Official Journals By StatPerson Publication
|
Table of Content Volume 12 Issue 3 - December 2019
Prevalence of psychiatric co-morbidities among the patients of primary headache in a tertiary hospital in north Bihar
Anirban Chakrabarti1, Nivedita Choudhury2*
{1Associate Professor, Department of Psychiatry} {2Associate Professor, Department of Ophthalmology} Mata Gujri Memorial Medical College and Lions Sevakendra Hospital, Kishanganj, Bihar. INDIA. Email: chakrabarti.a@gmail.com
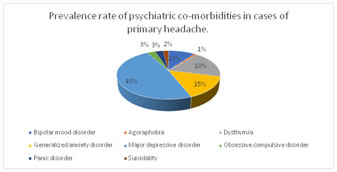
Abstract Background: Headache disorders constitute the commonest disorders of the nervous system and primary headache like migraine and tension type headache cause significant disability worldwide. The psychiatric co-morbidities associated with primary headaches also cause considerable disabilities globally. The present study is an attempt to find out the prevalence rate of different types psychiatric co-morbidities among the patients of primary headache in a tertiary hospital in north Bihar. Materials and Methods: The present study was a cross-sectional study done at a tertiary hospital in north Bihar done for a period of one year to find out the prevalence rate of different types of primary headache among the cases of primary headache aged between 13-60 years and the prevalence rate of different psychiatric co-morbidities among them. Results and Observations: The prevalence of tension type headache was 69%, migraine was 28% and cluster headache was 3%. Major depressive disorders were the commonest psychiatric co-morbidity associated with primary headache (48%), followed by dysthymia (18%), generalized anxiety disorder (15%) and bipolar mood disorder (10%). Discussions: The present study found tension type headache to be the commonest type of primary headache and female preponderance of cases of primary headache which conforms to the result of other studies.3,4 the prevalence rate of different psychiatric co-morbidities conforms to the results of other studies.7 Conclusion:Different psychiatric co-morbidities are associated with primary headache which often remain undiagnosed. Early diagnosis and effective management of such co-morbidities will help the patients of primary headache to have a better quality of life. Key Words: primary headache, tension type headache, migraine, psychiatric co-morbidities.
INTRODUCTION Cases of primary headache are the headache that are not caused due to any other medical conditions. These headaches include migraine, tension headache, cluster headache, other trigeminal autonomic cephalgia and other types of primary headache.1 Headache disorders are the commonest disorders of the nervous system and constitute a significant social and financial burden. According to Global Burden of Disease Study (2013), the headache disorders collectively were the third highest cause of years lost due to disability (YLD) and migraine alone was the sixth highest cause worldwide. A systematic analysis of the Global Burden of Disease Study (2016) showed that three billion people worldwide suffer from migraine and tension type headaches.2 Non-compliance and irregular treatment of patients with chronic headache predisposes that person to many psychiatric co-morbidities like anxiety and depression. The present study is an attempt to find out the prevalence rate of different types psychiatric co-morbidities among the patients of primary headache in a tertiary hospital in north Bihar. The purpose of the study is to create awareness among the medical professionals and patients about the seriousness of the psychiatric co-morbidities of primary headache and importance of early and effective treatment of the co-morbid conditions.
AIMS AND OBJECTIVES
MATERIALS AND METHODS
RESULTS AND OBSERVATIONS The total number of patients diagnosed to have primary headache is 100, out of which 15 patients were male and 85 patients were female. So, the prevalence of women was 85% and that of men was 15%. The prevalence of married persons was 87% and that of unmarried persons was 13%. The prevalence of illiterate patients was 71% and literate patients was 29%. The prevalence of tension headache was 69%, migraine was 28% and cluster headache was 3%. Table 1: Prevalence rate of different types of primary headache
Table 2: Prevalence rate of different psychiatric co-morbidities among patients of primary headache:
The prevalence rate of combined major depressive disorder and generalized anxiety disorder was 5%.
Table 3: Psychiatric co-morbidities in patients of migraine:
Table 4: Psychiatric co-morbidities in patients of tension type headache:
Major depressive disorder was found in all 3 cases of cluster headache. So, the prevalence rate of psychiatric co-morbidity (major depressive disorder) in patients of cluster headache was 100%.
Table 5: Types of headache in dysthymia:
Table 6: Types of headache in tension type headache:
Table 7: Types of headache in major depressive disorders:
Table 8: Types of headache in obsessive compulsive disorder
Table 9: Types of headache in panic disorder
Migraine was present in each of the 2 cases of suicidality giving the prevalence rate of primary headache in patients with suicidality to be 100%.
DISCUSSIONS Our study was conducted in a tertiary hospital of north Bihar, India. Little data is available for prevalence of primary headache and psychiatric co-morbidities in this population despite the prevalence of primary headache being studied in different subsets of population worldwide. The present study found the one-year prevalence rate of tension type headache (TTH) was 69%, that of migraine was 28% and that of cluster headache was 3%. The study also found that primary headache is commoner in women (85%) compared to men (15%). Stovner et al 3reported worldwide lifetime prevalence rates of 66 % (65 % in males, 69 % in females) for primary headache, 14 % for migraine, and 46 % for TTH, as well as worldwide 1-year prevalence rates of 47 % (37 % in males, 52 % in females) for primary headache in general, 12–15 % for migraine, and 38 % for TTH. A study conducted in northern China found that one-year prevalence rate of primary headache in population older than 60 years of age was 10.30 %, of tension-type headaches was 2.02 %, of migraines was 0.85 %, of chronic headache was 3.79 %, and of unclassified headache was 3.63 %.4 A study conducted in Malaysian population observed 1-year prevalence rates of 26.5 % for TTH, 9.0 % for migraine, and 28.2 % for other subtypes of headache.5 The study conducted by Stovner et al3 and the study conducted in northern China4 also found that the prevalence of primary headache was commoner in women than men which conforms to the result of our study. Different studies had reported the one-year prevalence of TTH among the population older than 50 years to be 16-44%.5,6 TTH is the commonest type of primary headache found in the elderly population7, which is in conformity to the results of our study. Several studies had reported regional variability in the prevalence of migraine,3 ranging from 1% to 22% in the continent of Asia. Our study found the one-year prevalence rate of migraine to be 28%, which is slightly higher than the reported range of prevalence stated in those studies. The present study reported the one-year prevalence rates of different psychiatric co-morbidities like bipolar mood disorder to be 10%, agoraphobia to be 1%, dysthymia to be 18%, generalized anxiety disorder to be 15%, major depressive disorder to be 48%, obsessive compulsive order to be 3%, panic disorder to be 3% and suicidality to be 2%. A similar study7 conducted in 2012 western India on a series of 101 patients of primary headache found prevalence rate of depressive disorders (dysthymia, major depression or suicidality) to be 48.5%. anxiety related disorders (generalized anxiety disorder, panic disorders, agoraphobia or social phobia) to be 17.9%, which is similar to our study (19%). Another study conducted by Martins V et al 8 reported the prevalence rate of mood disorders to be 62% and stress related neurotic disorders to be 39.2%. Major depressive disorder was the most prevalent mood disorder in that study (prevalence rate 33%) which is slightly less than the prevalence rate of major depressive disorders found in the present study. Another study conducted by Bera S .C.et al (2014)9 in a tertiary hospital in north India showed that psychiatric co-morbidity, especially depression is common in patients of migraine and tension type headache. The findings of the present study are in conformity to the above study.
CONCLUSION Primary headaches are often associated with different types of psychiatric co-morbidities, which are often overlooked, remain undiagnosed and untreated. Awareness of the different types of psychiatric co-morbidities with primary headache can help the patients to receive a better management by multidisciplinary approach.
REFERENCES
|
|
 Home
Home