Official Journals By StatPerson Publication
|
Table of Content Volume 13 Issue 2 - February 2020
Psychiatric morbidity in children of poly-substance abuser
Assistant Professor and Head of Department, Department of Psychiatry Government Medical college, Aurangabad, Maharashtra, India. Email: psdesh000@gmail.com
Abstract Background: It is an issue concern throughout the world about substance abuse and its effects on community, family. Research on children of drug users is based on the expectation that parental drug use has the potential to affect children's psychosocial development negatively in at least three main ways: first, by depriving them of adequate physical care; second, by impeding their socio-emotional and cognitive development; and third, by influencing them to become drug users themselves. Research on psychopathology among children of polysubstance abuser are limited. The substance seeking behaviour is increasing and the prevalence of problems related to them are growing in the Indian context. So, there is a need to do more research into this aspect. Aims and Objectives: To asses psychopathology among children of polysubstance abuser. Materials and method: It was a cross-sectional study. 30 (6 to 18 years old) children of patients with polysubstance abuse were enrolled in study. All the subjects recruited from psychiatry IPD and OPD service in Government medical college, Aurangabad, Maharashtra, India. The subjects were interviewed by interviewer conducting the study. Results: In total study sample 4 children each were of 7 years, 10 years, 11 years and 12 years of age. 6 children each were of 8 and 9 years of age and 2 children were of 13 years of age. 14 (46.67%) were male and 16 (53.34%) were female. 12 (40%) children were living in nuclear family and 18 (60%) children in joint family. Psychopathology seen in children in the form of the internalizing problems and externalizing problems. Among the internalizing problems seen in children anxiety was most common followed by depression and somatic complaints. In externalizing problems aggression and rule breaking were equally common. In externalizing problems 2 children have problems in borderline range and none in clinical range. Both the children in borderline range were male. Conclusion: psychopathology seen in children in the form of the internalizing problems and externalizing problems. Among the internalizing problems seen in children anxiety was most common followed by depression and somatic complaints. In externalizing problems aggression and rule breaking were equally common. Key Word: poly-substance abuser.
INTRODUCTION It is an issue concern throughout the world about substance abuse and its effects on community, family 1. Hazardous drinking was found in more than half of the alcohol drinkers in India which is emerging as a major public–health problem in the country2. In India, studies found that alcohol, cannabis, heroin and opium were the common drugs of abuse. The national household survey (2004) of drug use in the country found that alcohol was the most commonly used substance with prevalence of 21.4 %, followed by cannabis 3 % and opioid 0.7 %. The adverse effect of drug use on families is very large. Drug use is associated with domestic violence, risk of physical and emotional distress among family members 4. Large quantity consumption can cause long–term effects in the children5. To study effect of substance abuse in family is necessary because family members are at high risk6,8. In recent times substance abuse is increasing fast in society. More people are becoming drug abuser 9. The children of parents with substance use disorder as compared with reference children have greater liability for psychopathology. Emotional and behavioural problems in children of drug-dependent parents have been proven in several studies 10,14. Studies have reported increase in psychopathology among these children which include conduct disorder, attention deficit hyperactivity disorder (ADHD), major depressive disorder, and anxiety disorders15,18. Therefore, such children and their families have considered “high risk” 19. A person with poly-substance dependence is psychologically addicted to being in an intoxicated state without a preference for one particular substance20. According to the DSM-IV, a diagnosis of poly-substance dependence must include a person who has used at least three different substances (not including caffeine or nicotine) indiscriminately, but does not have a preference to any specific one. Study suggested that the number of new cases of poly-substance dependence has been going 21. Data from the government treatment centres (GOs) supported by the Ministry of Health and Family Welfare (MOHFW) showed that, 4.7 percent were dependent on multiple drugs. Research on children of drug users is based on the expectation that parental drug use has the potential to affect children's psychosocial development negatively in at least three main ways: first, by depriving them of adequate physical care; second, by impeding their socio-emotional and cognitive development; and third, by influencing them to become drug users themselves. A predictable, consistent environment, coupled with positive caregiver relationships, is critical for normal emotional development of children. Parental substance abuse and dependence have a negative impact on the physical and emotional well-being of children and can cause home environments to become disordered and unpredictable, leading to child maltreatment. The children's physical and emotional needs often becomes less important to their parents' activities related to obtaining, using, or recovering from the use of drugs and alcohol22. Research on psychopathology among children of polysubstance abuser are limited. The substance seeking behaviour is increasing and the prevalence of problems related to them are growing in the Indian context. So, there is a need to do more research into this aspect. AIMS AND OBJECTIVE To asses psychopathology among children of polysubstance abuser.
MATERIALS AND METHOD’S It was a cross-sectional study. 30 (6 to 18 years old) children of patients with polysubstance abuse were enrolled in study. All the subjects recruited from psychiatry IPD and OPD service in tertiary care hospital, after obtaining necessary permission and ethical clearance from the relevant authorities. The subjects were interviewed by interviewer conducting the study. The interview consisted of semi structured pro-forma which included socio-demographic data. one of the parent were asked question about psychopathology in their children. The data was then organized and analysed qualitatively as well as quantitatively by ratification on scales to gauge whether and how much they were in accordance with the aims and objectives of this study. TOOLS USED Socio demographic data sheet- The socio demographic data sheet will consist of information related to age, sex ,religion ,marital status ,education ,occupation ,income ,domicile ,type of family and duration of substance intake in partner. Child behavior checklist (CBCL/6-18) 23 The Child Behaviour Checklist (CBCL) for ages 6 – 18 years is a device by which parents or other individuals who know the child well, rate a child's behavioural problems and competencies. This instrument can either be self-administered or through an interview. It consists of 120 items on behaviour or emotional problems. Scoring is done as 0 for not true, 1 for somewhat or sometimes true, 2 for very true or often true. Questions create three types of behaviour scales: 1.Internalizing scales - depression/withdrawal, anxiety and somatic symptoms 2. Externalizing scales - cruel, aggressive, and delinquent behaviours 3.Total problems includes sum total of internalizing, externalizing along with social problems, thought problems, attention problems and other problems which were not included in above listed. For scoring purpose Syndrome scales for boys and girls were used to find ‘T’ scores for that Age and sex. Behavioral problems were thus classified into Normal, Borderline or Clinical range from syndrome scale graphs for Boys and Girls. The range of Test-Retest Value is 0.95 to 1.00. Inter-rater reliability is 0.93 to 0.96, and range of Internal consistency 0.78 to 0.97. Criterion validity was assessed and found to be acceptable. Time to administer is 15 min. Psychopathology in children
RESULTS 1. Socio-demographic profile of children a. Age
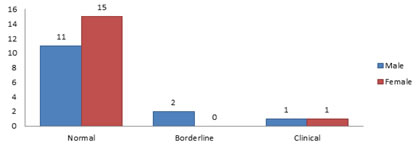
In total study sample 4 children each were of 7 years, 10 years, 11 years and 12 years of age. 6 children each were of 8 and 9 years of age and 2 children were of 13 years of age b. Gender Figure -10: gender distribution of total study sample In the total study sample 14 (46.67%) were male and 16 (53.34%) were female c. Type of family Figure-11: Distribution of total study sample as per type of family In the total study participants 12 (40%) children were living in nuclear family and 18 (60%) children in joint family 2. Psychopathology in children a. Internalizing problems
Figure 12: Distribution of internalizing problems in children
2 children have internalizing problems in borderline range and 2 in clinical range Both children in borderline range were male and in clinical range 1 was male other was female I. Internalizing problems in clinical range
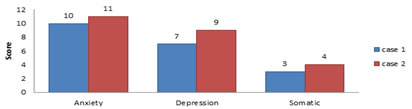
Figure 13: Distribution of internalizing problems in clinical range
II. Internalizing problems in borderline range
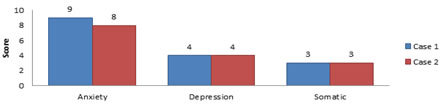
Figure 14: Distribution of internalizing problems in borderline range
In internalizing problems, anxiety was more common in both clinical and borderline range. Anxiety was followed by depression and somatic complaints (ref to figure 13 and 14)
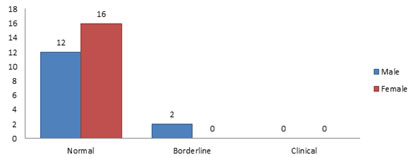
b. Externalizing problems Figure 15: Distribution of externalizing problems in children
In externalizing problems 2 children have problems in borderline range and none in clinical range. Both the children in borderline range were male
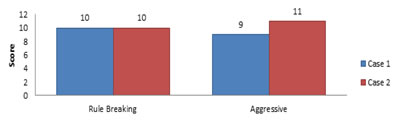
Externalizing problems in borderline range Figure 16: Distribution of Externalizing problems in borderline range
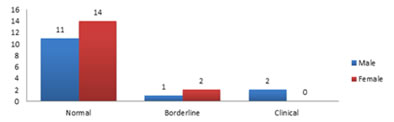
In externalizing problems, borderline range aggression was nearly equal to the rule breaking problems c. Total problems Figure-17: Distribution of total problems in children 5 children had total problems, 1 male and 2 female in borderline range And 2 male in clinical range
Table 16: Distribution of total problems according to CBCL in the 5 children
Out of 5 children who had total problems, 2 were in clinical range (T score 71) and 3 were in borderline range (T score= 66, 67 and 65).In those who were in clinical range other problems were common followed by aggressive behaviour and thought problems. 2 children (case 1 and case 3) who had problems in borderline range scores were highest on anxious/depressed domain followed by withdrawn/depressed. And in the remaining one thought problems and other problems like overeating, overweight, sleeps more, talks too much etc. were common.
DISCUSSION Substance related disorders are matters of global concern because of effect on individual health, family, society, criminal and legal problems. It has huge impact on family. So, family members are considered to be at high risk to develop mental disorder. This study was carried out to see if there is any psychopathology present in children of polysubstance abuser. Further it also intended to know if there is any difference in psychopathology depending on demographic factors.The inferences drawn out of the results obtained from the analysis of the data are as follows: A. Socio demographic description of the participants Age of the children was between 7 to 13 years. Among the children 14 were male and 16 were female. 60% children belonged to joint family and 40% to nuclear family. Psychopathology in children The children of parents with substance use disorder as compared with reference children have greater liability for psychopathology. Studies have reported increase in mental disorders among these children which include conduct disorder, attention deficit hyperactivity disorder (ADHD), major depressive disorder, and anxiety disorders 15,18. In our study sample internalizing problems were seen in 4 children, externalizing in 2 and total problem in 5 children. Study on children of alcoholics demonstrated associations between paternal alcoholism and externalizing and internalizing behaviour problems 24. Children of opiate-dependent parents had significantly higher levels of internalising and externalising behaviours on the Child Behavior Checklist. 25 We found that the anxiety was seen to be more common among internalizing problems in children, followed by depression and somatic complaints in both clinical and borderline range. Johnson, et al. (1991) also found evidence that, children of drug users are at higher risk for symptoms of depression and trait anxiety than children of non-drug users, based on the Children's Depression Inventory and the How I Feel Questionnaire, although children did not meet the criteria for clinical diagnoses 26. One more study reported that among the psychological difficulties seen in children of parents with substance use problems, the anxiety disorders are among the most chronic conditions. 27. The externalizing problems seen in our study were aggression and rule breaking problems. Loukas A, et al. examined trajectories of disruptive behavior from preschool to early adolescence among sons of alcoholic and non-alcoholic parents. He found sons of alcoholic fathers were consistently higher in disruptive behavior than were sons of non-alcoholic and this association remained after controlling for maternal alcohol problems, family conflict, and child temperament 28.
CONCLUSION It is known that psychological problems in children of substance abuser are common. In our study, psychopathology seen in children in the form of the internalizing problems and externalizing problems. Among the internalizing problems seen in children anxiety was most common followed by depression and somatic complaints. In externalizing problems aggression and rule breaking were equally common.
REFERENCES
Policy for Articles with Open Access |
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home