Official Journals By StatPerson Publication
|
Table of Content Volume 12 Issue 3 - December 2019
Ocular complications associated with different substance abuse and dependence pattern - A clinical study
Anirban Chakrabarti1, Nivedita Choudhury2*
{1Associate Professor, Department of Psychiatry} {2Associate Professor Department of Ophthalmology} Mata Gujri Memorial Medical College and Lions Sevakendra Hospital, Kishanganj, Bihar, INDIA Email: chakrabarti.a@gmail.com
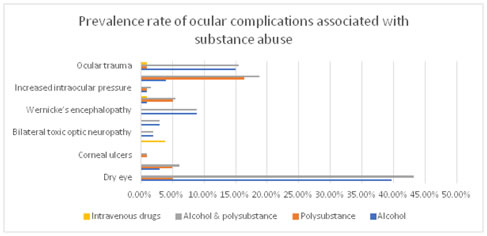
Abstract Substance abuse means the use of psychoactive substances, like illicit drugs and alcohol that produce harmful effects on health and can lead to dependence syndrome on repeated use. Background: Different types of ocular and neuro-ophthalmic complications ranging from dry eye to endophthalmitis and toxic amblyopia are associated with different substance abuse. The present study is an attempt to find out the prevalence of different ocular complications associated with different substance abuse and dependence pattern in a tertiary hospital in north Bihar. Materials and Methods: It was a non-interventional cross-sectional study done on patients of substance abuse who sought consultation in the psychiatry OPD and Ophthalmology OPD for ocular complications of substance abuse in a tertiary hospital in north Bihar for a period of one year. The aim of the study was to find out the one-year prevalence of different ocular complications of substance abuse among the selected patients. The data collected was recorded and analyzed. Results and Observations: The commonest ocular complication in alcohol abusers was dry eye (39.6%), followed by ocular trauma (15%), Wernicke’s encephalopathy (8.82%), ARMD (3.96%) and tobacco alcohol amblyopia (2.97%). Age related macular degeneration (ARMD) was the commonest complication in polysubstance abuse (16.33%), followed by dry eye and cataract (5.1%) each, and cataract (5%). When an alcohol abuser simultaneously abused some other substance, the prevalence rate of all the ocular complications increased. Among all types of substance abusers, intravenous drug abusers are least likely to have ocular complications. However, endophthalmitis was the commonest complication in this group (3.84%), followed by cataract and ocular trauma (1% each). Conclusion: Substance abuse and dependence cause a variety of ocular complications. Early diagnosis and management of ocular complications can reduce visual morbidity in substance abusers. Key Words: substance abuse and dependence, ocular complications.
INTRODUCTION Alcohol, cannabis and opium are the traditional drugs abused in social and ritual gatherings in India. (Ganguly et.al. 1995)1 Channabasavanna 1998, Siddiqui and Britto 19972,7 in their studies showed that cannabis, opium, methaqualone, barbiturates and minor tranquilizers were most often abused substances. Heroin became a commonly abused drug amongst youths and psychiatric patients since it was first reported in 1985 (Mohan et.al 1985)3 .It became a common substance of abuse since then and was widely used by the young people and psychiatric patients (Sharma et al 1995).4 A study conducted in 9 urban centers across India on drug abusers found that 43% were abusing alcohol, 51% different opioids and 6% cannabis (Mittal and Ch’ien 1998)5. Recent studies have revealed that 19% of all drug abusers were intravenous drug abusers and significant proportion of them were HIV positive. Different ocular complications and neuro-ophthalmic complications are associated with different substance abuse, ranging from dry eye to endophthalmitis and loss of vision. Very few studies estimating prevalence rate of different ocular complications in substance abusers were ever done in the state of Bihar. The present study is an attempt to find out the prevalence of different ocular complications associated with different substance abuse and dependence pattern in a tertiary hospital in north Bihar.
AIMS AND OBJECTIVES To find out the prevalence of different ocular complications associated with different substance abuse and dependence among them.
MATERIALS AND METHODS
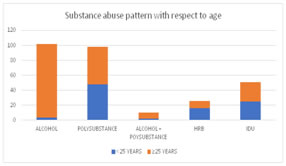
RESULTS AND OBSERVATIONS The sample size of the present study was 209 consisting of 187 males and 22 females. The total sample was analyzed separately with respect to age and sex. There were 53 patients below 25 years and 156 patients ≥ 25 years. The mean age of male patients was 32.41 years (16-70 years) with SD ± 10.35 years. On the other hand, the mean age of female patients was 33.91 years (15-55 years) with SD ±12.46 years. Substance abuse pattern with respect to age: The sample size was divided into two groups, one <25 years and the other ≥ 25 years. There were 53 patients (25%) < 25 years and 156 patients (75%) ≥ 25 years. 91% of the patients (n=48) <25 years were abusing poly-substance while only 6% (n=3) were abusing alcohol (P<0.05). 47% (n=25) of the < 25 years patient had a history of IDU and 30% (n=16) reported having high risk behavior. In contrast 63% (n=98) of the patients ≥ 25 years were abusing alcohol and 32% (n=50) had a history of poly-substance abuse. Only 17% of this group (n=26) had a history of IDU (P<0.001) and only 6% (n=10) reported high risk behavior.
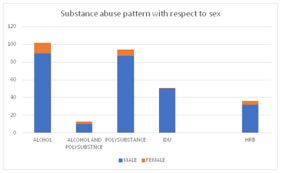
The Substance abuse pattern with respect to sex: Among the male patients 48% (n=90) were abusing alcohol and 47% (n=87) were abusing poly-substance. The number of patients abusing both polysubstance and alcohol was 10 (5%). 57% (n=50) of poly-substance abusers were doing so by intravenous route. Of all the males 27% (n=50) were intravenous drug users. 17% (n=32) of the male patients reported high risk behavior (sharing needles, unprotected sex, and multiple sex partners). On the other hand, 55% (n=12) of the female patients were abusing alcohol. The percentage of women abusing poly-substance and poly-substance and alcohol was 32% (n=7) and 14% (n=3) respectively. The number of female patients involved in high risk behavior was only 4 (18%).
Table 1: Prevalence rate of the ocular complications associated with substance abuse:
DISCUSSIONS The commonest ocular complication in alcohol abusers was dry eye (39.6%), followed by ocular trauma (15%), Wernicke’s encephalopathy (8.82%), ARMD (3.96%) and tobacco alcohol amblyopia (2.97%). Age related macular degeneration (ARMD) was the commonest complication in polysubstance abuse (16.33%), followed by dry eye and cataract (5.1%) each, and cataract (5%). When an alcohol abuser simultaneously abused some other substance, the prevalence rate of all the ocular complications increased. Among all types of substance abusers, intravenous drug abusers are least likely to have ocular complications. However, endophthalmitis was the commonest complication in this group (3.84%), followed by cataract and ocular trauma (1% each). Consumption of ethanol and smoking have been associated with dry eye symptoms in several studies.8 The dry eye symptoms were related to a history of heavy alcohol consumption, but not current alcohol consumption according to The Beaver Dam Eye Study.9 Cumurcu T et al (2013)10 showed that men who drink more than 4 drinks per day had decreased tear film breakup time, lower Schirmer 1 test and altered conjunctival impression cytology. The present study found mild dry eye in 22 patients, moderate dry eye in 15 patients and severe dry eye in 3 patients who abused alcohol, making a total of 40 patients with dry eye out of 101 patients of alcohol abuse. The prevalence rate was 39.2%. The prevalence rate of dry eye in patients with polysubstance abuse was found to be 5.1%. The prevalence rate of chronic conjunctivitis was found to be 3% in cases of alcohol abuse and 5% in cases of polysubstance abuse. Chronic conjunctivitis was reported in a series of cases of heroin and marijuana abuses by McLane NJ and Carroll DM (1986).11 The prevalence rate of corneal ulcers in abusers of polysubstance was 1% e. Poulsen EJ et al (1986)12 had reported cocaine abuse as a cause of devastating corneal ulcers in a case series. Severe endophthalmitis was reported in only one case of 26 intravenous drug users giving a prevalence rate of 3.84%. Kim RW et al (2002)13 described a variety of organisms causing endophthalmitis in intravenous drug abusers. Bilateral irreversible toxic optic neuropathy was found in 3 cases of total 101 alcohol abusers, giving a prevalence rate of 2.97%. Sanaei-Zadeh H et al (2011) 14 described a retrospective series of 37 cases of methanol poisoning in which 14% showed irreversible toxic optic neuropathy with complete blindness. In the present study, the cases of bilateral toxic optic neuropathy may indicate the possible adulteration of ethanol with methanol despite the continued efforts by the state Government to ban the sale and distribution of alcohol in the state of Bihar. Tobacco alcohol amblyopia was found in 3 cases of 101 alcohol abusers who were malnourished. The prevalence rate was estimated to be 0.02%. Phillips PH et al (2005)15 in their study found that the optic neuropathy was not due to the direct toxic effect of ethanol but due to malnutrition associated with it. Prevalence of Wernicke’s encephalopathy was found to be 8.82% in alcohol abusers. Torvik a et al16 found Wernicke’s lesion in 2.8% of general population autopsies, 12.5% of alcoholics and 35% if cerebellar damage due to lack of thiamine is included. The present study revealed prevalence rate of cataract to be 7.1%. The prevalence rate of cataract in the substance users of less than 25 years was only 0.01%. whereas the prevalence rate of cataract in substance abusers above 25 years of age was 7.09%. This finding may be confounded by the senile cataract in elderly patients. The Beaver Dam Eye Study17 found a dose response relationship of smoking cigarettes with formation of cataract. Galor A et al (2011)18 in their study documented the association of smoking cigarettes with cataract formation. Our study found increased intraocular pressure (>21mm of Hg on two consecutive occasions) in 0.99% of alcohol abusers and 1.02% in polysubstance abusers. Studies had found no consistent association of alcohol consumption and increased intraocular pressure and glaucoma.19 Our study revealed the prevalence rate of ARMD to be 3.96% in alcohol abusers and 16.33% in polysubstance abusers. Several population-based studies have revealed the association of smoking with age related macular degeneration (ARMD). An increased risk of both early and late age-related ARMD in individuals who consumed more than 20g of alcohol per day the Melbourne Collaborative Cohort Study20. However, the Beijing Eye Study found no association of moderate alcohol consumption with ARMD.21 Prevalence of ocular trauma in the present study was found to be 15% in alcoholics, 1% in polysubstance users and 1% in intravenous drug users, making an overall prevalence rate of 17% in the substance abusers. The rate of alcohol and other drug abuse in patients of open globe injury ranges from 24-73% according to Rahman I et al (2006). 22
CONCLUSION Substance abuse and dependence cause a variety of ocular complications leading to significant visual morbidity. We must be aware about the myriad of ocular complications of different substance abuse and should manage them early for avoiding visual morbidity.
REFERENCES
|
|
 Home
Home