A clinical study of rotaviral diarrhea in children aged 3 to 24 months
Madhurya B1, Shilpasri Y M2*
1Assistant Professor, Department of Paediatrics, Government Medical College, Mahabubnagar, Telangana, INDIA.
2Assistant Professor, Department of Paediatrics, Shridevi Institute of Medical Sciences and Research Hospital, Tumkur, Karnataka, INDIA.
Email: drmadhuclk@gmail.com drshilpa1011@gmail.com
Abstract Background: Diarrhea is a leading cause of childhood mortality in the world accounting for 5-10 million deaths/year. In early childhood the single most important cause of severe dehydrating diarrhea is rotavirus infection. Rotavirus and other viruses causing gastroenteritis not only are major cause of paediatric mortality but also lead to significant morbidity1. The Importance of rapid diagnosis of rotavirus infection has been stressed upon to initiate prompt rehydration therapy and prevent unnecessary use of antibiotics5. In the light of above, the present study is undertaken, to study the incidence, clinical features and the association of severe dehydrating diarrhea with rotavirus infection in Cheluvamba hospital, Mysore, a tertiary care hospital attached to Mysore Medical College. Objectives of the study: 1. To study the incidence of rotavirus gastroenteritis in children b/n 3 to 24 months of age admitted to the pediatrics unit with acute diarrhea. 2. To study the clinical features of rotavirus diarrhea. 3. To study the association of severe dehydrating diarrhea with rotavirus infection. Methods: After obtaining approval from the institutional ethics committee, a descriptive and explorative study was conducted in the Department of Paediatrics in Cheluvamba Hospital, Mysore. All Paediatric patients between 3 – 24 months of age admitted with a diagnosis of acute diarrheal disease are included. Details were entered in a predesigned proforma which has detailed history, no. of episodes of loose stools, vomiting, fever. Then a detailed anthropometry, head to toe examination and systemic examination is done. Dehydration is graded as no dehydration or some dehydration and severe dehydration according to WHO criteria. Stool samples were collected from the study population, only after informed and written consent was obtained. Stool samples once collected were transported to microbiology lab as soon as possible and were tested for rotaviral antigen by ELISA test. The information was collected and data was compiled and results obtained using SPSS version 20.0 and use of Microsoft excel. Results: The incidence of rotavirus infection in all acute watery diarrhoea among children between 3 and 24 months of age is 34 %. The incidence of rotavirus infection is greater among children between 3 and 12 months (82.4%), compared to children aged 13 and 24 months (17.6%). The children with rotaviraldiarrhea, 40 (58.8%) had fever, 45(66.2%) had vomiting, 60(88.2%) had some dehydration, 8 (11.8%) had severe dehydration, 19 (27.9%) had perianal excoriation. Out of 13 cases of severe dehydration 8(61.5%) were due to rotaviral diarrhea and 5 (38.4%) were due to non-rota viral diarrhea. Though the association between rotaviral diarrhea and severe dehydration is not statistically significant, there are positive trends for severe dehydration with rotaviral diarrhea than with non-rotaviral diarrhea. Conclusion: This study revealed that the association between rotaviral diarrhea and severe dehydration is not statistically significant, there is positive association between severe dehydration with rotaviral diarrhea than with non-rotaviral diarrhea.
Key Word: Incidence of Rota Virus; Rota Viral Diarrhea in Children; Rotaclone
INTRODUCTION
Diarrhea is a leading cause of childhood mortality in the world accounting for 5-10 million death/year. Twenty years ago, even the most sophisticated diagnostic facilities could identify a cause of acute diarrhoea in only 20% or less of all cases in childhood. Now that figure approaches 80%. By far the most important factor contributing to this remarkable improvement in diagnostic success is the recognition of human rotavirus as the major cause of acute diarrhoea in young children.2 In early childhood the single most important cause of severe dehydrating diarrhea is rotavirus infection. Rotavirus and other viruses causing gastroenteritis not only are major cause of paediatric mortality but also lead to significant morbidity.1 Worldwide rotavirus is estimated to cause > III million cases of diarrhea annually in children younger than 5 years, of these 18 million cases are considered atleast moderately severe with approximately 5 million deaths per year.1 1.00,000 deaths each year in India alone and more than 2,00,000 in Africa (80% of total deaths taking place in poorer countries). Considerable research work has been carried out on rotavirus disease in India. A review of 46 epidemiological studies concluded, that rotavirus positivity rates varied greatly between different settings, diarrhea hospitalisation (20%), neonatal infection (35%), symptomatic and asymptomatic infections in the community (15%) and 6.3% respectively) and nosocomial enteric infection (22.5%).3 The Importance of rapid diagnosis of rotavirus infection has been stressed upon to initiate and prevent unnecessary use of antibiotics.5 The sensitivity of rotavirus diagnostics is high since the amount of virus excreted by the child with diarrhea (1010 viruses/g of stool) far exceeds the level of detection (107 viruses/g of stool).7 In a comparison of ELISA technique and electron microscopy for investigating rotavirus infection ELISA was demonstrated to be more sensitive, especially for weakly positive cases. Because of its relative simplicity, low cost, and rapidity the ELISA appear to be more suitable for use in developing countries.4
OBJECTIVES
- To study the incidence of rotavirus gastroenteritis in children between 3 and 24 months of age in Cheluvamba hospital.
- To study the clinical features of rotavirus diarrhea.
- To study the association of severe dehydrating diarrhea with rotavirus infection.
METHODOLOGY
Source of Data: All paediatric patients (between 3 and 24 months of age) with diagnosis of acute diarrheal disease admitted to Cheluvamba Hospital attached to MMC and RI, Mysore from December 2013 to August 2014.
Method of Collection of Data: Sample Size: A sample size of 200 children with acute diarrheal disease admitted to Cheluvamba Hospital.
Sampling Method: Simple random sampling.
Type of the Study: Descriptive and explorative study.
Inclusion Criteria
All Paediatric patients between 3 and 24 months of age admitted in Cheluvamba Hospital with a diagnosis of acute diarrheal disease.
Exclusion Criteria
- Infants < 3 months and children > 2 years of age.
- History of gross blood in stools
- Persistent diarrhea (H/O loose stools for >14 days)
- Persistent severe or bilious vomiting
Method of Study: The proposed study is a observational study. A total of 200 children of paediatric age group 3 – 24 months are included in the present study. Details shall be entered in a predesigned proforma which has detailed H/O no. of episodes of loose stools, vomiting, fever. Then a detailed anthropometry, head to toe examination and systemic examination is done. Dehydration is graded as minimal or no dehydration or some dehydration and severe dehydration according to WHO criteria.
Statistical Methods Used
Descriptive Statistics Chi-square test Contingency table analysis Student ‘t’ test, independent samples using SPSS software (Version 20.0)
RESULTS
Table 1: Age wise distribution of rotaviral diarrhea
|
Age group (months) |
Total |
|
3-12 |
13-24 |
|
|
Positive |
Number |
56 |
12 |
68 |
Percentage |
82.4 |
17.6 |
100 |
Negative |
Number |
83 |
49 |
132 |
Percentage |
62.9 |
37.1 |
100 |
Total |
Number |
139 |
61 |
200 |
Percentage |
69.5 |
30.5 |
100 |
p=0.005
In this study 68 children were positive for rotaviral antigen of which 56 children (82.4%) belonged to age 3-12 months and 12 children (17.6%) belonged to 13-24 months of age.
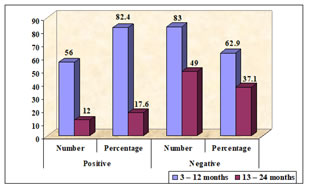
Figure 1: Age wise distribution of rotaviral diarrhea
Table 2: Degree of dehydration in rotaviral diarrhea cases
|
Dehydration |
Total |
|
Some |
Severe |
No |
|
Positive |
Number |
60 |
8 |
0 |
68 |
Percentage |
88.2 |
11.8 |
0 |
100 |
Negative |
Number |
126 |
5 |
1 |
132 |
Percentage |
95.5 |
3.8 |
8 |
100 |
Total |
Number |
186 |
13 |
1 |
200 |
Percentage |
93 |
6.5 |
5 |
100 |
p=0.076
Among 68 rotaviral diarrhea cases 60(88.2%) had some dehydration 8(11.8%) had severe dehydration. Out of 13 cases of severe dehydration 8(61.5%) were due to rotaviral diarrhea and 5 (38.4%) were due to non-rota viral diarrhea. Though the association between rotaviral diarrhea and severe dehydration is not statistically significant, there are positive trends for severe dehydration with rotaviral diarrhea than with non-rotaviral diarrhea.
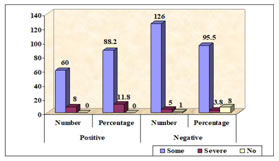
Figure 2: Degree of dehydration in rotaviral diarrhea cases
Clinical profiles
Table 3: Loose stool episodes per day in both groups
|
Stool |
Total |
<5 |
6 – 10 |
11+ |
|
Positive |
Number |
12 |
40 |
16 |
68 |
Percentage |
17.6 |
58.8 |
23.5 |
100 |
Negative |
Number |
14 |
100 |
18 |
132 |
Percentage |
10.6 |
75.8 |
13.6 |
100 |
Total |
Number |
26 |
140 |
34 |
200 |
Percentage |
13 |
70 |
17 |
100 |
p=0.047
Among the total diarrheal cases most children presented with an average of 6-10 episodes of loose stools per day.
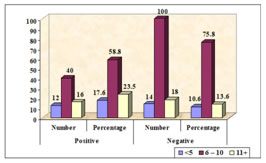
Figure 3: Loose stool episodes per day in both groups
Table 4: Perianal excoriation in both groups
|
Perianal excoriation |
Total |
|
Yes |
No |
|
Positive |
Number |
19 |
49 |
68 |
|
Percentage |
27.9 |
72.1 |
100 |
|
Negative |
Number |
7 |
125 |
132 |
|
Percentage |
5.3 |
94.7 |
100 |
|
Total |
Number |
26 |
174 |
200 |
|
Percentage |
13 |
87 |
100 |
|
p=0.000
Of the 26 children who had perianal excoriation 19(73%) belonged to rotaviral diarrhea group. (statistically significant p=.000)
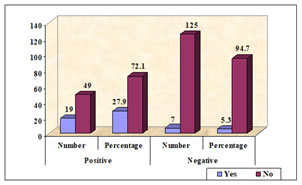
Figure 4: Perianal excoriation in both groups
DISCUSSION
Prevalence Rate: Previous studies in India as well as from different countries showed varying rates of incidence of rotaviral gastroenteritis, ranging as low as 4 to 62.6%. This wide spectrum of results can be explained by the samples of different age groups, different methods of detection, the seasonal variation of rotaviral infection and the geographical variations. Recent studies of rotaviral infections in India have concentrated mostly on the northern states. Hence this study was mainly focused on the southern state of the country. Incidence of rotaviral GE in children between 3 and 24 months of age in this study is 34%. This is in keeping with results from other similar studies conducted in India. Kang G et al. found an incidence rate of 39% in a multicenter, hospital based surveillance of rota virus disease and strains among Indian children. Borade A et al.9 showed an incidence of 37.77% in a study involving the characteristics of rotaviral GE in hospitalized children in Pune. Shariff M et al.8 showed an incidence rate of 38.7% in a study of diarrhea among children in eastern Nepal with special reference to rotavirus. Bahl R et al.11 showed an incidence of 23.5% of rotavirus infection in children suffering from GE in New Delhi. A high incidence of 71% rotavorus infection was reported in Calicut. Prevalence rates of the rotavirus infection differ from country to country. Raboni SM et al.10 found out rotavirus infection in 22.5% of children in Brazil. Van Damme P et al.6 showed a prevalence rate of 40.6% among seven European countries.
Age Distribution: In this study, majority of cases occurred in children < 12 months of age, which is the most susceptible target age group. Also most of the infection occurred in age group of 6 – 15 months which accounts for 95% of total positive cases. Around 82.4% of the total positive cases occurred among the children < 1 year of age, which is statistically significant (p value-0.000) Borade A et al.9 reported that occurrence of infections were most common in the age group 11-20 months (38.63%), followed by 0-10 Months (23.86%) Shariff M et al.8 also reported that the majority of infections (70.9%) were seen in children 6–24 Months of age Bahl R et al.11 found out that most of the children (98%) who were admitted for rotaviral GE were less than 2 years of age.
Gender: In this study male and female children constituted 54.4% and 45.6% respectively, of total children who were positive for rotavirus. There is no gender preponderance for infection in this study. Whereas few studies reported that there were association between gender and the incidence rate. This study found no significant evidence of that (p-0.624). Various studies done by Banerjee L et al.,12 Raboni SM et al.,10 and Ghazi HO et al.13 report that larger proportion of children with rotavirus infection were male.
Clinical Profile: In this study the associated clinical features in rotavirus positive children were fever in 58.8%, Vomiting in 66.2% and some Dehydration in 88.2% and severe dehydration in 11.8%. This is consistent with previous studies conducted by Barode A et al.9 in Pune. In this study Fever was present in 40 children (58.8%) out of 68 children with rotavirus infection. Vomiting present in 45 (66.2%) rotavirus positive children compared to the negative group showing a statistically significant association (p–0.37) in this study. Among 68 rotaviral diarrhea cases 60(88.2%) had some dehydration 8(11.8%) had severe dehydration. Out of 13 cases of severe dehydration 8(61.5%) were due to rotaviral diarrhea and 5 (38.4%) were due to non-rotaviral diarrhea. Though the association between rotaviral diarrhea and severe dehydration is not statistically significant, there are positive trends for severe dehydration with rotaviral diarrhea than with non-rotaviral diarrhea. Perianal excoriation were present in 27.9% of rotavirus positive children compared with other group (5.3%) showing a strong association (p-<0.001)
CONCLUSION
The incidence of rotavirus infection in all acute watery diarrhoea among children between 3 and 24 months of age is 34%. Incidence of rotavirus infection is greater among children between 3 and 12 months (82.4%), compared to children aged 13 – 24 months (17.6%). In children with rotaviral diarrhoea, some dehydration 60 (88.2%) was the most common clinical feature followed by vomiting 45 (66.2%), fever 40 (58.8%), perianal excoriation 19 (27.9%), and severe dehydration 8 (11.8%). Out of 13 cases of severe dehydration 8(61.5%) were due to rotaviral diarrhea and 5 (38.4%) were due to non-rota viral diarrhea. Though the association between rotaviral diarrhea and severe dehydration is not statistically significant, there are positive trends for severe dehydration with rotaviral diarrhea than with non-rotaviral diarrhea.
REFERENCES
-
Dorsey M Bass. Rotaviruses, Calciviruses and Astroviruses. In: Nelson Text Book of Pediatrics, Kliegman, Stanton, St. Geme, Schor, Behrman, eds.
-
Hamilton J Richard. Viral enteritis in Paediatric Gastroenterology I. Pediatr Clin North Am 1988 Feb;35(1):89-99.
-
Sasirekha Ramani, Gagandeep Kang. Review Article, Department of Gastrointestinal Science, Christian Medical College, Vellore, India. Indian J Med Res 2007 May;125: 619-32.
-
Dowe G, King SD, Maitland PB, Swaby-Ellis DE. Department of Microbiology, University of the West Indies, Mona, Kingston, Jamaica. Laboratory investigations on Rotavirus in infantile Gastroenteritis in Jamaica.
-
Vidya Nerurkar, Vipulmati Dhole. Paediatric Rotavirus Gastroenteritis: A2–years analysis to understand current prevalence in Mumbai. JHAS 2011 Jan-Mar;10(1).
-
Damme PV, Giaquinto C, Todd P, Wielen MV. On behalf of the REVEAL study group. Distribution of rotavirus genotypes in Europe 2004-2005. The REVEAL study. J Inf Dis 2007;195: S17-25.
-
Matthijnssens J, Ciarlet M, Heiman E, Arijs I, Delbeke T, McDonald SM, et al. Full genome based classification of rotaviruses reveals a common origin between human Wa-like and Porcine rotavirus strains and human DS-1 like and bovine rotavirus strains. J Virology 2008 Apr;3204-19.
-
Shariff M, Deb M, Singh R. A study of diarrhea among children in eastern Nepal with reference to rotavirus. Indian Journal of Medical Microbiology, subtype J Clin Microbiology 1999;37:1213-6.
-
Borade A, Bais AS, Bapat V, Dhongade R. Characteristics of rotavirus gastroenteritis in hospitalized children in pune. Indian J Med Sci 2010 May; 6(5):210-8.
-
Raboni SM, Nogueira MB, Hakim VM, Torrecilha VTG, Lerner H, Tsuchiya LRV. Comparison of Latex Agglutination with Enzyme Immunoassay for Detection of Rotavirus in Fecal Specimens. Am J Clin Pathol 2002; 117: 392-4.
-
Bahl R, Ray PV, Suboth S, Shambharkar B, Saxena M, Parashar U, et al. Incidence of severe rotavirus diarrhea in New Delhi, India and GandP types of infecting rotavirus strains. JID 2005;192(1):SI14-9.
-
Banerjee I, Ramani S, Prime Rose B, Mosis P, Iturriza GM, Gray J, et al. Comparative study of epidemiology of rotavirus in children from community based cohort and a hospital in South India. J Clin Micro 2006 Jul;44(7):2468-74.
-
Ghazi HO, Khan MA, Telmesani AM, Idress B, Mahomed MF. Rotavirus Infection in Infants, and Young Children in Makkah, Saudi Arabia. J Pakis Medical Asso 2005; 55: 231.