conjunctiva, mouth mucosa or tongue. Although various studies have been conducted on this topic, these are mostly of adult origin or in pre-schoolers. While the prevalence of anemia is high in the school age group, studies assessing most appropriate clinical markers in the age group of 6-14 years are few and far between. Hence this study has been undertaken to establish an easy to assess marker which can be used by medical and paramedical workers in the field and which has a good correlation and predictability of anemia, so that the disease can be detected and judiciously treated early.
AIM AND OBJECTIVES
MATERIAL AND METHODS An Observational cross- sectional study was conducted among school children aged 6–14 years in urban government schools from January 2017 to January 2018. Sample size was calculated with margin of error 5% and confidence level of 95% and prevalence of anemia as 65% 6 in children the sample size is 350. The children falling in the age group of 6-14years were enlisted for the study and those with skin disease dermatitis of hand and onycholysis, conjunctivitis, Glossitis, Use of nail polish, mehndi, Kajal and Refusal of consent were excluded from the study. 450 children were enrolled on planned visits to school out of which 394 students were included in study after obtaining written informed consent from parents and concerned authorities. Children were assessed for pallor at four sites by the investigator. In order to eliminate observer bias, 2 observers made independent assessment of anemia at the sites viz. conjunctiva, nail bed, palmar creases and oral mucosa. Clinical examination for pallor were made without having the information on the child’s hemoglobin level or of the other observer’s assessment for pallor. Anemia would be defined as hemoglobin level <11.5 g/dL as per WHO standards in the group of children in the study. Detailed history and clinical examination was carried out in all children. Pallor be graded as no anemia, mild, moderate and severe. In all children haemoglobin estimation done by Sahli’s hemoglobinometer. Anemia graded according to WHO criteria which is follows, Mild (11-11.4 gms%), Moderate (8-10.9 gms%) and Severe ( <8gms% ). Ethical clearance was obtained from the Hospital Ethics Committee and the hospital research committee. Informed consent was obtained by the principal of the school after informing the concerned parents, children and the necessary administrative authorities. All the data of the study was analysed using parametric and non-parametric tests for drawing valid conclusions in the study and its significance in the view of medical use by using SPSS EpiInfo 6, MS Excel
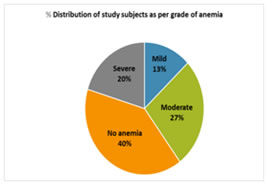
RESULTS The present study was conducted in urban government schools in apparently healthy school children aged 6-14 years during study period of one year from Jan 2017 to Jan 2018. During the study period, 450 children were examined. However 56 children were excluded from the study as they came under exclusion criteria. A total of 394 children were examined. The prevalence of anemia was 60% i.e. 237 children out of 394. The children in age group of 6-11 years, number of female and male children are 145 and 171 respectively. In age group 12-14 years, number of females were less than males 35 and 43 respectively. The prevalence of mild, moderate and severe anemia is 13%, 27 % and 20 % respectively in the present study as shown in figure
The accuracy of identifying grades of Anemia by both observers at various sites was shown in table-1. Using the readings at Palm site, 57.1% doctor observations are accurate with the lab bracket. 2/51 “Mild”, 35/106 “Moderate”, 153/157 “No Anemia”, 35/80 “Severe” readings were accurately diagnosed.
Table 1: Accuracy of observers
The data was analyzed to derive the sensitivity and specificity of all 4 sites. The tables 2-5 illustrates the specificity and sensitivity for the different sites viz. Conjunctive, Palm, Oral mucosa and nail bed.
Table 2: Sensitivity at different sites for grades of pallor as assessed by observer 1
The sensitivity of palmar pallor for observer 1 was highest 43% when severe anemia, Sensitivity to identify anemia including all sites ranges from 55.3 – 59.9%.
Table 3: Specificity at different sites for grades of pallor as assessed by observer 1
The specificity for severe pallor was 100% at all sites. Table 4: Sensitivity of different sites for grades of pallor as assessed by observer 2
The 2nd observer had the sensitivity of palmer pallor as the highest at 51.3%. Sensitivity to identify anemia including all sites ranges from 56.1 – 60.3%.
Table 5: Specificity of different sites for grades of pallor assessed by observer 2
The specificity for severe pallor was 100% at all sites. The Goodman and Kruskal Gamma is used as a measure the association between the different sites for an observer as shown in table – 6, 7. Table 6: Kruskal – Goodman Table for Observer 1
Table 7: Kruskal – Goodman Table for Observer 2
Fleiss Kappa was used as a measure to review inter observer reliability at the different sites i.e. the chances that both the observers had the same bracket for a particular site. It was derived for the different sites as shown in table – 8.
Table 8: Inter Observer Reliability
DISCUSSION The present study showed high prevalence of anemia among urban school children 6-14 years of age, who are in urban government schools and apparently belong from lower middle and low income poor socio-economic, where anemia rate is expected to be high.7,8 High rates of asymptomatic anemia have been reported in other studies as well.9 Identifying this can lead to better health and cognitive outcome for children with asymptomatic anemia. Hence the study was undertaken to identify the site/sites that helps to clinically diagnose anemia. The significance lies in the fact that usually these group of children often come in contact with primary health workers, how well they can pick up anemia simply by looking at a specific site so that moderate and severe anemia are identified and treated before it manifests clinically. During the period of study from January 2017 to January 2018, a total of 394 urban school children from government schools were enrolled for study. The prevalence of anemia in this study population was 60%. Among the total of 394 children 237(60%) were found to be anemic as per the WHO standards. Our study had prevalence similar to Chandrasekaran, et al10, where total prevalence of anemia was 62%. The finding in similar to study performed by Sudhagandhi et al11 in school children of Kattangulathur showed that the overall prevalence of anemia among children in the age between 8 to 16 years was 52.88% (476/900). The overall prevalence of anemia (Hb< 11 g/dl) was 66.0% in study by Desai et al,12Ritu S et al 13 found total of 143 (32.21%) children were anemic. DeMaeyeret al14 reported the worldwide prevalence of Anemia in 5-12 years old children to be 37%. In our study prevalence of mild, moderate and severe anemia were 13%, 27% and 20% respectively. According to Leal LP et al15 the prevalence of moderate/severe anemia were 16.2% and 20%, which was not far from our study. Chandrasekaran, et al study16 found Mild anemia in 39% (389 children), moderate anemia in was found in 21.2% (212 children) and severe anemia in 2% (20 children). According to Ritu S et al,13 the percentage of mild, moderate, and severe Anemia was found in 56.64%, 41.96%, and 1.40%, respectively, which had varied figures when compared with our study. Aseefa et al,19 out of 152 which, 73(18.1%) had mild while 79(19.6%) of them had moderate anemia. In our study among all children 54.31% (214) were male and 45.69% (180) were female and ratio being 1.2:1. In study by Arnab Ghosh et al male preponderance was seen similar to our study with a male to female ratio of 1.5:1.17. Muhe L et al 18 had also found male to be affected more in pediatric age group. In contrast to our study Sudha Gandhi et al11 showed that prevalence of anemia in girls (23.9 %, 141/590) was higher when compared to boys (7.7%, 41/530). According to the observations made by both the observers, they have correctly placed the pallor in respective category of no anemia, severe, moderate, and mild most accurately for palm followed by nail bed, conjunctiva and lastly oral mucosa. Both the observers have similar findings. The most correctly categorized was for anemia and no anemia, followed by severe pallor, then moderate and mild. Our study reveals that when detecting anemia vs no anemia highest sensitivity was seen for conjunctive (60.3%), Palm (59.9%), both oral and nail bed (56.1%). Both the observers showed that palm had the highest sensitivity for identifying severe pallor as the 43% and 51.3% respectively. Specificity for severe pallor was 100 % for all sites. In our study sensitivity was slightly better for moderate pallor ranged from 18.9% (oral) to 36.8% (palm) and sensitivity for severe pallor was 15% for oral and palm 51%. Luby et al.19 had very high i.e. 93% sensitivity for the detection of severe anemia and 66% for moderate anemia using palmer pallor. Arun Kumar et al20 health worker could diagnose palmar pallor with sensitivity ranging from 30.8 to 42.8% and specificity from 70% to 89%. Similarly for doctors sensitivity was 40–47% and specificity was 60–66%, respectively. The sensitivity to predict mild pallor for all sites ranged from 2% to 5.9 % which was very low. Leal et al15 also concluded that higher hemoglobin values are hard to detect and interpret through clinical signs. Kalantri et al study21 has reported a wide range of sensitivity and specificity estimates varying from 19% to 70% and 70% to 100% respectively. Study by Stoltzfus et al in 1999 found22 conjunctiva sensitivity to be 47.8% and specificity 97.5%, palm sensitivity 52.2% and specificity 95.5%, nail pallor sensitivity 50.0% and specificity 98.4%. Arun Kumar et al20 study stated that for most of the clinical signs, except for conjunctival pallor, the first examiner displayed a greater capacity to identify true positive results in cases of moderate/severe anemia, increasing the test sensitivity. The specificity ranges from 81.6% (conjunctiva) for moderate pallor to 100% for all sites when it came to severe. While it is difficult to predict mild pallor based on clinical signs as the severity increases the accuracy improves. Conjunctiva (60.3%) was found to be most sensitive in severe anemia cases though palm was very close to it (59.9%) and the remaining 2 sites were not very far behind. Specificity ranged from 81.6% to 100%. Moderate anemia can be predicted with sensitivity of 41.67% and has specificity of 86.04%, mild sensitivity is 10% and specificity 100%. The published literature about accuracy of clinical signs has reported a wide range of sensitivity and specificity estimates varying from 19% to 70% and 70% to 100% respectively Kalantri et al.21 Kalter et al in 1997,23 observed that the combined observation of palmar and conjunctival pallor was able to detect between 71% and 87% of all cases of moderate anemia, and 50% or more of all cases of mild anemia; roughly one-half of non-anemic children were incorrectly classified as being anemic. Desai et al, 12 concluded in their study combination of all four anatomical sites (conjunctiva, tongue, palm and nail bed) has not made pallor a more informative test. When comparing interobserver variation, our study shows high kappa scores >0.8 for all 4 site assessed similar to Shethet al24 (0.75 and 0.54), as the observers had standardized their physical assessments before they began the study. In contrast Kalantri et al21 study shows very low kappa scores for the conjunctival pallor was 0.07, and that for tongue, finger nailbed and tongue pallor was 0.19, 0.18, and 0.09 respectively. Nardone et al 25interobserver variability K scores were negative for palmar creases but ranged from 0.16 to 0.51 for other sites. Gjorup T, et al26 kappa values which ranged from 0.23-0.47.
CONCLUSION In this study prevalence of anemia was high in school children studied, but this cannot be extrapolated to general population as mostly government school children would be belonging to low socioeconomic group. The upside of this study is that it gives the prevalence in these group of children; thus targeted health programmes can help bridge the gap between the privileged and under privileged. According to our study conjunctiva and palm were the most sensitive to assess the severity of anemia. Clinical assessment of pallor can be used as initial screening tool for diagnosing anemia in school children especially in places where Prevalence in high and early incorporation of treatment is beneficial. This study was more useful for detecting moderate to severe anemia, though it is not sensitive to detect mild anemia. Therefore, it can be useful screening tool where there are no facilities for diagnosing anemia by laboratory testing. Limitations of the Study: It is worth noting that many factors could have led to variability in validity of the anemia classification with pallor at various sites. Skin colour and palmar pigmentation could vary in different parts of our country. Cleanliness of palms can be a hindering factor for observation. Among the various sites for assessing pallor, conjunctiva and palm will continue to be useful in early treatment of anemia with the caution that children with “no pallor” should also be followed up closely. REFERENCES
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home