|
Table of Content - Volume 14 Issue 2 - May 2020
A study of sociodemographic factors associated with the patients of post-partum depression at tertiary health care centre
Amita Ranade1*, Abhishek Ranade2, Rajesh Ranade3
1Associate Professor, Department of Physiology, SBHGMC, Dhule, Maharashtra, INDIA. 2IInd MBBS Student, SKNMC, Pune, Maharashtra, INDIA. 3Department of Obstetrics and Gynaecology, Ranade Maternity Hospital, Dhule, Maharashtra, INDIA. Email: aabhiaadi@gmail.com
Abstract Background: Prevalence of depression among postpartum women is quite high and the health seeking for depression is very low. Postpartum depression has a major impact on health of mother and child. PPD can be prevented by reducing the associated risk factors. Aim and objective: To study the sociodemographic factors associated with the patients of postpartum depression at tertiary health care centre Methodology: Total 200 patients studied in a prospective study. Data collected with pretested questionnaire. Data included mainly ssociodemographic data like age, religion, education, employment, and economic status. Data regarding marital relationship, marital violence and social support was noted. Data analysed with appropriate statistical tests in depression patients and controls. Results and discussion: Incidence of postpartum depression in our study was 12.5%. In our study illiteracy, lower socioeconomic status, Sex preference for child, Marital disharmony and domestic violence were significantly associated factors in postpartum depression.
INTRODUCTION Pregnancy is regarded as a positive and necessary event for woman’s personal fulfillment and social acceptance. Postpartum period is period upto 6 weeks after delivery. Postpartum period is having various physical and mental complications. Postpartum depression is one important complication in postnatal period. Postpartum depression (PPD) is a prolonged and serious condition generally occurs in at least 13% of women within 4-6 weeks after delivery with low mood, anhedonia, forgetfulness, irritability, anxiety, sleep disturbance and postpartum psychosis though rare, is seen in 1-2/1000 deliveries.1 Women in the postpartum period are more vulnerable to develop depression. The global prevalence of postpartum depression has been estimated as 100‒150 per 1000 births.2 The current literature suggests that the burden of perinatal mental health disorders, including postpartum depression, is high in low- and lower-middle-income countries. A systematic review of 47 studies in 18 countries reported a prevalence of 18.6% (95% confidence interval, CI: 18.0‒19.2).3 Factors contributing to maternal depression are marital status of the mother, unplanned/unwanted pregnancy, unwanted gender of the baby, poor relationship with a partner, lack of emotional support in family, insufficient social support, poverty and social adversity. Maternal depression affects mother’s health. Postpartum depression can predispose to chronic or recurrent depression. In addition to mother it also affects children’s physical and psychological health. Maternal depression leads to lower birth weight of infants. Lack of care of baby leads to higher rates of underweight at 6 month of age. Children have poor long term cognitive development and increased rates of antisocial behaviour. 4,5 Thus postpartum depression has an important impact on mothers life. Early detection of risk factors will be helpful for prevention of depression so this study was conducted to find out the sociodemographic factors associated with postnatal depression. Aim and objective: To study the sociodemographic factors associated with the patients of postpartum depression at tertiary health care centre
MATERIAL AND METHODS Present study is a prospective study carried out in Psychiatry department of a tertiary health care centre. Total 200 pregnant females were recruited for the study. Females in third trimester were enrolled during their antenatal visits in department of Obstetrics. Inclusion criteria: 1. pregnant females in third trimester in age group of 10-35 years, Exclusion criteria: 1. Patients below 18 and above 35 years 2. Critically ill patients 3. Patients with past history of depression or psychiatric disease Study was approved by ethical committee of the institute. A valid written consent was taken from patient after explaining study to them. Pregnant females were interviewed at the time of enrolment, 4-6 weeks after delivery and 6 months after delivery. Data was collected with pre tested questionnaire. Data included sociodemographic data like age, religion, education, employment, and economic status. Data regarding marital relationship, marital violence and social support was noted. A detailed obstetric history was taken. Through clinical examination was done. All females were administered Edinburgh Postpartum depression Scale 6 at 6-8 weeks after delivery for assessment of postnatal depression. This scale has score in range from 0 to 30. Version of the scale was prepared in Marathi language for understanding of the patients. A cut off score of 11 or 12 on the Edinburgh Postpartum depression Scale was found to detect depression with a specificity of 85% and sensitivity of 92%. The patients who developed postpartum depression were treated accordingly. Data was analysed with appropriate statistical tests.
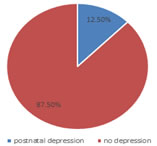
RESULTS Study was conducted to find the incidence and sociodemographic factors related to postpartum depression at a tertiary healthcare center. Out of total 200 patients 192 patients were followed up regularly until delivery and 8 weeks after delivery. 8 patients were lost in follow up due to change in delivery hospital. Out of 192 patients 3 patients had twins and 2 were still birth. All deliveries were institutional delivery except 2 who delivered during transit. They were admitted in the hospital and followed up. Out of 192 patients 24 patients have Edinburgh Postpartum depression Scale score of 11-12,so incidence of postpartum depression in our study was 12.5%. Table 1 shows comparison between patients diagnosed with postpartum depression and those with no depression according to sociodemographic variables. Majority of the patients were from age group of 21-29 (around 70%) in both the groups. Patients above 30 years were 8.33% and 9.52% in both the groups respectively. This may due to our inclusion criteria of 18-35 years. Majority of the patients in the patients with depression were illetrate (41.66%) followed by primary education . Patients with secondary education and higher education were 16.67% in both categories. In case of patients without depression majority patients were having secondary education (37.5%) followed by primary education (26.9%). Illiteracy contributes to depression. Education of patients in depression group was significantly lower than control group. (p<0.05). In our study majority of the patients were working women in patients with depression (58.33%) and in control group (54.76%). In our study we studied socioeconomic status of the patient with B G Prasad economic scale and categorized these patients into three classes for study purpose lower, middle and upper socioeconomic status. Majority of the patients in cases (patients with depression) were from middle class (41.67%) followed by lower class (37.5%). In control group majority patients were from middle class (37.5%) and upper class (33.34%). When we applied chi square test economic class of the patient shows significant difference in both the groups. (table 1) In our study we studied some social factors to see their association with postnatal depression. Majority of the patients were from nuclear family in both cases (54.17%) and controls (53.57%). Majority of the patients in both the groups were from rural area (62.5% and60.12%). Type of family and place of residence were not associated with postpartum depression (P>0.05). Majority of the patients with depression have sex preference (62.5%) Specially male child. But such preference is not seen in control group. This difference is statistically significant. Marital disharmony was most commonly observed in postpartum depression patients (66.67%) than control group(51.19%). The difference between them is statistically significant (p<0.05) In patients with postpartum depression domestic violence (62.5%) was more than control group (52.38%). The difference between them is statistically significant (p<0.05).
Figure 1: distribution of patients according to EPDS score Table 1: Comparison of postpartum depression cases and controls according to sociodemographic variables
Table 2: Comparison of postpartum depression cases and controls according to social variables
DISCUSSION Incidence of postpartum depression in our study was 12.5%. various studies show different range of postnatal depression. It is due to different study population, difference in methodology, different sociocultural environment of patients . In a study in Gadchiroli, severe anxiety, or depression during the postpartum period was present in 7.4% of the women.7 The prevalence of depression in postnatal period is 23% in a study by Patel V . 8 In a study by Prost A in rural Jharkhand and Orissa 11.5% of mothers had symptoms of distress.9 Chandran M et al. in Vellore found that 19.8% women suffer from postnatal depression. 10 In studies in Aberdeen and Australia prevalence of postpartum depression was 21% and 16.9% respectively.11,12 In our study education of patients in depression group was significantly lower than control group. (p<0.05). similar findings were seen in Yehia et al. where they found Predominance of less educated (less than 12th standard) among the depressed mothers was significant.13 women who were illiterate were financially dependent, had less social support and highly educated women were financially independent and better interpersonal relationship could be the reason for difference in depression prevalence. In our study lower socioeconomic status was significantly associated with postnatal depression. (p<0.05) similar findings were seen in previous studies where lack of money was a risk factor for depression and that lower socio-economic status is related with poor mental health.8,10 In our study Sex preference for child (62.5%), Marital disharmony (66.67%) and domestic violence (62.5%) were significantly more in postpartum depression than control group. (p<0.05) Indian mothers are at a constant pressure to bear a male child so they have preference for male child. Birth of female child in such patients leads to postnatal depression. Similar findings were seen in Patel V et al.8 and Chandran M et al.. 10 Marital disharmony is common in Indian population. It is seen due to various factors like gender bias in family, financial dependence of female, male dominated society. Domestic violence in females is commonly observed in India.14 marital disharmony and domestic violence precipitates depression.
CONCLUSION Higher education to females, making women financially independent, Parent counseling to promote marital communication and to reduce the preference for male children and reducing domestic violence must be implemented to prevent postnatal depression.
REFERENCES
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home