Official Journals By StatPerson Publication
|
Table of Content Volume 12 Issue 3 - December 2019
Study of prevalence and pattern of psychiatric morbidity in liaison context in a tertiary hospital
Vishnu Vardhan Gandikota1, Kishore Kumar Rokkam2*
1Assistant Professor, Department of Psychiatry, Sri Venkateswara Medical College, Tirupathi, Andhra Pradesh, INDIA. 2Assistant Professor, Department of Psychiatry, Santhiram Medical College, Nandyal, Andhra Pradesh, INDIA.
Abstract Background: Stigma is still prevalent in India, even in health care professionals regarding mental illness. This is responsible for delay in referral and failing to identify psychiatric symptoms in that right time. Hence studies regarding cross referrals and liaison psychiatry is the need of the hour in providing comprehensive care to the patients. It is welcoming that psychiatric services had moved from mental hospital to a general hospital psychiatric unit which made the availability of psychiatric services closer to the public and made an effort to reduce the stigma Materials and Methods: Referrals to Psychiatric Department were assessed for six months period with 505 patients. Out of these, 384 were inpatients referred from the general hospital and other hospitals, 59 were outpatients referred from various specialities, and 62 were from the emergency unit. Results: Suicidal ideation/ attempts (51.92%) was the most common reason for psychiatric consultation. Inpatients referrals and outpatient referral rates were 2.3% and 0.075. Depression is very frequent, which has to be recognised early and intervened. Conclusion: Most of the referrals are from medicine and related departments. Suicidal attempts are the most common reason for referral. Mood disorders are a common psychiatric illness observed.
INTRODUCTION General hospitals have an essential role in the evolution of psychiatry. They have provided soil for the growth of inpatient psychiatric units, consultation-liaison psychiatry, psychosomatic medicine, med-psych units, outpatient psychiatric clinics, emergency services and a whole spectrum of resources for the communities in which they exist. General hospital psychiatry units have provided increased opportunities for interaction between psychiatrists and other medical specialists, making consultation-Liaison Psychiatry more meaningful 1.It is welcoming issue that psychiatric services had moved from mental hospital to a general hospital psychiatric unit which made the availability of psychiatric services closer to the public and made an effort to reduce the stigma
MATERIALS AND METHODS The present study had been conducted in the Department of Psychiatry, Sri Venkateswara Medical College, Tirupati. The hospital is a Tertiary General Hospital with about 1200 beds covering all disciplines like Casualty, General Medicine, General Surgery, Paediatrics, Dermatology, Ophthalmology, ENT, Paediatric Surgery, NeuroSurgery, Gastroenterology. All departments run OPD. Hospital related to obstetrics and gynaecology is separate one (Government Maternity Hospital, GMH). Inpatient and outpatient referrals, including emergencies to the Department of Psychiatry, were taken to study over for six months. All the referrals registered at Psychiatric OPD. Referrals coming from an outside source apart from the general hospital also included. Patients were informed about the purpose of the study, and voluntary written consent, taken before their inclusion. Confidentiality of the patient was maintained. Those who do not give consent and prisoners, excluded from this study. A proforma containing all the parameters of the study like demography, source of referral, reasons for the referral, psychiatric diagnosis given by the referring unit, diagnosis made at the psychiatric unit documented. All the particulars of the referred cases noted in consultation with the referring doctor. Inpatient and outpatient, including emergencies, were noted separately. The psychiatric diagnosis confirmed according to International Classification of Diseases (ICD-10), and necessary intervention was done. The details about the clinicians who referred, collected at the respective OP and wards. The collected data analysed after the end of the study.
OBSERVATIONS AND RESULTS Total referrals to Psychiatric Department were 505 during six months period with 2.7 cases per day. Out of these, 384 were inpatients referred from the general hospital and other hospitals, 59 were outpatients referred from various specialities, and 62 were from the emergency unit.
Table 1: Distribution of Source of referral
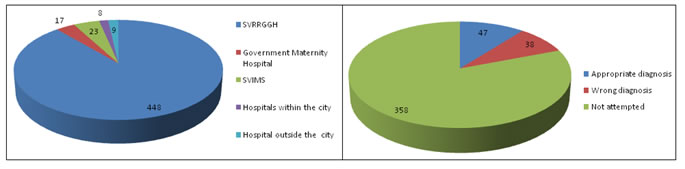
SVRRGG Hospital contributed major referral cases forming 88.7% of total referrals with 354 inpatients, 32 Outpatients and 62 cases from emergency. Sri Venkatewswara Institute of Medical Sciences (SVIMS) which is a super speciality hospital located adjacent to SVRRGGH having Neurology, Nephrology, Neurosurgery, Gastroenterology, Cardiology and other surgical and medical branches referred 4.6% of cases.1.6% of cases are from hospitals with in city and 1.8% from outside city. Government maternity Hospital consisting Obstetrics and Gynaecology departments referred 3.4%.
Table 2: Hospital Inpatient and outpatient details and Referral rates
Table 2 Showing the number of total referrals in comparison to total hospital admissions and also in comparison to attendance at Psychiatric OPD. The inpatient referral rate was 2.3%, and outpatient referral rate was 0.075%. Inpatient referrals were three times more than outpatient referrals Table 3: Distribution of Departments
Among specialities, most of the referrals were from General medicine among inpatients and outpatients(68.7% and 18.6% respectively) and total patients (62.1%) followed by Surgery(7.9%) and referral rate ENT and ophthalmology it was 1.8%. Apart from psychiatry, Dermatology and Neurosurgery had least referral rates (1.1% each). Among super specialities, 5% of cases were from cardiology, which formed third-highest referral among all departments. General practitioners referred only 1.8% of cases. Less than 2% rates, received from Neurology, Neurosurgery, Dermatology and ENT and ophthalmology. Around 80% of cases are from medical branches, and about 20% are from surgical branches
Table 4: Reason for the referral
Table 4 showing the reasons for the referral revealed suicidal ideation/ attempts (51.92%) was the most common reason for psychiatric consultation.
Table 5: Psychiatric diagnosis made by referring clinician
Table 6: Diagnoses made by psychiatrist according to ICD-10
The most common diagnosis made by attending psychiatrist in the emergency unit was mood disorder (30.6%) followed by substance use disorders (16%). The diagnosis made by psychiatrist depicted in Fig 8. Among mood disorders, manic excitement was the most frequent (63%, 12 cases out of 19). Other mood disorders seen are moderate depression with conversion disorders (3 cases), severe depression with psychotic features (3 cases) and 1 case of recurrent depressive disorder with psychotic features (Fig 4). However, when the attending clinician’s diagnosis analysed, it showed psychosis was the most common diagnosis made. Females have psychiatric illness more of mood disorders followed by neurotic, stress-related and somatoform disorders and males are having a significant number of substance-related disorders followed by mood disorders.
Table 7: Mode of suicidal attempt
Mode of attempt studied showed, poisoning was the common method used (81.4%). Among poisoning, insecticide poisoning was the most common method followed by taking excess doses of medications prescribed to them/their family members or bought from different medical stores several times and collected. In this study, out of 34 cases of medication poisoning, 19 cases (55.8%) had taken benzodiazepines, 8 cases taken cetirizine tablets and remaining had taken analgesics and other medication. Super Vasmol poisoning in this study, taken three times were commonly by females than males. Self-inflicted injuries were attempted more in males than females. Other methods of attempts were 28 cases in the form of burns, unknown poisoning, falling from moving vehicles and height. No drowning and gunshot reported.
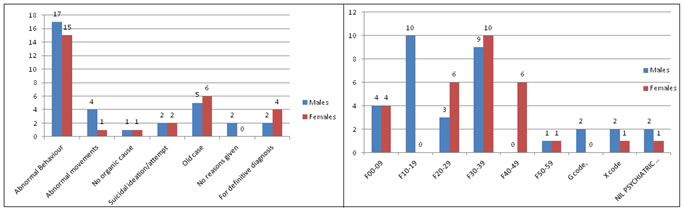
Figure 1: Number of cases from different hospitals Figure 2: Diagnosis attempts Figure 3: Reason for the referral in Emergency Figure 4: Diagnosis made by Psychiatrist in Emergency The most common reason for the referral from emergencies was abnormal behaviour (51.6%), followed by the old case of psychiatry (17.7%). Suicidal ideation or attempts were 6%. Abnormal behaviour in the form of aggression was seen almost in equal number in males and females. Abnormal movements referred were 5 in number (4 males, one female).Suicidal attempt as referral seen in 2 males and two females. No organic cause found were 2 in number. Six cases referred for definitive diagnosis. The details are given in Fig.3.
DISCUSSION Distribution of Source of referral SVRRGG Hospital contributed primary referrals, 88.7% of total referrals. Sri Venkateswara Institute of Medical Sciences(SVIMS) referred 4.6% of cases. Government Maternity Hospital (GMH) consisting of Obstetrics and Gynaecology departments, referred 3.4% of cases, more than that of Lin HL et al.2 study in which psychiatric referrals formed 0.11% of all cases. In contrast, Ajit Avasthi et al.3 study had 7.5% referrals from obstetrics and gynaecology. Referral rates The inpatient referral rate was 2.3%, and outpatient referral rate was 0.075%. Referral rates vary from country to country and vary within the country between studies. In India, the referral rates of inpatients varied from 0.15% to 3.6%.4 In this study, the inpatient referrals rate was 2.3% which is 16 times more than Jindal RC and Hemrajani DK study(0.15%)5, six times that of Aghanwa H (0.4%)6 and 1.8 times more than the study of Grover S.7 This unveils varying attitude of clinicians to look for psychiatric disorders in inpatients admitted under their care. Indian studies outpatient referral rate varied from 0.06% to 1.94%. In this study, it was 0.075% which is a poorer rate than Jindal RC and Hemrajani DK study5. Referrals were high in USA studies, where the rate varied from 0.5% to 9.13%. Distribution of Departments Among specialities, most of the referrals were from General medicine among inpatients and outpatients and total patients followed by Surgery(table 6). This finding is in agreement with previous studies like Bhogale GS et al.8 (General medicine 83.17%.,2000), HP Jhinghan (63%)9, Singh PM et al.10 (General medicine- 49.8% and Surgery-11.2%., 2009) and Chinese study (Chen CY).[11] The present finding was because psychiatry is a branch of medicine and physicians are most oriented to psychiatry than other specialities. Surgery referral rate was 7.9% and from ENT and ophthalmology was 1.8% which are lower than the study of Singh PM 10 where the referral rates were 11.2% and 10.3% respectively. Nephrology had a lower rate than seen in the study of Chen CY.58 Obstetrics and gynaecology had referrals rate almost the same as in Lin HL study2, but much lower than Ajith Avasthi study.3 Reason for the referral Suicidal ideation/ attempts (51.92%) was the most common reason for psychiatric consultation a finding similar in studies of Singh PM et al.10 and MMC Wong et al. (2014).12 The reason could be that suicidal attempts, and medico-legal cases are mostly dealt with by government tertiary hospitals leading to increased number in hospital admission. It is in contrast to the finding of other studies like Bhogale GS et al.[13] Where unexplained somatic complaints were the most common reason. Surprisingly, in this study, vague complaints formed only 3.4%, which was the reason least referred. Males referred to in every component (fig.4). The reason could be that males are more in number in this study. EMERGENCIES Out of 505 cases, 62 were from emergency (12.2%). In emergency cases, males and females ratio was 1.1:1. The ratio was 1.3:1 in the study of Saddichha S 14 Mostly, males were reported in the study of James et al.15 and females were predominant in the study of Padilha et al.16 The referral rate was 0.2% which is less than other Indian and western studies. Emergency referral rate was low compared with figures of 1.8% in the UK and 3.9% in the USA studies. (Mahgoub OM., 2000).17
CONCLUSIONS
REFERENCES
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home